Medicine:Monkeypox
| Monkeypox | |
|---|---|
 | |
| Monkeypox rash on arm and leg of a four-year-old girl in 1971 | |
| Specialty | Infectious disease[1] |
| Symptoms | Fever, headache, muscle pains, shivering, blistering rash, swollen lymph nodes[2] |
| Complications | Secondary infections, eye infection, visual loss, scarring,[3][2] encephalitis, sepsis, bronchopneumonia[4] |
| Usual onset | 5–21 days post exposure[5] |
| Duration | 2 to 4 weeks[5] |
| Types | Central African (Congo Basin), West African[6] |
| Causes | Monkeypox virus[7] |
| Diagnostic method | Testing for viral DNA[8] |
| Differential diagnosis | Chickenpox, smallpox[9] |
| Prevention | Smallpox vaccine, hand washing, covering rash, PPE, keeping away from sick people[10][11] |
| Treatment | Supportive, antivirals, vaccinia immune globulin[12] |
| Medication | Tecovirimat[3] |
| Prognosis | Most recover[13] |
| Frequency | Not as rare as previously thought[14] |
| Deaths | up to 3.6% (clade II),[15] up to 10.6%[15] (clade I, untreated)[16] |
Monkeypox is an infectious viral disease that can occur in humans and some other animals.[1] Symptoms include fever, swollen lymph nodes, and a rash that forms blisters and then crusts over.[1] The time from exposure to onset of symptoms ranges from five to twenty-one days.[3][5] The duration of symptoms is typically two to four weeks.[5] There may be mild symptoms, and it may occur without any symptoms being known.[3][17] The classic presentation of fever and muscle pains, followed by swollen glands, with lesions all at the same stage, has not been found to be common to all outbreaks.[1][18] Cases may be severe, especially in children, pregnant women or people with suppressed immune systems.[19]
The disease is caused by the monkeypox virus, a zoonotic virus in the genus Orthopoxvirus. The variola virus, the causative agent of smallpox, is also in this genus.[2] Of the two types in humans, clade II (formerly West African clade)[20] causes a less severe disease than the Central African (Congo basin) type.[21] It may spread from infected animals by handling infected meat or via bites or scratches.[22] Human-to-human transmission can occur through exposure to infected body fluids or contaminated objects, by small droplets, and possibly through the airborne route.[1][22] People can spread the virus from the onset of symptoms until all the lesions have scabbed and fallen off; with some evidence of spread for more than a week after lesions have crusted.[21] Diagnosis can be confirmed by testing a lesion for the virus's DNA.[8]
There is no known cure.[23] A study in 1988 found that the smallpox vaccine was around 85% protective in preventing infection in close contacts and in lessening the severity of the disease.[24] A newer smallpox and monkeypox vaccine based on modified vaccinia Ankara has been approved, but with limited availability.[3] Other measures include regular hand washing and avoiding sick people and animals.[25] Antiviral drugs, cidofovir and tecovirimat, vaccinia immune globulin and the smallpox vaccine may be used during outbreaks.[12][13] The illness is usually mild and most of those infected will recover within a few weeks without treatment.[13] Estimates of the risk of death vary from 1% to 10%, although few deaths as a consequence of monkeypox have been recorded since 2017.[26]
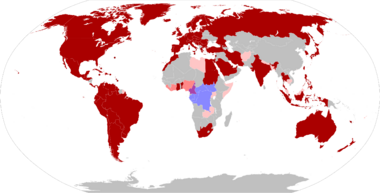
Several species of mammals are suspected to act as a natural reservoir of the virus.[3] Although it was once thought to be uncommon in humans, the quantity and severity of outbreaks has significantly increased since the 1980s,[27][28] possibly as a result of waning immunity since the stopping of routine smallpox vaccination.[9][14] The first cases in humans were found in 1970 in the Democratic Republic of the Congo (DRC).[29] There have been sporadic cases in Central and West Africa, and it is endemic in the DRC.[28] The 2022 monkeypox outbreak represents the first incidence of widespread community transmission outside of Africa, which was initially identified in the United Kingdom in May 2022, with subsequent cases confirmed in at least 74 countries[30] in all continents except Antarctica.[31][32][33][34][35][36] On 23 July 2022, the World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern (PHEIC)[37] with more than 53,000 reported cases in 75 countries and territories.
