Medicine:Candidiasis
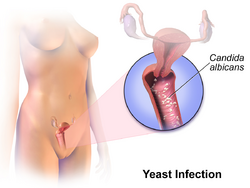
Candidiasis is a fungal infection due to any species of the genus Candida (a yeast).[1] When it affects the mouth, in some countries it is commonly called thrush.[2] Signs and symptoms include white patches on the tongue or other areas of the mouth and throat.[2] Other symptoms may include soreness and problems swallowing.[3] When it affects the vagina, it may be referred to as a yeast infection or thrush.[4][5] Signs and symptoms include genital itching, burning, and sometimes a white "cottage cheese-like" discharge from the vagina.[6] Yeast infections of the penis are less common and typically present with an itchy rash.[6] Very rarely, yeast infections may become invasive, spreading to other parts of the body.[7] This may result in fevers, among other symptoms.[7] Finally, candidiasis of the esophagus is an important risk factor for contracting esophageal cancer in individuals with achalasia.[8]
More than 20 types of Candida may cause infection with Candida albicans being the most common.[9] Infections of the mouth are most common among children less than one month old, the elderly, and those with weak immune systems.[10] Conditions that result in a weak immune system include HIV/AIDS, the medications used after organ transplantation, diabetes, and the use of corticosteroids.[10] Other risk factors include during breastfeeding, following antibiotic therapy, and the wearing of dentures.[10][11] Vaginal infections occur more commonly during pregnancy, in those with weak immune systems, and following antibiotic therapy.[12] Individuals at risk for invasive candidiasis include low birth weight babies, people recovering from surgery, people admitted to intensive care units, and those with an otherwise compromised immune system.[13]
Efforts to prevent infections of the mouth include the use of chlorhexidine mouthwash in those with poor immune function and washing out the mouth following the use of inhaled steroids.[14] Little evidence supports probiotics for either prevention or treatment, even among those with frequent vaginal infections.[15][16] For infections of the mouth, treatment with topical clotrimazole or nystatin is usually effective.[14] Oral or intravenous fluconazole, itraconazole, or amphotericin B may be used if these do not work.[14] A number of topical antifungal medications may be used for vaginal infections, including clotrimazole.[17] In those with widespread disease, an echinocandin such as caspofungin or micafungin is used.[18] A number of weeks of intravenous amphotericin B may be used as an alternative.[18] In certain groups at very high risk, antifungal medications may be used preventively,[13][18] and concomitantly with medications known to precipitate infections.
Infections of the mouth occur in about 6% of babies less than a month old.[19] About 20% of those receiving chemotherapy for cancer and 20% of those with AIDS also develop the disease.[19] About three-quarters of women have at least one yeast infection at some time during their lives.[20] Widespread disease is rare except in those who have risk factors.[21]
Signs and symptoms


Signs and symptoms of candidiasis vary depending on the area affected.[22] Most candidal infections result in minimal complications such as redness, itching, and discomfort, though complications may be severe or even fatal if left untreated in certain populations. In healthy (immunocompetent) persons, candidiasis is usually a localized infection of the skin, fingernails or toenails (onychomycosis), or mucosal membranes, including the oral cavity and pharynx (thrush), esophagus, and the sex organs (vagina, penis, etc.);[23][24][25] less commonly in healthy individuals, the gastrointestinal tract,[26][27][28] urinary tract,[26] and respiratory tract[26] are sites of candida infection.
In immunocompromised individuals, Candida infections in the esophagus occur more frequently than in healthy individuals and have a higher potential of becoming systemic, causing a much more serious condition, a fungemia called candidemia.[23][29][30] Symptoms of esophageal candidiasis include difficulty swallowing, painful swallowing, abdominal pain, nausea, and vomiting.[23][31]
Mouth
Infection in the mouth is characterized by white discolorations in the tongue, around the mouth, and in the throat. Irritation may also occur, causing discomfort when swallowing.[32]
Thrush is commonly seen in infants. It is not considered abnormal in infants unless it lasts longer than a few weeks.[33]
Genitals
Infection of the vagina or vulva may cause severe itching, burning, soreness, irritation, and a whitish or whitish-gray cottage cheese-like discharge. Symptoms of infection of the male genitalia (balanitis thrush) include red skin around the head of the penis, swelling, irritation, itchiness and soreness of the head of the penis, thick, lumpy discharge under the foreskin, unpleasant odour, difficulty retracting the foreskin (phimosis), and pain when passing urine or during sex.[34]
Skin
Signs and symptoms of candidiasis in the skin include itching, irritation, and chafing or broken skin.[35]
Invasive infection
Common symptoms of gastrointestinal candidiasis in healthy individuals are anal itching, belching, bloating, indigestion, nausea, diarrhea, gas, intestinal cramps, vomiting, and gastric ulcers.[26][27][28] Perianal candidiasis can cause anal itching; the lesion can be red, papular, or ulcerative in appearance, and it is not considered to be a sexually transmitted infection.[36] Abnormal proliferation of the candida in the gut may lead to dysbiosis.[37] While it is not yet clear, this alteration may be the source of symptoms generally described as the irritable bowel syndrome,[38][39] and other gastrointestinal diseases.[27][40]
Neurological symptoms
Systemic candidiasis can affect the central nervous system, causing a variety of neurological symptoms, with a presentation similar to meningitis.
