Medicine:Pseudomonas infection
| Pseudomonas infection | |
|---|---|
| Other names | pseudomoniasis; pseudomonosis |
 | |
| Prognosis | 18-61CFR |

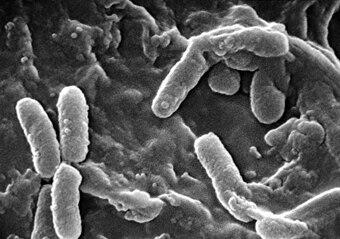
Pseudomonas infection refers to a disease caused by one of the species of the genus Pseudomonas.
P. aeruginosa is a germ found in the environment it is an opportunistic human pathogen most commonly infecting immunocompromised patients, such as those with cancer ,diabetes, cystic fibrosis,[1] severe burns, AIDS,[2] or people who are very young or elderly. Infection can affect many parts of the body, but infections typically target the respiratory tract, the renal system, the gastrointestinal system or it can cause blood infection, the symptoms include bacterial pneumonia, severe coughing, congestion, UTI, pain in the ears and eyes, joint pain, neck or back pain, headache, diarrhea, a rash which can include pimples filled with pus, swelling in the eyes. Complications include pneumonia, gangrene, necrotizing fasciitis, compartment syndrome, necrosis, and loss of an extremity, Septicemia may lead to septic shock and death. In a surveillance study between 1986 and 1989, P. aeruginosa was the third leading cause of all nosocomial infections, and specifically the number one leading cause of hospital-acquired pneumonia and third leading cause of hospital-acquired UTI.[3] Treatment of such infections can be difficult due to multiple antibiotic resistance,[4] and in the United States, there was an increase in MDRPA (Multidrug-resistant Pseudomonas aeruginosa) resistant to ceftazidime, ciprofloxacin, and aminoglycosides, from 0.9% in 1994 to 5.6% in 2002.[5]
P. oryzihabitans can also be a human pathogen, although infections are rare. It can cause peritonitis,[6] endophthalmitis,[7] sepsis and bacteremia. Similar symptoms although also very rare can be seen by infections of P. luteola.[8]
P. plecoglossicida is a fish pathogenic species, causing hemorrhagic ascites in the ayu (Plecoglossus altivelis).[9] P. anguilliseptica is also a fish pathogen.[10]
Due to their hemolytic activity, even non-pathogenic species of Pseudomonas can occasionally become a problem in clinical settings, where they have been known to infect blood transfusions.[11]
See also
References
- ↑ "Pseudomonal infection in cystic fibrosis: the battle continues". Expert Review of Anti-infective Therapy 1 (4): 609–18. 2003. doi:10.1586/14787210.1.4.609. PMID 15482158.
- ↑ Shanson DC (1990). "Septicaemia in patients with AIDS". Trans. R. Soc. Trop. Med. Hyg. 84 Suppl 1: 14–6. doi:10.1016/0035-9203(90)90449-o. PMID 2201108.
- ↑ Schaberd; Culver; Gaynes (1991). "Major trends in the microbial etiology of nosocomial infection". The American Journal of Medicine 91 (3): S72–S75. doi:10.1016/0002-9343(91)90346-Y. PMID 1928195. https://deepblue.lib.umich.edu/bitstream/2027.42/29131/1/0000170.pdf.
- ↑ McGowan JE (2006). "Resistance in nonfermenting gram-negative bacteria: multidrug resistance to the maximum". Am. J. Med. 119 (6 Suppl 1): S29–36; discussion S62–70. doi:10.1016/j.amjmed.2006.03.014. PMID 16735148.
- ↑ Obritsch; Fish; MacLauren; Jung (2005). "Nosocomial Infections Due to Multidrug-Resistant Pseudomonas aeruginosa: Epidemiology and Treatment Options". Pharmacotherapy 25 (10): 1353–1364. doi:10.1592/phco.2005.25.10.1353. PMID 16185180.
- ↑ "Peritonitis with multiple rare environmental bacteria in a patient receiving long-term peritoneal dialysis". Am. J. Kidney Dis. 46 (6): e119–24. 2005. doi:10.1053/j.ajkd.2005.08.021. PMID 16310563.
- ↑ "Chronic postoperative endophthalmitis due to Pseudomonas oryzihabitans". Am. J. Ophthalmol. 134 (4): 613–4. 2002. doi:10.1016/S0002-9394(02)01586-6. PMID 12383826.
- ↑ "Two new species of Pseudomonas: P. oryzihabitans isolated from rice paddy and clinical specimens and P. luteola isolated from clinical specimens". Int J Syst Bacteriol 35 (Pt 2): 467–74. 1985. doi:10.1099/00207713-35-4-467.
- ↑ "Pseudomonas plecoglossicida sp. nov., the causative agent of bacterial haemorrhagic ascites of ayu, Plecoglossus altivelis". Int. J. Syst. Evol. Microbiol. 50 (1): 83–9. 2000. doi:10.1099/00207713-50-1-83. PMID 10826790.
- ↑ "Existence of two O-serotypes in the fish pathogen Pseudomonas anguilliseptica". Vet. Microbiol. 94 (4): 325–33. 2003. doi:10.1016/S0378-1135(03)00124-X. PMID 12829386.
- ↑ "Pseudomonas fluorescens bacteremia from blood transfusion". Am. J. Med. 76 (1): 62–8. 1984. doi:10.1016/0002-9343(84)90751-4. PMID 6419604.
External links
| Classification |
|---|