Signs and symptoms
It is possible for a person to be infected with monkeypox without showing any symptoms.[38] Monkeypox symptoms tend to begin 5 to 21 days after infection,[6] with early symptoms including headache, muscle pains, fever and fatigue, initially resembling influenza.[3][39][40] Within a few days of the fever, lesions characteristically appear on the face before appearing on the trunk then elsewhere such as palms of the hands and soles of the feet.[41][42] The disease can resemble chickenpox, measles and smallpox but is distinguished by the presence of swollen glands[3][39] which may appear behind the ear, below the jaw, in the neck or in the groin, before the onset of the rash.[9] Many cases in the 2022 monkeypox outbreak presented with genital and peri-anal lesions, fever, swollen lymph nodes, and pain when swallowing,[1] with some patients manifesting only single sores from the disease.[43]
Three-quarters of affected people have lesions on the palms and soles, more than two-thirds in the mouth, a third on the genitals and one in five have lesions in the eyes.[3] They begin as small flat spots, before becoming small bumps which then fill with at first clear fluid and then yellow fluid, which subsequently burst and scab over, persisting for around ten days.[5][39][44] There may be a few lesions or several thousand, sometimes merging to produce large lesions.[3] After healing, the lesions may leave pale marks before becoming dark scars.[2]
An unwell person may remain so for two to four weeks.[5]
Complications
Complications include secondary infections, pneumonia, sepsis, encephalitis, and loss of vision with severe eye infection.[3] If infection occurs during pregnancy, still birth or birth defects may occur.[45] The disease may be milder in people vaccinated against smallpox in childhood.[13] Patel and colleagues,[46] in the BMJ, demonstrate that this virus can produce severe symptoms, particularly in HIV-positive people. The descriptive case series reveal that symptoms can be so severe that hospitalization is required in 10% of cases. The study also shows that 75% of patients (15 out of 20 participants) admitted to the hospital were HIV-positive individuals. Overall, the study depict a new variety of clinical manifestations including proctitis and rectal perforation. The pictures of genital lesions[46] published in the BMJ show the severity of monkeypox, which is often described as causing moderate symptoms.[47]
In other animals
The disease has also been reported in dormice, tree squirrels, rope squirrels and non human primates.[3] Rodents such as rats and mice are likely susceptible but not known.[48][49][50] Signs and symptoms in animals vary among different species.[51] Monkeypox infected Gambian pouched rats may have mild symptoms.[48] During the 2003 US outbreak, affected prairie dogs presented with fever, cough, sore eyes, poor feeding and rash.[51] Non-human primates present similarly.[51] They may have breathing problems, facial swelling, mouth ulcers and swollen glands.[48] In cynomolgus monkeys, the time from exposure to symptoms[52] was noted to be around a week. Rabbits and rodents typically present with fever, cough, runny nose, sore eyes and swollen glands.[48] They develop small bumps that fill with yellow fluid and may have patches of hair loss and pneumonia.[48] Spread among animals occurs via the fecal-oral route and through the nose, through wounds and eating infected meat.[48] Death is more likely in baby monkeys.[48] The CDC recommend that animals exposed to monkeypox be quarantined for six weeks.[48]
Causes
Monkeypox in both humans and animals is caused by infection with the monkeypox virus – a double-stranded DNA virus in the genus Orthopoxvirus, family Poxviridae.[7] The virus was first identified in captive monkeys and is found mainly in tropical rainforest regions of Central and West Africa.[7] The two subtypes of virus are clade I and clade II (formerly Congo Basin and West African clades, matching the geographical areas).[16]
In addition to monkeys, the virus has been identified in Gambian pouched rats (Cricetomys gambianus), dormice (Graphiurus spp.) and African squirrels (Heliosciurus, and Funisciurus). The use of these animals as food may be an important source of transmission to humans.[53][3]
Transmission
Humans can be infected by an animal via a bite or scratch, bush meat preparation, or by contact with an infected animal’s bodily fluids or lesion material.[54] The virus is thought to enter the body through broken skin, the respiratory tract, or the mucous membranes of the eyes, nose, or mouth.[6]
Once a human is infected, transmission to other humans is common, with family members and hospital staff at particularly high risk of infection.[6] The virus can spread by respiratory (airborne) contact or by direct contact with an infected person's bodily fluids[15] or during pregnancy from mother to fetus.[54] There are indications that transmission can occur during sexual contact,[55] with infectious monkeypox virus able to be isolated from semen samples.[56] Prolonged shedding in seminal fluids has raised the possibility of a genital reservoir for monkeypox virus.[56][21] It is not known if the virus can spread through vaginal fluids.[54]
The virus can also spread via fomites or through indirect contact with lesion material, such as through contaminated bedding, even with standard personal protective equipment, likely through inhalation.[57] Risk factors for transmission include sharing a bed or room, or using the same utensils as an infected person. Increased transmission risk is associated with factors involving the introduction of virus to the oral mucosa.[39] It is not yet known if people without symptoms of monkeypox can spread the virus.[54]
Further research about the transmission of the strain responsible for the 2022 outbreak is ongoing, but it is not thought to be different from other strains of the clade II.[58][59]
People living with HIV
According to a CDC report, 41% of cases of monkeypox were among HIV-positive patients (136 out of 334 patients) between May and July 2022.[60] The New England Journal of Medicine (NEJM) also looked at more than 500 cases from different countries and found that 41% of them were among HIV patients.[61] In addition, a study published in The Lancet that looked at nearly 200 cases in Barcelona and Madrid discovered that 40% were HIV-positive.[62] Patel and colleagues[46] observed 197 patients from sexual health centres in south London between May and July 2022. They reported 35.5% patients had HIV-1 co-infection. 91.4% of these participants were receiving antiretroviral therapy and 78.6% had an undetectable HIV-1 viral load (<200 copies). The median CD4 count was 664 cells (interquartile range 522-894 cells). The proportion of HIV-positive individuals in these reports is significantly higher than the HIV rate among men who have sex with other men.[63] The reasons for this heavy overrepresentation of men living with HIV among monkeypox cases are not fully understood yet.