Causes
Candida yeasts are generally present in healthy humans, frequently part of the human body's normal oral and intestinal flora, and particularly on the skin; however, their growth is normally limited by the human immune system and by competition of other microorganisms, such as bacteria occupying the same locations in the human body.[41] Candida requires moisture for growth, notably on the skin.[42] For example, wearing wet swimwear for long periods of time is believed to be a risk factor.[43] Candida can also cause diaper rashes in babies.[35] In extreme cases, superficial infections of the skin or mucous membranes may enter the bloodstream and cause systemic Candida infections.[44]
Factors that increase the risk of candidiasis include HIV/AIDS, mononucleosis, cancer treatments, steroids, stress, antibiotic therapy, diabetes, and nutrient deficiency. Hormone replacement therapy and infertility treatments may also be predisposing factors.[45] Use of inhaled corticosteroids increases risk of candidiasis of the mouth.[46] Inhaled corticosteroids with other risk factors such as antibiotics, oral glucocorticoids, not rinsing mouth after use of inhaled corticosteroids or high dose of inhaled corticosteroids put people at even higher risk.[46] Treatment with antibiotics can lead to eliminating the yeast's natural competitors for resources in the oral and intestinal flora, thereby increasing the severity of the condition.[47] A weakened or undeveloped immune system or metabolic illnesses are significant predisposing factors of candidiasis.[48] Almost 15% of people with weakened immune systems develop a systemic illness caused by Candida species.[49] Diets high in simple carbohydrates have been found to affect rates of oral candidiases.[50]
C. albicans was isolated from the vaginas of 19% of apparently healthy women, i.e., those who experienced few or no symptoms of infection. External use of detergents or douches or internal disturbances (hormonal or physiological) can perturb the normal vaginal flora, consisting of lactic acid bacteria, such as lactobacilli, and result in an overgrowth of Candida cells, causing symptoms of infection, such as local inflammation.[51] Pregnancy and the use of oral contraceptives have been reported as risk factors.[52] Diabetes mellitus and the use of antibiotics are also linked to increased rates of yeast infections.[52]
In penile candidiasis, the causes include sexual intercourse with an infected individual, low immunity, antibiotics, and diabetes. Male genital yeast infections are less common, but a yeast infection on the penis caused by direct contact via sexual intercourse with an infected partner is not uncommon.[53]
Breastfeeding mothers may develop candidiasis on and around the nipple due to the moisture created by excessive milk production.[11]
Vaginal candidiasis can cause congenital candidiasis in newborns.[54]
Diagnosis




In oral candidiasis, simply inspecting the person's mouth for white patches and irritation may make the diagnosis. A sample of the infected area may also be taken to determine what organism is causing the infection.[55]
Symptoms of vaginal candidiasis are also present in the more common bacterial vaginosis;[56] aerobic vaginitis is distinct and should be excluded in the differential diagnosis.[57] In a 2002 study, only 33% of women who were self-treating for a yeast infection were found to have such an infection, while most had either bacterial vaginosis or a mixed-type infection.[58]
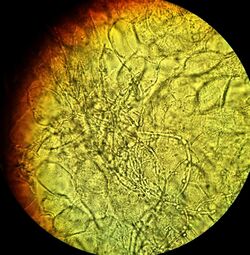
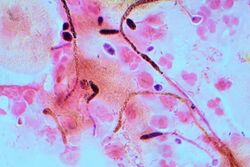
Diagnosis of a yeast infection is confirmed either via microscopic examination or culturing. For identification by light microscopy, a scraping or swab of the affected area is placed on a microscope slide. A single drop of 10% potassium hydroxide (KOH) solution is then added to the specimen. The KOH dissolves the skin cells, but leaves the Candida cells intact, permitting visualization of pseudohyphae and budding yeast cells typical of many Candida species.[59]
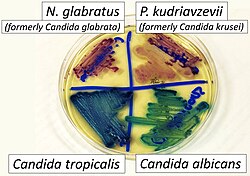
For the culturing method, a sterile swab is rubbed on the infected skin surface. The swab is then streaked on a culture medium. The culture is incubated at 37 °C (98.6 °F) for several days, allowing development of yeast or bacterial colonies. The characteristics (such as morphology and color) of the colonies may allow initial diagnosis of the organism causing disease symptoms.[60] Respiratory, gastrointestinal, and esophageal candidiasis require an endoscopy to diagnose.[28][61] For gastrointestinal candidiasis, it is necessary to obtain a 3–5 milliliter sample of fluid from the duodenum for fungal culture.[28] The diagnosis of gastrointestinal candidiasis is based upon the culture containing exceeding 1,000 colony-forming units per milliliter.[28]
Classification
Candidiasis may be divided into these types:
- Mucosal candidiasis
- Oral candidiasis (thrush, oropharyngeal candidiasis)[23][25]
- Pseudomembranous candidiasis[25]
- Erythematous candidiasis[23][25]
- Hyperplastic candidiasis[25]
- Denture-related stomatitis[23][25] — Candida organisms are involved in about 90% of cases
- Angular cheilitis[23][25] — Candida species are responsible for about 20% of cases, mixed infection of C. albicans and Staphylococcus aureus for about 60% of cases.
