Chemistry:Antiseptic
An antiseptic (Greek: ἀντί, romanized: anti, lit. 'against'[1] and σηπτικός, sēptikos, 'putrefactive'[2]) is an antimicrobial substance or compound that is applied to living tissue to reduce the possibility of sepsis, infection or putrefaction. Antiseptics are generally distinguished from antibiotics by the latter's ability to safely destroy bacteria within the body, and from disinfectants, which destroy microorganisms found on non-living objects.[3]
Antibacterials include antiseptics that have the proven ability to act against bacteria. Microbicides which destroy virus particles are called viricides or antivirals. Antifungals, also known as antimycotics, are pharmaceutical fungicides used to treat and prevent mycosis (fungal infection).[4]
Surgery

The widespread introduction of antiseptic surgical methods was initiated by the publishing of the paper Antiseptic Principle of the Practice of Surgery in 1867 by Joseph Lister, which was inspired by Louis Pasteur's germ theory of putrefaction.[5][6] In this paper, Lister advocated the use of carbolic acid (phenol) as a method of ensuring that any germs present were killed. Some of this work was anticipated by:
- Ancient Greek physicians Galen (c. 130–200) and Hippocrates (c. 400 BC) as well as Sumerian clay tablets dating from 2150 BC that advocate the use of similar techniques.[7]
- Florence Nightingale, who contributed substantially to the report of the Royal Commission on the Health of the Army (1856–1857), based on her earlier work
- Ignaz Semmelweis, who published his work The Cause, Concept and Prophylaxis of Childbed Fever in 1861, summarizing experiments and observations since 1847[8]
- Medieval surgeons Hugh of Lucca, Theoderic of Servia, and his pupil Henri de Mondeville were opponents of Galen's opinion that pus was important to healing, which had led ancient and medieval surgeons to let pus remain in wounds. They advocated draining and cleaning the wound edges with wine, dressing the wound after suturing, if necessary and leaving the dressing on for ten days, soaking it in warm wine all the while, before changing it. Their theories were bitterly opposed by Galenist Guy de Chauliac and others trained in the classical tradition.[9]
- Oliver Wendell Holmes Sr., who published The Contagiousness of Puerperal Fever in 1843
Some common antiseptics
Antiseptics can be subdivided into about eight classes of materials. These classes can be subdivided according to their mechanism of action: small molecules that indiscriminately react with organic compounds and kill microorganisms (peroxides, iodine, phenols) and more complex molecules that disrupt the cell walls of the bacteria.[10]
- Alcohols, including ethanol and 2-propanol/isopropanol are sometimes referred to as surgical spirit. They are used to disinfect the skin before injections, among other uses.
- Diguanides including chlorhexidine gluconate, a bacteriocidal antiseptic which (with an alcoholic solvent) is considered a safe and effective antiseptic for reducing the risk of infection after clean surgery,[11] including tourniquet-controlled upper limb surgery.[12] It is also used in mouthwashes to treat inflammation of the gums (gingivitis). Polyhexanide (polyhexamethylene biguanide, PHMB) is an antimicrobial compound suitable for clinical use in critically colonized or infected acute and chronic wounds. The physicochemical action on the bacterial envelope prevents or impedes the development of resistant bacterial strains.[13][14][15]
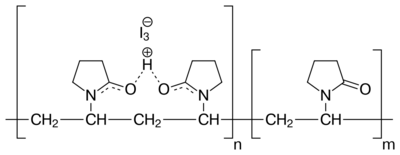
- Iodine, especially in the form of povidone-iodine, is widely used because it is well tolerated; does not negatively affect wound healing; leaves a deposit of active iodine, thereby creating the so-called "remnant", or persistent effect; and has wide scope of antimicrobial activity. The traditional iodine antiseptic is an alcohol solution (called tincture of iodine) or as Lugol's iodine solution. Some studies[16] do not recommend disinfecting minor wounds with iodine because of concern that it may induce scar tissue formation and increase healing time. However, concentrations of 1% iodine or less have not been shown to increase healing time and are not otherwise distinguishable from treatment with saline.[17] Iodine will kill all principal pathogens and, given enough time, even spores, which are considered to be the most difficult form of microorganisms to be inactivated by disinfectants and antiseptics.
- Octenidine dihydrochloride, currently increasingly used in continental Europe, often as a chlorhexidine substitute.
- Peroxides, such as hydrogen peroxide and benzoyl peroxide. Commonly, 3% solutions of hydrogen peroxide have been used in household first aid for scrapes, etc. However, the strong oxidization causes scar formation and increases healing time during fetal development.[18]
- Phenols such as phenol itself (as introduced by Lister) and triclosan, hexachlorophene, chlorocresol, and chloroxylenol. The latter is used for skin disinfection and cleaning surgical instruments. It is also used within a number of household disinfectants and wound cleaners.
- Quat salts such as benzalkonium chloride/Lidocaine (trade name Bactine among others), cetylpyridinium chloride, or cetrimide. These surfactants disrupt cell walls.
- Quinolines such as hydroxyquinolone, dequalium chloride, or chlorquinaldol.