Diagnosis
Clinical differential diagnosis must consider other rash illnesses, such as chickenpox, measles, bacterial skin infections, scabies, syphilis and medication-associated allergies. Lymphadenopathy during the prodromal stage of illness can distinguish monkeypox from chickenpox or smallpox. Diagnosis can be verified by testing for the virus.[3]
Polymerase chain reaction (PCR) testing of samples from skin lesions is the preferred laboratory test. PCR blood tests are usually inconclusive because the virus remains in blood only a short time. To interpret test results, information is required on date of onset of fever, date of onset of rash, date of specimen collection, current stage of rash, and patient age.[3]
India has developed the first indigenously-developed RT- PCR kit for testing monkeypox disorder.[64]
Prevention
Vaccination against smallpox is assumed to protect against human monkeypox infection because they are closely related viruses, and the vaccine protects animals from experimental lethal monkeypox challenges.[65] This has not been conclusively demonstrated in humans because routine smallpox vaccination was discontinued following the eradication of smallpox.[3]
Smallpox vaccine has been reported to reduce the risk of monkeypox among previously vaccinated persons in Africa. The decrease in immunity to poxviruses in exposed populations is a factor in the prevalence of monkeypox. It is attributed to waning cross-protective immunity among those vaccinated before 1980, when mass smallpox vaccinations were discontinued, and to the gradually increasing proportion of unvaccinated individuals.[39]
The United States Centers for Disease Control and Prevention (CDC) recommends that persons investigating monkeypox outbreaks and involved in caring for infected individuals or animals should receive a smallpox vaccination to protect against monkeypox. Persons who have had close or intimate contact with individuals or animals confirmed to have monkeypox should also be vaccinated.[7] However, the CDC does not recommend pre-exposure vaccination for unexposed veterinarians, veterinary staff, or animal control officers, unless such persons are involved in field investigations.[7] No smallpox or monkeypox vaccine has been approved for use during pregnancy.[66] The CDC recommends that healthcare providers don a full set of personal protective equipment (PPE) before caring for an infected person. This includes a gown, mask, goggles, and a disposable filtering respirator (such as an N95). An infected person should be isolated in preferably a negative air pressure room or at least a private exam room to keep others from possible contact.[67]
Monkeypox prevention cannot be simplified to just providing a vaccine. There are more pressing challenges to address, such as access to treatment, veracity and availability of information, and quality of health care.[46] Public health messaging is perhaps the most important challenge. The multiple levels of interconnectivity and negotiated social meanings inherent to the disease require cooperation between medical professionals and patients to achieve correct public health communication.[68] Therefore, Scalvini[68] argues in the BMJ that it is necessary a "new ethic of shared responsibility" to educate people about dangers and give people from underprivileged groups the tools they need to make better decisions.