- Median rhomboid glossitis[25]
- Candidal vulvovaginitis (vaginal yeast infection)[23][62]
- Candidal balanitis — infection of the glans penis,[23] almost exclusively occurring in uncircumcised males[63]
- Esophageal candidiasis (candidal esophagitis)[23][31]
- Gastrointestinal candidiasis[26][27][28]
- Respiratory candidiasis[23][26]
- Oral candidiasis (thrush, oropharyngeal candidiasis)[23][25]
- Cutaneous candidiasis
- Candidal folliculitis[23]
- Candidal intertrigo[23]
- Candidal paronychia[23]
- Perianal candidiasis, may present as pruritus ani[64]: 309
- Candidid
- Chronic mucocutaneous candidiasis[23]
- Congenital cutaneous candidiasis[54]
- Diaper candidiasis: an infection of a child's diaper area[64]: 309
- Erosio interdigitalis blastomycetica
- Candidal onychomycosis (nail infection) caused by Candida[23][65]
- Systemic candidiasis[23]
- Antibiotic candidiasis (iatrogenic candidiasis)
Prevention
A diet that supports the immune system and is low in simple carbohydrates contributes to a healthy balance of the oral and intestinal flora.[41][50] While yeast infections are associated with diabetes, the level of blood sugar control may not affect the risk.[67] Wearing cotton underwear may help to reduce the risk of developing skin and vaginal yeast infections, along with not wearing wet clothes for long periods.[12][43] For women who experience recurrent yeast infections, there is limited evidence that oral or intravaginal probiotics help to prevent future infections.[15][68] This includes either as pills or as yogurt.[15]
Oral hygiene can help prevent oral candidiasis when people have a weakened immune system.[10] For people undergoing cancer treatment, chlorhexidine mouthwash can prevent or reduce thrush.[10] People who use inhaled corticosteroids can reduce the risk of developing oral candidiasis by rinsing the mouth with water or mouthwash after using the inhaler.[10] People with dentures should also disinfect their dentures regularly to prevent oral candidiasis.[55]
Treatment
Candidiasis is treated with antifungal medications; these include clotrimazole, nystatin, fluconazole, voriconazole, amphotericin B, and echinocandins.[18] Intravenous fluconazole or an intravenous echinocandin such as caspofungin are commonly used to treat immunocompromised or critically ill individuals.[18]
The 2016 revision of the clinical practice guideline for the management of candidiasis lists a large number of specific treatment regimens for Candida infections that involve different Candida species, forms of antifungal drug resistance, immune statuses, and infection localization and severity.[18] Gastrointestinal candidiasis in immunocompetent individuals is treated with 100–200 mg fluconazole per day for 2–3 weeks.[28]
Localized infection
Mouth and throat candidiasis are treated with antifungal medication. Oral candidiasis usually responds to topical treatments; otherwise, systemic antifungal medication may be indicated for oral infections. Candidal skin infections in the skin folds (candidal intertrigo) typically respond well to topical antifungal treatments (e.g., nystatin or miconazole). For breastfeeding mothers, topical miconazole is the most effective treatment for treating candidiasis on the breasts.[69] Gentian violet can be used for thrush in breastfeeding babies.[11] Systemic treatment with antifungals by mouth is reserved for severe cases or if treatment with topical therapy is unsuccessful. Candida esophagitis may be treated orally or intravenously. For severe or azole-resistant esophageal candidiasis, treatment with amphotericin B may be necessary.[14]
Vaginal yeast infections are typically treated with topical antifungal agents.[18] Penile yeast infections are also treated with antifungal agents, but while an internal treatment may be used (such as a pessary) for vaginal yeast infections, only external treatments – such as a cream – can be recommended for penile treatment.[70] A one-time dose of fluconazole by mouth is 90% effective in treating a vaginal yeast infection.[71] For severe nonrecurring cases, several doses of fluconazole is recommended.[18] Local treatment may include vaginal suppositories or medicated douches. Other types of yeast infections require different dosing. C. albicans can develop resistance to fluconazole, this being more of an issue in those with HIV/AIDS who are often treated with multiple courses of fluconazole for recurrent oral infections.[72]
For vaginal yeast infection in pregnancy, topical imidazole or triazole antifungals are considered the therapy of choice owing to available safety data.[73] Systemic absorption of these topical formulations is minimal, posing little risk of transplacental transfer.[73] In vaginal yeast infection in pregnancy, treatment with topical azole antifungals is recommended for seven days instead of a shorter duration.[73]
For vaginal yeast infections, many complementary treatments are proposed; however, several have side effects.[74] No benefit from probiotics has been found for active infections.[16]
Blood-borne infection
Candidemia occurs when any Candida species infects the blood. Its treatment typically consists of oral or intravenous antifungal medications.[75] Examples include intravenous fluconazole or an echinocandin such as caspofungin may be used.[18] Amphotericin B is another option.[18]
Prognosis
In hospitalized patients who develop candidemia, age is an important prognostic factor. Mortality following candidemia is 50% in patients aged ≥75 years and 24% in patients aged <75 years.[76] Among individuals being treated in intensive care units, the mortality rate is about 30–50% when systemic candidiasis develops.[77]
Epidemiology
Oral candidiasis is the most common fungal infection of the mouth,[78] and it also represents the most common opportunistic oral infection in humans.[79] Infections of the mouth occur in about 6% of babies less than a month old.[19] About 20% of those receiving chemotherapy for cancer and 20% of those with AIDS also develop the disease.[19]