- 4-Hexylresorcinol, or S.T.37
See also
- Actinonin
- Henry Jacques Garrigues, introduced antiseptic obstetrics to North America
- NASLA (Nanostructured Anti-septical Coatings) Project
References
- ↑ Liddell, Henry George; Scott, Robert. "ἀντί". A Greek-English Lexicon. Perseus perseus.tufts.edu. https://www.perseus.tufts.edu/hopper/text?doc=Perseus%3Atext%3A1999.04.0057%3Aentry%3Da%29nti%2F.
- ↑ Liddell, Henry George; Scott, Robert. "σηπτικός". A Greek-English Lexicon. Perseus perseus.tufts.edu. https://www.perseus.tufts.edu/hopper/text?doc=Perseus%3Atext%3A1999.04.0057%3Aentry%3Dshptiko%2Fs.
- ↑ McDonnell, Gerald; Russell, A. Denver (January 1999). "Antiseptics and Disinfectants: Activity, Action, and Resistance". Clinical Microbiology Reviews 12 (1): 147–79. doi:10.1128/CMR.12.1.147. PMID 9880479.
- ↑ Wang, Jing; Zhou, Min; Xu, Jing-Yan; Zhou, Rong-Fu; Chen, Bing; Wan, Yuan (8 October 2020). "Comparison of Antifungal Prophylaxis Drugs in Patients With Hematological Disease or Undergoing Hematopoietic Stem Cell Transplantation: A Systematic Review and Network Meta-analysis" (in en). JAMA Network Open 3 (10): e2017652. doi:10.1001/jamanetworkopen.2020.17652. ISSN 2574-3805. PMID 33030550. PMC 7545296. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2771516. Retrieved 18 February 2023.
- ↑ Chisholm, Hugh, ed (1911). "Antiseptics". Encyclopædia Britannica. 2 (11th ed.). Cambridge University Press. p. 146.
- ↑ Bashford, Henry (Apr 1951). "The Coming of Antisepsis". History Today 1 (4): 37–41.
- ↑ "Inflammation in wound repair: molecular and cellular mechanisms". J. Invest. Dermatol. 127 (3): 514–25. 2007. doi:10.1038/sj.jid.5700701. PMID 17299434.
- ↑ "Ignaz Semmelweis and the birth of infection control". Qual Saf Health Care 13 (3): 233–4. 2004. doi:10.1136/qhc.13.3.233. PMID 15175497.
- ↑ Edwards H (1976). "Theodoric of Cervia, a medieval antiseptic surgeon". Proceedings of the Royal Society 69 (3): 553–5. PMID 790395.
- ↑ Kutscher, Bernhard (2020). "Ullmann's Encyclopedia of Industrial Chemistry". Ullmann's Encyclopedia of Industrial Chemistry. Weinheim: Wiley-VCH. pp. 1–22. doi:10.1002/14356007.w08_w03.
- ↑ Wade, Ryckie G.; Burr, Nicholas E.; McCauley, Gordon; Bourke, Grainne; Efthimiou, Orestis (1 September 2020). "The Comparative Efficacy of Chlorhexidine Gluconate and Povidone-iodine Antiseptics for the Prevention of Infection in Clean Surgery: A Systematic Review and Network Meta-analysis". Annals of Surgery Publish Ahead of Print (6): e481–e488. doi:10.1097/SLA.0000000000004076. PMID 32773627.
- ↑ Wade, Ryckie G; Bourke, Gráinne; Wormald, Justin C R; Totty, Joshua Philip; Stanley, Guy Henry Morton; Lewandowski, Andrew; Rakhra, Sandeep Singh; Gardiner, Matthew D et al. (9 November 2021). "Chlorhexidine versus povidone–iodine skin antisepsis before upper limb surgery (CIPHUR): an international multicentre prospective cohort study". BJS Open 5 (6): zrab117. doi:10.1093/bjsopen/zrab117. PMID 34915557.
- ↑ Kaehn K (2010). "Polihexanide: a safe and highly effective biocide". Skin Pharmacol Physiol 23 Suppl: 7–16. doi:10.1159/000318237. PMID 20829657.
- ↑ "Clinical use of polihexanide on acute and chronic wounds for antisepsis and decontamination". Skin Pharmacol Physiol 23 Suppl: 45–51. 2010. doi:10.1159/000318267. PMID 20829662.
- ↑ "Comparison of PHMB-containing dressing and silver dressings in patients with critically colonised or locally infected wounds". J Wound Care 21 (1): 12, 14–6, 18–20. January 2012. doi:10.12968/jowc.2012.21.1.12. PMID 22240928. http://www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=88747;article=JWC_21_1_12_20.
- ↑ Vermeulen, H.; Westerbos, S.J.; Ubbink, D.T. (2010). "Benefit and harm of iodine in wound care: a systematic review". Journal of Hospital Infection 76 (3): 191–199. doi:10.1016/j.jhin.2010.04.026. ISSN 0195-6701. PMID 20619933.
- ↑ "Antiseptics on Wounds: An Area of Controversy: Hydrogen Peroxide". Medscape.com. http://www.medscape.com/viewarticle/456300_3.
- ↑ "Hydrogen peroxide disrupts scarless fetal wound repair". Wound Repair Regen 13 (5): 513–9. 2005. doi:10.1111/j.1067-1927.2005.00072.x. PMID 16176460.
External links
 "Antiseptic". New International Encyclopedia. 1905.
"Antiseptic". New International Encyclopedia. 1905.
 |