Treatment
In the European Union and the United States , tecovirimat is approved for the treatment of several poxviruses, including monkeypox.[69] BMJ Best Practice recommends tecovirimat or the smallpox treatment brincidofovir as the first line antiviral treatment if required, alongside supportive care (including antipyretic, fluid balance and oxygenation). Empirical antibiotic therapy or aciclovir may be used if secondary bacterial or varicella zoster infection is suspected, respectively.[70]
Outcome
After healing, the scabs may leave pale marks before becoming darker scars.[2] The risk of death in those infected ranges from 0% to 11%, depending on the type of monkeypox and location in the world.[3][28] Fatality rates have been reported as around 3.6% in West Africa and 10.6% in Central Africa.[28] Most reported deaths have occurred in young children and people with HIV infection.[21]
Epidemiology
In 1970, monkeypox was first associated with an illness as a disease in humans in the Democratic Republic of the Congo (formerly Zaire), in the town of Basankusu, Équateur Province.[71] Although it was once thought to be uncommon in humans, cases increased since the 1980s,[27][28] possibly as a result of waning immunity since the stopping of routine smallpox vaccination.[9]
Between 1981 and 1986 WHO surveillance in DRC/Zaire recorded 338 confirmed cases and 33 deaths (CFR 9.8%).[72] In 1996–1997, a second outbreak of human illness was identified in DRC/Zaire[73] and between 1991 and 1999, 511 cases were reported in DRC/Zaire.[72] Clade I of disease remains endemic in DRC and has a higher CFR[72] than the other genetic clade in Western Africa.[3]
By May 2022, the case fatality rate (CFR) of past outbreaks was around 3%–6%,[74] while the CFR of the 2022 outbreak remains below 1%. No human-to-human transmission was documented[72] until the 2022 monkeypox outbreak in Europe.[75] Clade II had an outbreak – the first outbreak of monkeypox outside of Africa – in Midwestern United States among owners of pet prairie dogs in 2003. Seventy-one people were reportedly infected, of whom none died.[76]
As of 2018, monkeypox was traditionally restricted to the ecology of tropical rainforests.[72] although the pattern was broken in 2005, when 49 cases were reported in Sudan (areas now South Sudan), with no fatalities.[77] The genetic analysis suggested that the virus did not originate in Sudan but was imported, most likely from DRC.[78]
Many more monkeypox cases have been reported in Central and West Africa, and in the Democratic Republic of Congo in particular: 2000 cases per year are known between 2011 and 2014. The collected data is often incomplete and unconfirmed, which hinders realistic estimations of the number of cases of monkeypox over time. Nevertheless, it was suggested that the number of reported monkeypox cases had increased and the geographical occurrence broadened as of 2018.[72]
2003 U.S. outbreak
In May 2003, a young child became ill with fever and rash after being bitten by a prairie dog purchased at a local swap meet near Milwaukee, Wisconsin.[79] In total, 71 cases of monkeypox were reported through June 20, 2003. All cases were traced to Gambian pouched rats imported from Accra, Ghana, in April 2003 by a Texas exotic animal distributor. No deaths resulted.[80] Electron microscopy and serologic studies were used to confirm that the disease was human monkeypox.[81]
People with monkeypox typically experienced prodromal symptoms of fever, headaches, muscle aches, chills, and drenching sweats. Roughly one-third of infected people had nonproductive coughs. This prodromal phase was followed 1–10 days later by the development of a papular rash that typically progressed through stages of vesiculation, pustulation, umbilication, and crusting. In some people, early lesions had become ulcerated.[82]
Rash distribution and lesions occurred on head, trunk, and extremities. Many of the people had initial and satellite lesions on palms, soles, and extremities. Rashes were generalized in some people. After onset of the rash, people generally manifested rash lesions in different stages. Everyone affected reported direct or close contact with prairie dogs, later found to be infected with the monkeypox virus.[82]
2017–2019 Nigeria outbreak
According to the Nigeria Centre for Disease Control (NCDC), between 1971 and 1978, only 10 human monkeypox infections were reported in the country.[83]
In September 2017, human monkeypox re-emerged in Nigeria, 39 years since it had been last reported. The subsequent 2017–18 Nigerian human monkeypox outbreak was, at that time, the largest ever outbreak of clade II of the virus, with 118 confirmed cases. Unlike previous outbreaks of this clade, infection was predominantly among young male adults and human-to-human transmission appears to have readily occurred. Seven deaths (5 male, 2 female, case fatality rate of 6%) were reported, including a baby and four HIV/AIDS patients. Additionally, a pregnant woman in her second trimester had a spontaneous miscarriage due to monkeypox infection.[84]