It is estimated that 20% of women may be asymptomatically colonized by vaginal yeast.[80] In the United States there are approximately 1.4 million doctor office visits every year for candidiasis.[81] About three-quarters of women have at least one yeast infection at some time during their lives.[20]
Esophageal candidiasis is the most common esophageal infection in persons with AIDS and accounts for about 50% of all esophageal infections, often coexisting with other esophageal diseases. About two-thirds of people with AIDS and esophageal candidiasis also have oral candidiasis.[31]
Candidal sepsis is rare.[82] Candida is the fourth most common cause of bloodstream infections among hospital patients in the United States.[83] The incidence of bloodstream candida in intensive care units varies widely between countries.[84]
History
Descriptions of what sounds like oral thrush go back to the time of Hippocrates circa 460–370 BCE.[22]
The first description of a fungus as the causative agent of an oropharyngeal and oesophageal candidosis was by Bernhard von Langenbeck in 1839.[85]
Vulvovaginal candidiasis was first described in 1849 by Wilkinson.[86] In 1875, Haussmann demonstrated that the causative organism in both vulvovaginal and oral candidiasis is the same.[86]
With the advent of antibiotics following World War II, the rates of candidiasis increased. The rates then decreased in the 1950s following the development of nystatin.[87]
The colloquial term "thrush" is of unknown origin but may stem from an unrecorded Old English word *þrusc or a Scandinavian root. The term is not related to the bird of the same name.[88] The term candidosis is largely used in British English, and candidiasis in American English.[86] Candida is also pronounced differently; in American English, the stress is on the "i", whereas in British English the stress is on the first syllable.[86]
The genus Candida and species C. albicans were described by botanist Christine Marie Berkhout in her doctoral thesis at the University of Utrecht in 1923. Over the years, the classification of the genera and species has evolved. Obsolete names for this genus include Mycotorula and Torulopsis. The species has also been known in the past as Monilia albicans and Oidium albicans. The current classification is nomen conservandum, which means the name is authorized for use by the International Botanical Congress (IBC).[89]
The genus Candida includes about 150 different species. However, only a few are known to cause human infections. C. albicans is the most significant pathogenic species. Other species pathogenic in humans include C. auris, C. tropicalis, C. parapsilosis, C. dubliniensis, and C. lusitaniae.
The name Candida was proposed by Berkhout. It is from the Latin word toga candida, referring to the white toga (robe) worn by candidates for the Senate of the ancient Roman republic.[86] The specific epithet albicans also comes from Latin, albicare meaning "to whiten".[86] These names refer to the generally white appearance of Candida species when cultured.
Alternative medicine
A 2005 publication noted that "a large pseudoscientific cult"[90] has developed around the topic of Candida, with claims stating that up to one in three people are affected by yeast-related illness, particularly a condition called "Candidiasis hypersensitivity".[91] Some practitioners of alternative medicine have promoted these purported conditions and sold dietary supplements as supposed cures; a number of them have been prosecuted.[91][92] In 1990, alternative health vendor Nature's Way signed an FTC consent agreement not to misrepresent in advertising any self-diagnostic test concerning yeast conditions or to make any unsubstantiated representation concerning any food or supplement's ability to control yeast conditions, with a fine of $30,000 payable to the National Institutes of Health for research in genuine candidiasis.[92]
Research
High level Candida colonization is linked to several diseases of the gastrointestinal tract including Crohn's disease.[93][94]
There has been an increase in resistance to antifungals worldwide over the past 30–40 years.[95][96]
References
- ↑ "Candidiasis". United States: Centers for Disease Control and Prevention. 13 November 2019. https://www.cdc.gov/fungal/diseases/candidiasis/.
- ↑ 2.0 2.1 "Candida infections of the mouth, throat, and esophagus". United States: Centers for Disease Control and Prevention. 13 November 2019. https://www.cdc.gov/fungal/diseases/candidiasis/thrush/index.html.
- ↑ "Symptoms of Oral Candidiasis". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/thrush/symptoms.html.
- ↑ "Vaginal Candidiasis". United States: Centers for Disease Control and Prevention. 13 November 2019. https://www.cdc.gov/fungal/diseases/candidiasis/genital/index.html.
- ↑ "Thrush in men and women" (in en). 9 January 2018. https://www.nhs.uk/conditions/thrush-in-men-and-women/.
- ↑ 6.0 6.1 "Symptoms of Genital / Vulvovaginal Candidiasis". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/genital/symptoms.html.
- ↑ 7.0 7.1 "Symptoms of Invasive Candidiasis". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/invasive/symptoms.html.
- ↑ "Esophageal Candida Infection and Esophageal Cancer Risk in Patients With Achalasia.". JAMA Netw Open 8 (1): e2454685. January 2025. doi:10.1001/jamanetworkopen.2024.54685. PMID 39808429.
- ↑ "Candidiasis". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 "Risk & Prevention". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/thrush/risk-prevention.html.
- ↑ 11.0 11.1 11.2 "Conquering common breast-feeding problems". The Journal of Perinatal & Neonatal Nursing 22 (4): 267–74. 2008. doi:10.1097/01.JPN.0000341356.45446.23. PMID 19011490.
- ↑ 12.0 12.1 "People at Risk for Genital / Vulvovaginal Candidiasis". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/genital/risk-prevention.html.
- ↑ 13.0 13.1 "People at Risk for Invasive Candidiasis". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/invasive/risk-prevention.html.
- ↑ 14.0 14.1 14.2 14.3 "Treatment & Outcomes of Oral Candidiasis". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/thrush/treatment.html.
