Chemistry:Ximelagatran
 | |
| Clinical data | |
|---|---|
| Trade names | Exanta |
| Pregnancy category |
|
| Routes of administration | Oral (tablets) |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 20% |
| Metabolism | to melagatran |
| Elimination half-life | 3–5 hours |
| Excretion | Renal (80%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| Chemical and physical data | |
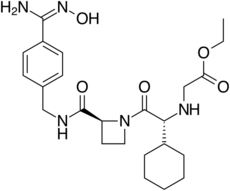
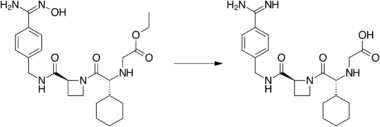
| Formula | C24H35N5O5 |
| Molar mass | 473.574 g·mol−1 (429 g/mol after conversion) |
| 3D model (JSmol) | |
| |
| |
| | |
Ximelagatran (Exanta or Exarta, H 376/95) is an anticoagulant that has been investigated extensively as a replacement for warfarin[1] that would overcome the problematic dietary, drug interaction, and monitoring issues associated with warfarin therapy. In 2006, its manufacturer AstraZeneca announced that it would withdraw pending applications for marketing approval after reports of hepatotoxicity (liver damage) during trials, and discontinue its distribution in countries where the drug had been approved (Germany, Portugal, Sweden, Finland, Norway, Iceland, Austria, Denmark, France, Switzerland, Argentina and Brazil).[2]
Method of action
Ximelagatran, a direct thrombin inhibitor,[3] was the first member of this class that can be taken orally. It acts solely by inhibiting the actions of thrombin. It is taken orally twice daily, and rapidly absorbed by the small intestine. Ximelagatran is a prodrug, being converted in vivo to the active agent melagatran. This conversion takes place in the liver and many other tissues through hydrolysis and dehydroxylation (replacing the ethyl and hydroxyl groups with hydrogen).
Uses
Ximelagatran was expected to replace warfarin and sometimes aspirin and heparin in many therapeutic settings, including deep venous thrombosis, prevention of secondary venous thromboembolism and complications of atrial fibrillation such as stroke. The efficacy of ximelagatran for these indications had been well documented,[4][5][6] except for non valvular atrial fibrillation.
An advantage, according to early reports by its manufacturer, was that it could be taken orally without any monitoring of its anticoagulant properties. This would have set it apart from warfarin and heparin, which require monitoring of the international normalized ratio (INR) and the partial thromboplastin time (PTT), respectively. A disadvantage recognised early was the absence of an antidote in case acute bleeding develops, while warfarin can be antagonised by prothrombin complex concentrate and/or vitamin K and heparin by protamine sulfate.
Side effects
Ximelagatran was generally well tolerated in the trial populations, but a small proportion (5–6%) developed elevated liver enzyme levels, which prompted the FDA to reject an initial application for approval in 2004. The further development was discontinued in 2006 following reports of hepatotoxicity. Subsequent analysis of Phase 2 clinical study data using extreme value modelling showed that the elevated liver enzyme levels observed in Phase 3 clinical studies could have been predicted; if this had been known at the time, it might have affected decisions on future development of the compound.[7]
A chemically different but pharmacologically similar substance, AZD-0837, was developed by AstraZeneca for similar indications.[2] It is a prodrug of a potent, competitive, reversible inhibitor of free and fibrin-bound thrombin called ARH0637.[8] The development of AZD-0837 has been discontinued. Due to a limitation identified in long-term stability of the extended-release AZD-0837 drug product, a follow-up study from ASSURE on stroke prevention in patients with non-valvular atrial fibrillation, was prematurely closed in 2010 after 2 years. There was also a numerically higher mortality against warfarin.[9][10][11] In a Phase 2 trial for AF the mean serum creatinine concentration increased by about 10% from baseline in patients treated with AZD-0837, which returned to baseline after cessation of therapy.[12]
References
- ↑ "Beyond unfractionated heparin and warfarin: current and future advances". Circulation 116 (5): 552–560. July 2007. doi:10.1161/CIRCULATIONAHA.106.685974. PMID 17664384.
- ↑ 2.0 2.1 "AstraZeneca Decides to Withdraw Exanta" (Press release). AstraZeneca. February 14, 2006. Retrieved 2012-07-16.
- ↑ "Ximelagatran: direct thrombin inhibitor". Vascular Health and Risk Management 2 (1): 49–58. 2006. doi:10.2147/vhrm.2006.2.1.49. PMID 17319469.
- ↑ "A randomized, controlled, dose-guiding study of the oral direct thrombin inhibitor ximelagatran compared with standard therapy for the treatment of acute deep vein thrombosis: THRIVE I". Journal of Thrombosis and Haemostasis 1 (1): 41–47. January 2003. doi:10.1046/j.1538-7836.2003.00034.x. PMID 12871538.
- ↑ "Comparison of ximelagatran with warfarin for the prevention of venous thromboembolism after total knee replacement". The New England Journal of Medicine 349 (18): 1703–1712. October 2003. doi:10.1056/NEJMoa035162. PMID 14585938.
- ↑ "Secondary prevention of venous thromboembolism with the oral direct thrombin inhibitor ximelagatran". The New England Journal of Medicine 349 (18): 1713–1721. October 2003. doi:10.1056/NEJMoa030104. PMID 14585939.
- ↑ "Predicting potential liver toxicity from phase 2 data: a case study with ximelagatran". Statistics in Medicine 33 (17): 2914–2923. July 2014. doi:10.1002/sim.6142. PMID 24623062.
- ↑ "Development and clinical applications of novel oral anticoagulants. Part II. Drugs under clinical investigation". Discovery Medicine 13 (73): 445–450. June 2012. PMID 22742650.
- ↑ "AZD0837". Astrazenecaclinicaltrials.com. http://www.astrazenecaclinicaltrials.com/other-drug-products/in_development_drugs/AZD0837/.
- ↑ "Long-term treatment with the oral direct thrombin inhibitor AZD0837, compared to Vitamin-K antagonists, as stroke prevention in patients with non-valvular atrial fibrillation and one or more risk factors for stroke and systemic embolic events. A 5-year follow-up study study". Clinical Study Report Synopsis. AstraZeneca. 21 January 2010. http://www.astrazenecaclinicaltrials.com/_mshost800325/content/clinical-trials/resources/pdf/D1250C00042.
- ↑ "New anticoagulants". Circulation 121 (13): 1523–1532. April 2010. doi:10.1161/CIRCULATIONAHA.109.853119. PMID 20368532.
- ↑ "Oral direct thrombin inhibitor AZD0837 for the prevention of stroke and systemic embolism in patients with non-valvular atrial fibrillation: a randomized dose-guiding, safety, and tolerability study of four doses of AZD0837 vs. vitamin K antagonists". European Heart Journal 30 (23): 2897–2907. December 2009. doi:10.1093/eurheartj/ehp318. PMID 19690349.
External links
- "Ximelagatran". Drug Information Portal. U.S. National Library of Medicine. https://druginfo.nlm.nih.gov/drugportal/name/ximelagatran.
 |