The Niger Delta University Teaching Hospital reported that a substantial number of its young adult cases had concomitant genital ulcers, syphilis and HIV infection.[85] Monkeypox spread around southeast and south Nigeria with some states and the federal government of Nigeria seeking ways to contain it.[86] By December 2017 it spread to Akwa Ibom, Abia, Bayelsa, Benue, Cross River, Delta, Edo, Ekiti, Enugu, Imo, Lagos, Nasarawa, Oyo, Plateau, Rivers and Federal Capital Territory.[87][88] The outbreak started in September 2017 and remained ongoing across multiple states as of May 2019.[89]
| State | Sep 2017 – Dec 2019 | Jan 2020 – Feb 2022 |
|---|---|---|
| Abia | 3 | 0 |
| Adamawa | 0 | 1 |
| Akwa Ibom | 7 | 0 |
| Anambra | 2 | 0 |
| Bayelsa | 37 | 6 |
| Benue | 2 | 0 |
| Cross River | 13 | 1 |
| Delta | 19 | 10 |
| Ebonyi | 0 | 1 |
| Edo | 6 | 4 |
| Ekiti | 2 | 0 |
| Enugu | 4 | 0 |
| Federal Capital Territory | 5 | 2 |
| Imo | 8 | 1 |
| Lagos | 20 | 11 |
| Nasarawa | 2 | 0 |
| Niger | 0 | 1 |
| Ogun | 0 | 1 |
| Oyo | 6 | 0 |
| Plateau | 2 | 1 |
| Rivers | 46 | 6 |
| Totals | 184 | 46 |
The Centers for Disease Control and Prevention reported cases of American travelers contracting Monkeypox upon return from Lagos and Ibadan.[91] Agam Rao, a medical officer in the Division of Pathogens and High Consequence Pathology at the CDC, said that since 2018 all cases reported outside Africa have come from Nigeria.[92]
In a 2021 article Oyewale Tomori pointed out that the number of monkeypox infections in Nigeria through 2021 was likely to be under-represented, because much of the Nigerian population had been avoiding healthcare facilities due to fear of contracting COVID-19.[83]
In May 2022, the Nigerian government released a report stating that between 2017 and 2022, 558 cases were confirmed across 32 states and the Federal Capital Territory. The Rivers State was the most affected by monkeypox followed by Bayelsa and Lagos. There were 8 deaths reported, making for a 3.5% Case Fatality Ratio. In 2022, NCDC implemented a National Technical Working Group for reporting and monitoring infections, strengthening response capacity.[93]
2018 and 2019 United Kingdom cases
In September 2018, the United Kingdom 's first case of monkeypox was recorded. The person, a Nigerian national, is believed to have contracted monkeypox in Nigeria before travelling to the United Kingdom.[94] According to Public Health England, the person was staying in a naval base in Cornwall before being moved to the Royal Free Hospital's specialised infectious disease unit. People who had been in contact with the person since he contracted the disease were contacted.[95]
A second case was confirmed in the town of Blackpool,[96][97] with a further case that of a medical worker who cared for the case from Blackpool.[98] A fourth case occurred on 3 December 2019, when monkeypox was diagnosed in a person in south west England. They were travelling to the UK from Nigeria.[99]
2019 Singapore case
On 8 May 2019, a 38-year-old man who travelled from Nigeria was hospitalised in an isolation ward at the National Centre for Infectious Diseases in Singapore, after being confirmed as the country's first case of monkeypox. As a result, 22 people were quarantined.[100] The case may have been linked to a simultaneous outbreak in Nigeria.[89]
2021 cases in United Kingdom, United States
On 24 May in the UK, three cases of monkeypox from a single household were identified by Public Health Wales. The cases were also announced by Health Secretary Matt Hancock while addressing MPs. The index case was diagnosed on 24 May after traveling from Nigeria. The second case was reported on 2 June, and the third on 24 June.[101][102] One of the three patients, an adult female, was treated with tecovirimat.[21] On day 7 of tecovirimat, she was discharged from hospital to complete her second week of treatment at home.[21]
On 14 July in the US, an American returning from a trip in Nigeria was diagnosed with monkeypox. Subsequent testing identified the virus as belonging to clade II. The patient was hospitalized and treated with tecovirimat and was discharged after 32 days, at which time monkeypox virus DNA could no longer be detected in residual skin lesions.[103]
2022 outbreak
History