- ↑ 15.0 15.1 15.2 "Clinical inquiries. Can probiotics safely prevent recurrent vaginitis?". The Journal of Family Practice 61 (6): 357, 368. June 2012. PMID 22670239.
- ↑ 16.0 16.1 "The role of lactobacillus probiotics in the treatment or prevention of urogenital infections--a systematic review". Journal of Chemotherapy 21 (3): 243–52. June 2009. doi:10.1179/joc.2009.21.3.243. PMID 19567343.
- ↑ "Treatment & Outcomes of Genital / Vulvovaginal Candidiasis". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/genital/treatment.html.
- ↑ 18.00 18.01 18.02 18.03 18.04 18.05 18.06 18.07 18.08 18.09 "Executive Summary: Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America". Clinical Infectious Diseases 62 (4): 409–17. February 2016. doi:10.1093/cid/civ1194. PMID 26810419.
- ↑ 19.0 19.1 19.2 19.3 "Oral Candidiasis Statistics". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/thrush/statistics.html.
- ↑ 20.0 20.1 "Genital / vulvovaginal candidiasis (VVC)". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/genital/index.html.
- ↑ "Invasive Candidiasis Statistics". United States: Centers for Disease Control and Prevention. February 13, 2014. https://www.cdc.gov/fungal/diseases/candidiasis/invasive/statistics.html.
- ↑ 22.0 22.1 Dolin, Gerald L.; Mandell, John E.; Bennett, Raphael (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases (7th ed.). Philadelphia, PA: Churchill Livingstone/Elsevier. pp. Chapter 250. ISBN 978-0-443-06839-3.
- ↑ 23.00 23.01 23.02 23.03 23.04 23.05 23.06 23.07 23.08 23.09 23.10 23.11 23.12 23.13 23.14 23.15 23.16 23.17 23.18 23.19 "Candidiasis: Clinical Presentation". WebMD. 18 August 2015. http://emedicine.medscape.com/article/213853-clinical#showall.
- ↑ Baron S, ed (1996). "Deep Mycoses". Baron's Medical Microbiology (4th ed.). Univ of Texas Medical Branch. ISBN 978-0-9631172-1-2. https://www.ncbi.nlm.nih.gov/books/NBK7902/.
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 25.6 25.7 "Clinical Appearance of Oral Candida Infection and Therapeutic Strategies". Frontiers in Microbiology 6: 1391. December 2015. doi:10.3389/fmicb.2015.01391. PMID 26733948.
- ↑ 26.0 26.1 26.2 26.3 26.4 26.5 "Candidiasis: predisposing factors, prevention, diagnosis and alternative treatment". Mycopathologia 177 (5–6): 223–40. June 2014. doi:10.1007/s11046-014-9749-1. PMID 24789109. http://repositorium.sdum.uminho.pt/bitstream/1822/31482/1/document_17753_1.pdf. Retrieved 2019-09-24. "Candida species and other microorganisms are involved in this complicated fungal infection, but Candida albicans continues to be the most prevalent. Over the past two decades, an abnormal overgrowth in the gastrointestinal, urinary, and respiratory tracts has been observed, not only in immunocompromised patients but also related to nosocomial infections and even in healthy individuals. There is a wide variety of causal factors that contribute to yeast infection, which means that candidiasis is a good example of a multifactorial syndrome.".
- ↑ 27.0 27.1 27.2 27.3 "Review article: fungal microbiota and digestive diseases". Alimentary Pharmacology & Therapeutics 39 (8): 751–66. April 2014. doi:10.1111/apt.12665. PMID 24612332. "In addition, GI fungal infection is reported even among those patients with normal immune status. Digestive system-related fungal infections may be induced by both commensal opportunistic fungi and exogenous pathogenic fungi. The IFI in different GI sites has its special clinical features, which are often accompanied by various severe diseases. Although IFI associated with digestive diseases are less common, they can induce fatal outcomes due to less specificity of related symptoms, signs, endoscopic and imaging manifestations, and the poor treatment options. ... Candida sp. is also the most frequently identified species among patients with gastric IFI. ... Gastric IFI is often characterised by abdominal pain and vomiting, and with the endoscopic characteristics including gastric giant and multiple ulcers, stenosis, perforation, and fistula. For example, gastric ulcers combined with entogastric fungal infection, characterised by deep, large, and intractable ulcers [118], were reported as early as the 1930s. ... The overgrowth and colonisation of fungi in the intestine can lead to diarrhea.".
- ↑ 28.0 28.1 28.2 28.3 28.4 28.5 28.6 "Small intestinal fungal overgrowth". Current Gastroenterology Reports 17 (4). April 2015. doi:10.1007/s11894-015-0436-2. PMID 25786900. "Small intestinal fungal overgrowth (SIFO) is characterized by the presence of excessive number of fungal organisms in the small intestine associated with gastrointestinal (GI) symptoms. Candidiasis is known to cause GI symptoms, particularly in immunocompromised patients or those receiving steroids or antibiotics. However, only recently, there has been emerging literature that an overgrowth of fungus in the small intestine of non-immunocompromised subjects may cause unexplained GI symptoms. Two recent studies showed that 26 % (24/94) and 25.3 % (38/150) of a series of patients with unexplained GI symptoms had SIFO. The most common symptoms observed in these patients were belching, bloating, indigestion, nausea, diarrhea, and gas. The underlying mechanism(s) that predispose to SIFO are unclear, but small intestinal dysmotility and the use of proton pump inhibitors have been implicated. However, further studies are needed; both to confirm these observations and to examine the clinical relevance of fungal overgrowth, both in healthy subjects and in patients with otherwise unexplained GI symptoms. ... For routine SIFO in an immunocompetent host, a 2–3 week oral course of fluconazole 100–200 mg will suffice.".
- ↑ "Immunity to Candida". Oral Diseases 8 (Suppl 2): 69–75. 2002. doi:10.1034/j.1601-0825.2002.00015.x. PMID 12164664.
- ↑ "Invasive candidiasis". Infectious Disease Clinics of North America 20 (3): 485–506. September 2006. doi:10.1016/j.idc.2006.07.004. PMID 16984866.
- ↑ 31.0 31.1 31.2 Textbook of gastroenterology (5th ed.). Chichester, West Sussex: Blackwell Pub.. 2009. p. 814. ISBN 978-1-4051-6911-0.
- ↑ "Candida infections of the mouth, throat, and esophagus | Fungal Diseases | CDC". 2019-04-17. https://www.cdc.gov/fungal/diseases/candidiasis/thrush/index.html.
- ↑ "Thrush". 2011. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001650/.
- ↑ NHS: Symptoms of thrush in men (balanitis thrush)
- ↑ 35.0 35.1 "Candida infection of the skin: MedlinePlus Medical Encyclopedia" (in en). https://medlineplus.gov/ency/article/000880.htm.
- ↑ Wolff, Bruce G., ed (2007). The ASCRS textbook of colon and rectal surgery. New York: Springer. pp. 241, 242, 245. ISBN 978-0-387-24846-2.
- ↑ "Mycobiota in gastrointestinal diseases". Nature Reviews. Gastroenterology & Hepatology 12 (2): 77–87. February 2015. doi:10.1038/nrgastro.2014.188. PMID 25385227.
- ↑ "Yeast metabolic products, yeast antigens and yeasts as possible triggers for irritable bowel syndrome". European Journal of Gastroenterology & Hepatology 17 (1): 21–6. January 2005. doi:10.1097/00042737-200501000-00005. PMID 15647635. http://www.jptwellnesscircle.com/teleseminars/DrSantelmannCandida.pdf. Retrieved 2017-10-24.
- ↑ "A role for the gut microbiota in IBS". Nature Reviews. Gastroenterology & Hepatology 11 (8): 497–505. August 2014. doi:10.1038/nrgastro.2014.40. PMID 24751910.
- ↑ "Digestive tract mycobiota: a source of infection". Médecine et Maladies Infectieuses 45 (1–2): 9–16. 2015. doi:10.1016/j.medmal.2015.01.007. PMID 25684583.
- ↑ 41.0 41.1 Primary Care Medicine: office evaluation and management of the adult patient. Philadelphia: Wolters Kluwer Health. 2006. pp. 802–3. ISBN 978-0-7817-7456-7. https://books.google.com/books?id=aWQhTbwoM9EC&pg=RA1-PA802. Retrieved 2008-11-23.
- ↑ Goehring, Richard V. (2008). Mims' medical microbiology. (4th ed.). Philadelphia, PA: Mosby Elsevier. p. 656. ISBN 978-0-323-04475-2.
- ↑ 43.0 43.1 MedlinePlus Encyclopedia Vaginal yeast infection
- ↑ Spampinato, Claudia; Leonardi, Darío (2013). "CandidaInfections, Causes, Targets, and Resistance Mechanisms: Traditional and Alternative Antifungal Agents". BioMed Research International (Hindawi Limited) 2013: 1–13. doi:10.1155/2013/204237. ISSN 2314-6133. PMID 23878798.
- ↑ "Chronic vaginal candidiasis. Management in the postmenopausal patient". Drugs & Aging 16 (5): 335–9. May 2000. doi:10.2165/00002512-200016050-00003. PMID 10917071.
- ↑ 46.0 46.1 Saag, Kenneth G; Furst, MScDaniel E; Barnes, Peter J. "Major side effects of inhaled glucocorticoids". https://www.uptodate.com/contents/major-side-effects-of-inhaled-glucocorticoids#H4.
- ↑ "Bench-to-bedside review: therapeutic management of invasive candidiasis in the intensive care unit". Critical Care 14 (6): 244. December 2010. doi:10.1186/cc9239. PMID 21144007.
- ↑ "Candida infections: an overview". Critical Reviews in Microbiology 15 (1): 1–5. 1987. doi:10.3109/10408418709104444. PMID 3319417.
- ↑ "A comparative histopathological study of systemic candidiasis in association with experimentally induced breast cancer". Oncology Letters 1 (1): 215–222. January 2010. doi:10.3892/ol_00000039. PMID 22966285. PMC 3436220. http://www.spandidos-publications.com/ol/1/1/215.
- ↑ 50.0 50.1 "Oral candidiasis". Postgraduate Medical Journal 78 (922): 455–9. August 2002. doi:10.1136/pmj.78.922.455. PMID 12185216.
- ↑ "Colonisation of extragenital sites by Candida in women with recurrent vulvovaginal candidosis". BJOG 110 (10): 934–7. October 2003. doi:10.1111/j.1471-0528.2003.01445.x. PMID 14550364.