Monkeypox was first identified as a distinct illness in 1958 among laboratory monkeys in Copenhagen, Denmark.[104] The first documented cases in humans was in 1970, in six unvaccinated children during the smallpox eradication efforts; the first being a 9-month old boy in the Democratic Republic of the Congo (formerly Zaire).[28][105] The others, including three who were playmates, were in Liberia and Sierra Leone.[105][106] It was noted to be less easily transmissible than smallpox.[2] From 1981 to 1986, over 300 cases of human monkeypox were reported in the DRC, the majority being due to contact with animals.[107] In 1996, the disease reemerged in the DRC with 88% of cases resulting from human-to-human transmission.[2] Small viral outbreaks with a death rate in the range of 10% and a secondary human-to-human infection rate of about the same amount occur routinely in equatorial Central and West Africa.[107] In humans, the disease remained confined to the rain forests of Western and Central Africa until 2003, when an outbreak of monkeypox occurred in the US.[108] All cases were traced to sick rodents imported from Ghana.[2] Local prairie dogs caught the infection and passed it onto their owners.[2] The disease was found to be mild and there were no deaths.[2] Between 1970 and 2019 the disease was reported in 10 African countries; mostly in Central and West Africa.[28]
In 2018, cases of monkeypox were diagnosed in the UK in two unrelated travellers from Nigeria.[109] That year the first human-to-human transmission outside of Africa was confirmed in the UK.[110] This person was a healthcare worker who possibly contracted the disease from contaminated bedlinen.[109] Cases were also reported in travellers to Israel and Singapore.[110] The UK saw further cases in 2019 and 2021.[13]
In June 2022, the World Health Organization announced that it would find a new name for the disease, in line with its policy to avoid misleading associations with specific regions or animals.[111]
On 31 July 2022, the first death from monkeypox was recorded in India: a 22-year-old man who had returned from the UAE died.[112]
See also
- 2003 Midwest monkeypox outbreak
- 2022 monkeypox outbreak
- 2022 monkeypox outbreak in Canada
- 2022 monkeypox outbreak in the United States
- 2022 monkeypox outbreak in the United Kingdom
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 "Multi-country monkeypox outbreak: situation update". World Health Organization. 4 June 2022. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON390.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Petersen, Brett W.; Damon, Inger K. (2020). "348. Smallpox, monkeypox and other poxvirus infections". in Goldman, Lee; Schafer, Andrew I.. Goldman-Cecil Medicine. 2 (26th ed.). Philadelphia: Elsevier. pp. 2180–2183. ISBN 978-0-323-53266-2. https://books.google.com/books?id=7pKqDwAAQBAJ&dq=monkeypox&pg=PA2180.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 "WHO Factsheet – Monkeypox". World Health Organization. 19 May 2022. https://www.who.int/news-room/fact-sheets/detail/monkeypox. Retrieved 28 May 2022.
- ↑ Sreenivas, Shishira (28 June 2022). "Monkeypox: What to Know". WebMD. https://www.webmd.com/a-to-z-guides/monkeypox-what-know.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 "Signs and Symptoms Monkeypox". 11 May 2015. https://www.cdc.gov/poxvirus/monkeypox/symptoms.html.
- ↑ 6.0 6.1 6.2 6.3 Petersen, Eskild; Kantele, Anu; Koopmans, Marion; Asogun, Danny; Yinka-Ogunleye, Adesola; Ihekweazu, Chikwe; Zumla, Alimuddin (December 2019). "Human Monkeypox: Epidemiologic and Clinical Characteristics, Diagnosis, and Prevention". Infectious Disease Clinics of North America 33 (4): 1027–1043. doi:10.1016/j.idc.2019.03.001. PMID 30981594.
- ↑ 7.0 7.1 7.2 7.3 7.4 "About Monkeypox | Monkeypox | Poxvirus | CDC". 2021-11-22. https://www.cdc.gov/poxvirus/monkeypox/about.html.
- ↑ 8.0 8.1 "2003 U.S. Outbreak Monkeypox". 11 May 2015. https://www.cdc.gov/poxvirus/monkeypox/outbreak.html.
- ↑ 9.0 9.1 9.2 9.3 "Human monkeypox". Clinical Infectious Diseases 58 (2): 260–267. January 2014. doi:10.1093/cid/cit703. PMID 24158414.
- ↑ "Monkeypox and Smallpox Vaccine Guidance". 29 November 2019. https://www.cdc.gov/poxvirus/monkeypox/clinicians/smallpox-vaccine.html. Retrieved 20 May 2022.
- ↑ "Infection Control: Hospital Monkeypox". 22 May 2022. https://www.cdc.gov/poxvirus/monkeypox/clinicians/infection-control-hospital.html. Retrieved 24 May 2022.
- ↑ 12.0 12.1 "Interim Clinical Guidance for the Treatment of Monkeypox | Monkeypox | Poxvirus | CDC". 26 May 2022. https://www.cdc.gov/poxvirus/monkeypox/treatment.html. Retrieved 8 June 2022.
- ↑ 13.0 13.1 13.2 13.3 13.4 "Monkeypox". 24 May 2022. https://www.gov.uk/guidance/monkeypox.
- ↑ 14.0 14.1 Simpson, Karl; Heymann, David; Brown, Colin S.; Edmunds, W. John; Elsgaard, Jesper; Fine, Paul et al. (14 July 2020). "Human monkeypox – After 40 years, an unintended consequence of smallpox eradication". Vaccine 38 (33): 5077–5081. doi:10.1016/j.vaccine.2020.04.062. PMID 32417140.
- ↑ 15.0 15.1 15.2 "Multi-country monkeypox outbreak in non-endemic countries". https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON385.
- ↑ 16.0 16.1 Osorio, J.E.; Yuill, T.M. (2008). "Zoonoses". Encyclopedia of Virology. pp. 485–495. doi:10.1016/B978-012374410-4.00536-7. ISBN 9780123744104.