- ↑ 52.0 52.1 "Mycoses of the urogenital tract". Mycoses 40 (Suppl 2): 33–6. 1997. doi:10.1111/j.1439-0507.1997.tb00561.x. PMID 9476502.
- ↑ "Genital colonisation and infection with Candida in heterosexual and homosexual males". Genitourinary Medicine 73 (5): 394–6. October 1997. doi:10.1136/sti.73.5.394. PMID 9534752.
- ↑ 54.0 54.1 "Congenital candidiasis as a subject of research in medicine and human ecology". Annals of Parasitology 60 (3): 179–89. 2014. PMID 25281815.
- ↑ 55.0 55.1 "Oral thrush - Diagnosis and treatment - Mayo Clinic". https://www.mayoclinic.org/diseases-conditions/oral-thrush/diagnosis-treatment/drc-20353539.
- ↑ Warren, Terri (2010). "Is It a Yeast Infection?". http://women.webmd.com/features/is-it-yeast-infection.
- ↑ "Definition of a type of abnormal vaginal flora that is distinct from bacterial vaginosis: aerobic vaginitis". BJOG 109 (1): 34–43. January 2002. doi:10.1111/j.1471-0528.2002.00432.x. PMID 11845812. https://repository.uantwerpen.be/docman/irua/30bd6b/6019.pdf.
- ↑ "Over-the-counter antifungal drug misuse associated with patient-diagnosed vulvovaginal candidiasis". Obstetrics and Gynecology 99 (3): 419–25. March 2002. doi:10.1016/S0029-7844(01)01759-8. PMID 11864668.
- ↑ "Fluorescence staining vs. routine KOH smear for rapid diagnosis of oral candidiasis-A diagnostic test". Oral Diseases 26 (5): 941–47. July 2020. doi:10.1111/odi.13293. PMID 32011074.
- ↑ Guarner, J.; Brandt, M. E. (2011-04-01). "Histopathologic Diagnosis of Fungal Infections in the 21st Century". Clinical Microbiology Reviews (American Society for Microbiology) 24 (2): 247–280. doi:10.1128/cmr.00053-10. ISSN 0893-8512. PMID 21482725.
- ↑ "Candidiasis: Workup". WebMD. 18 August 2015. http://emedicine.medscape.com/article/213853-workup#showall.
- ↑ "Bacterial vaginosis: a review on clinical trials with probiotics". The New Microbiologica 36 (3): 229–38. July 2013. PMID 23912864. http://www.newmicrobiologica.org/PUB/allegati_pdf/2013/3/229.pdf.
- ↑ "Genital mycotic infections in patients with diabetes". Postgraduate Medicine 125 (3): 33–46. May 2013. doi:10.3810/pgm.2013.05.2650. PMID 23748505.
- ↑ 64.0 64.1 James, William D et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. pp. 308–311. ISBN 978-0-7216-2921-6.
- ↑ "Terbinafine in onychomycosis with involvement by non-dermatophytic fungi". The British Journal of Dermatology 130 (Suppl 43): 16–21. April 1994. doi:10.1111/j.1365-2133.1994.tb06088.x. PMID 8186136.
- ↑ Reiss, Errol; Shadomy, H. Jean; Lyon, G. Marshall (2011). "Chapter 11". Fundamental medical mycology. Hoboken, N.J.: John Wiley & Sons. ISBN 978-1-118-10176-6. https://books.google.com/books?id=eTkxR7lxr4YC&q=candidiasis&pg=PT360.
- ↑ Mobley, David P.; Cappelli, Connie C. (2008). Prevention in clinical oral health care. St. Louis, Mo.: Mosby Elsevier. p. 254. ISBN 978-0-323-03695-5. https://books.google.com/books?id=k9fbhs2PMTIC&pg=PA254.
- ↑ "Probiotics for prevention of recurrent vulvovaginal candidiasis: a review". The Journal of Antimicrobial Chemotherapy 58 (2): 266–72. August 2006. doi:10.1093/jac/dkl246. PMID 16790461. "Thus, the available evidence for the use of probiotics for prevention of recurrent VVC is limited".
- ↑ Walker, Marsha (2008). "Conquering Common Breast-feeding Problems" (in en). The Journal of Perinatal & Neonatal Nursing 22 (4): 267–274. doi:10.1097/01.JPN.0000341356.45446.23. ISSN 0893-2190. PMID 19011490.
- ↑ "Male thrush: everything you need to know" (in en). https://www.medino.com/article/what-is-male-thrush-symptoms-treatment.
- ↑ "Fungicidal activity of fluconazole against Candida albicans in a synthetic vagina-simulative medium". Antimicrobial Agents and Chemotherapy 48 (1): 161–7. January 2004. doi:10.1128/AAC.48.1.161-167.2004. PMID 14693534.
- ↑ "The genetic basis of fluconazole resistance development in Candida albicans". Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease 1587 (2–3): 240–8. July 2002. doi:10.1016/s0925-4439(02)00087-x. PMID 12084466.
- ↑ 73.0 73.1 73.2 "Vaginal yeast infections during pregnancy". Canadian Family Physician 55 (3): 255–6. March 2009. PMID 19282531.
- ↑ "Alternative and complementary therapies for vulvovaginal candidiasis". Folia Microbiologica 64 (2): 133–141. March 2019. doi:10.1007/s12223-018-0652-x. PMID 30269301.