- ↑ Sutcliffe, Catherine G.; Rimone, Anne W.; Moss, William J. (2020). "32.2. Poxviruses". in Ryan, Edward T.; Hill, David R.; Solomon, Tom et al.. Hunter's Tropical Medicine and Emerging Infectious Diseases E-Book (Tenth ed.). Edinburgh: Elsevier. pp. 272–277. ISBN 978-0-323-55512-8. https://books.google.com/books?id=y8SODwAAQBAJ&dq=monkeypox+nigeria&pg=PA272.
- ↑ Harris, Emily (27 May 2022). "What to Know About Monkeypox". JAMA 327 (23): 2278–2279. doi:10.1001/jama.2022.9499. PMID 35622356.
- ↑ "Multi-country monkeypox outbreak in non-endemic countries". 21 May 2022. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON385.
- ↑ "Monkeypox: experts give virus variants new names". 2022-08-12. https://www.who.int/news/item/12-08-2022-monkeypox--experts-give-virus-variants-new-names.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 Adler, Hugh; Gould, Susan; Hine, Paul; Snell, Luke B.; Wong, Waison; Houlihan, Catherine F. et al. (24 May 2022). "Clinical features and management of human monkeypox: a retrospective observational study in the UK". The Lancet. Infectious Diseases 22 (8): S1473–3099(22)00228–6. doi:10.1016/S1473-3099(22)00228-6. PMID 35623380.
- ↑ 22.0 22.1 "Transmission Monkeypox". 11 May 2015. https://www.cdc.gov/poxvirus/monkeypox/transmission.html.
- ↑ "Treatment Monkeypox Poxvirus CDC". 28 December 2018. https://www.cdc.gov/poxvirus/monkeypox/clinicians/treatment.html.
- ↑ Fine, P. E.; Jezek, Z.; Grab, B.; Dixon, H. (September 1988). "The transmission potential of monkeypox virus in human populations". International Journal of Epidemiology 17 (3): 643–650. doi:10.1093/ije/17.3.643. ISSN 0300-5771. PMID 2850277. https://pubmed.ncbi.nlm.nih.gov/2850277/.
- ↑ "Prevention". 29 November 2019. https://www.cdc.gov/poxvirus/monkeypox/prevention.html. Retrieved 14 May 2022.
- ↑ "Multi-country monkeypox outbreak in non-endemic countries: Update" (in en). https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON388.
- ↑ 27.0 27.1 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "19. Viral diseases". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. p. 389. ISBN 978-0-323-54753-6. https://books.google.com/books?id=UEaEDwAAQBAJ&dq=human&pg=PA389.
- ↑ 28.0 28.1 28.2 28.3 28.4 28.5 28.6 Bunge, Eveline M.; Hoet, Bernard; Chen, Liddy; Lienert, Florian; Weidenthaler, Heinz; Baer, Lorraine R.; Steffen, Robert (11 February 2022). "The changing epidemiology of human monkeypox – A potential threat? A systematic review". PLOS Neglected Tropical Diseases 16 (2): e0010141. doi:10.1371/journal.pntd.0010141. PMID 35148313.
- ↑ "Monkeypox". 11 May 2015. https://www.cdc.gov/poxvirus/monkeypox/index.html.
- ↑ "Monkeypox outbreak: List of countries with reported cases". https://gulfnews.com/special-reports/monkeypox-outbreak-list-of-countries-with-reported-cases-1.1653054419477.
- ↑ "Viruela del mono: confirmaron el primer caso del virus en el país" (in es). 26 May 2022. https://www.lanacion.com.ar/sociedad/viruela-del-mono-confirmaron-el-primer-caso-del-virus-en-el-pais-nid26052022/.
- ↑ Efrati, Ido. "Israel Confirms First Case of Monkeypox Virus". Haaretz. https://www.haaretz.com/israel-news/israel-discovers-first-case-of-monkeypox-virus-1.10812439.
- ↑ "UAE reports first case of monkeypox in the country". 24 May 2022. https://english.alarabiya.net/News/gulf/2022/05/24/UAE-reports-first-case-of-monkeypox-in-the-country.
- ↑ "Monkeypox cases investigated in Europe, the United States, Canada and Australia". BBC News. 20 May 2022. https://www.bbc.co.uk/news/health-61506562.
- ↑ "Singapore confirms imported case of monkeypox after flight attendant develops fever and rashes". https://www.channelnewsasia.com/singapore/monkeypox-singapore-imported-case-flight-attendant-fever-rashes-moh-2760996.
- ↑ "Morocco Reports First Monkeypox Case". https://www.moroccoworldnews.com/2022/06/349441/morocco-reports-first-monkeypox-case.