- ↑ "Systemic candidiasis". U.S. DHHS, National Institute of Health. Oct 2014. http://rarediseases.info.nih.gov/gard/1076/systemic-candidiasis/resources/1.
- ↑ "Clinical Features and Mortality of Nosocomial Candidemia in Very Old Patients: A Multicentre Italian Study" (in en). Gerontology 66 (6): 532–541. 2020. doi:10.1159/000510638. ISSN 0304-324X. PMID 33070136. https://www.karger.com/Article/FullText/510638. Retrieved 2023-10-26.
- ↑ "Pathogenesis and treatment of oral candidosis". Journal of Oral Microbiology 3: 5771. January 2011. doi:10.3402/jom.v3i0.5771. PMID 21547018.
- ↑ Bouquot, Brad W.; Neville, Douglas D.; Damm, Carl M.; Allen, Jerry E. (2002). Oral & maxillofacial pathology (2. ed.). Philadelphia: W.B. Saunders. pp. 189–197. ISBN 978-0-7216-9003-2.
- ↑ "Oral candidiasis: pathogenesis, clinical presentation, diagnosis and treatment strategies". Journal of the California Dental Association 41 (4): 263–8. April 2013. doi:10.1080/19424396.2013.12222301. PMID 23705242.
- ↑ Sobel, Jack D (2007). "Vulvovaginal candidosis". The Lancet 369 (9577): 1961–1971. doi:10.1016/s0140-6736(07)60917-9. ISSN 0140-6736. PMID 17560449.
- ↑ "Estimation of Direct Healthcare Costs of Fungal Diseases in the United States". Clinical Infectious Diseases 68 (11): 1791–1797. May 2019. doi:10.1093/cid/ciy776. PMID 30204844.
- ↑ Gow, Neil A. R. G (8 May 2002). "Candida albicans - a fungal Dr Jekyll and Mr Hyde". Mycologist 16 (1). doi:10.1017/S0269915X02006183. https://pdfs.semanticscholar.org/4190/f12a123810269fb91e6d9134c52ccfad096f.pdf.
- ↑ "Candida". United States: Centers for Disease Control and Prevention. https://www.cdc.gov/hai/eip/pdf/Candida-factsheet.pdf.
- ↑ Vallabhaneni, Snigdha; Mody, Rajal K.; Walker, Tiffany; Chiller, Tom (2016). "1. The global burden of fungal disease". in Sobel, Jack; Ostrosky-Zeichner, Luis (in en). Fungal Infections, An Issue of Infectious Disease Clinics of North America. Philadelphia: Elsevier. pp. 2–3. ISBN 978-0-323-41649-8. https://books.google.com/books?id=uwndCwAAQBAJ&pg=PA2. Retrieved 2021-05-29.
- ↑ Knoke, M.; Bernhardt, H. (July 2006). "The first description of an oesophageal candidosis by Bernhard von Langenbeck in 1839". Mycoses 49 (4): 283–287. doi:10.1111/j.1439-0507.2006.01237.x. PMID 16784441.
- ↑ 86.0 86.1 86.2 86.3 86.4 86.5 "Oral candidiasis. History, classification, and clinical presentation". Oral Surgery, Oral Medicine, and Oral Pathology 78 (2): 189–93. August 1994. doi:10.1016/0030-4220(94)90146-5. PMID 7936588.
- ↑ "Thrush - nightmare of the foundling hospitals". Neonatology 101 (3): 159–65. 2012. doi:10.1159/000329879. PMID 22024688.
- ↑ “Thrush, N. (2).” Oxford English Dictionary, Oxford UP, July 2023, https://doi.org/10.1093/OED/1201547560.
- ↑ International Code of Botanical Nomenclature. Königstein. 2000. ISBN 978-3-904144-22-3. http://www.bgbm.org/iapt/nomenclature/code/SaintLouis/0000St.Luistitle.htm. Retrieved 2008-11-23.
- ↑ "Candida infections: an overview". Critical Reviews in Microbiology 15 (1): 1–5. 1987. doi:10.3109/10408418709104444. PMID 3319417.
- ↑ 91.0 91.1 Barrett, Stephen (October 8, 2005). "Dubious "Yeast Allergies"". Quackwatch. http://www.quackwatch.org/01QuackeryRelatedTopics/candida.html.
- ↑ 92.0 92.1 Jarvis WT. "Candidiasis Hypersensitivity". National Council Against Health Fraud. http://www.ncahf.org/articles/c-d/candida.html.
- ↑ "Inflammation and gastrointestinal Candida colonization". Current Opinion in Microbiology 14 (4): 386–91. August 2011. doi:10.1016/j.mib.2011.07.015. PMID 21802979.
- ↑ "An immunological link between Candida albicans colonization and Crohn's disease". Critical Reviews in Microbiology 41 (2): 135–9. June 2015. doi:10.3109/1040841X.2013.810587. PMID 23855357. https://zenodo.org/record/3440733.
- ↑ "Growing resistance to antifungal drugs 'a global issue'". BBC News. 17 May 2018. https://www.bbc.com/news/health-44160730.
- ↑ "Invasive candidiasis". Nature Reviews. Disease Primers 4. May 2018. doi:10.1038/nrdp.2018.26. PMID 29749387.
External links
- "Yeast Infections". MedlinePlus. U.S. National Library of Medicine. https://medlineplus.gov/yeastinfections.html.
| Classification | |
|---|---|
| External resources |
 |