- ↑ Grover, Natalie; Revill, John; Rigby, Jennifer (23 July 2022). "Monkeypox outbreak constitutes global health emergency – WHO". https://www.reuters.com/business/healthcare-pharmaceuticals/monkeypox-outbreak-constitutes-global-health-emergency-who-2022-07-23/.
- ↑ "Asymptomatic monkeypox infection detected from routine sexual health samples" (in en). 2022-07-07. https://www.news-medical.net/news/20220707/Asymptomatic-monkeypox-infection-detected-from-routine-sexual-health-samples.aspx.
- ↑ 39.0 39.1 39.2 39.3 39.4 "Emerging diseases-the monkeypox epidemic in the Democratic Republic of the Congo". Clinical Microbiology and Infection 22 (8): 658–659. August 2016. doi:10.1016/j.cmi.2016.07.004. PMID 27404372.
- ↑ Gilbourne, Marika; Coulson, Ian; Mitchell, Gus (May 2022). "Monkeypox: Symptoms, Treatment, and Outcome — DermNet". in Amanda Oakley. https://dermnetnz.org/topics/monkeypox.
- ↑ "WHO Factsheet - Monkeypox". World Health Organization. 19 May 2022. https://www.who.int/news-room/fact-sheets/detail/monkeypox. Retrieved 28 May 2022.
- ↑ "Emerging diseases-the monkeypox epidemic in the Democratic Republic of the Congo". Clinical Microbiology and Infection 22 (8): 658–659. August 2016. doi:10.1016/j.cmi.2016.07.004. PMID 27404372.
- ↑ "New Monkeypox Symptoms Are Making Cases Harder to Recognize" (in en). Bloomberg.com. 2022-07-21. https://www.bloomberg.com/news/articles/2022-07-21/monkeypox-symptom-patterns-confound-doctors-in-global-outbreak.
- ↑ Gilbourne, Marika; Coulson, Ian; Mitchell, Gus (May 2022). "Monkeypox: Symptoms, Treatment, and Outcome — DermNet". in Amanda Oakley. https://dermnetnz.org/topics/monkeypox.
- ↑ "Monkeypox - United Kingdom of Great Britain and Northern Ireland". https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON383.
- ↑ 46.0 46.1 46.2 46.3 Patel, Aatish; Bilinska, Julia; Tam, Jerry C. H.; Fontoura, Dayana Da Silva; Mason, Claire Y.; Daunt, Anna; Snell, Luke B.; Murphy, Jamie et al. (2022-07-28). "Clinical features and novel presentations of human monkeypox in a central London centre during the 2022 outbreak: descriptive case series" (in en). BMJ 378: e072410. doi:10.1136/bmj-2022-072410. ISSN 1756-1833. PMID 35902115. PMC 9331915. https://www.bmj.com/content/378/bmj-2022-072410.
- ↑ CDC (2022-08-05). "Monkeypox in the U.S." (in en-us). https://www.cdc.gov/poxvirus/monkeypox/symptoms/index.html.
- ↑ 48.0 48.1 48.2 48.3 48.4 48.5 48.6 48.7 Nash, Sherrie L.; Palmer, Sally B.; Wingfield, Wayne E. (2009). "1.11. Zoonoses and zoonotic diseases". in Wingfield, Wayne E.; Palmer, Sally B.. Veterinary Disaster Response. Iowa: John Wiley & Sons. pp. 167–168. ISBN 978-0-8138-1014-0. https://books.google.com/books?id=kffqobiSuqAC&dq=monkeypo&pg=PA167.
- ↑ "Monkeypox in the U.S.". 12 August 2022. https://www.cdc.gov/poxvirus/monkeypox/veterinarian/monkeypox-in-animals.html.
- ↑ "The Ultimate Guide to Monkeypox". 29 September 2022. https://killem.com.sg/blog/the-ultimate-guide-to-monkeypox/.
- ↑ 51.0 51.1 51.2 "Examining Animals With Suspected Monkeypox | Monkeypox | Poxvirus | CDC". CDC. 19 November 2019. https://www.cdc.gov/poxvirus/monkeypox/veterinarian/examination.html. Retrieved 24 May 2022.
- ↑ Abbasi, Saman. "What is Monkeypox? Symptoms, Causes, Treatment And Prevention". YourDoctorsOnline. https://yourdoctors.online/monkeypox-causes-symptoms-and-prevention/.
- ↑ Falendysz, Elizabeth A.; Lopera, Juan G.; Lorenzsonn, Faye; Salzer, Johanna S.; Hutson, Christina L.; Doty, Jeffrey; Gallardo-Romero, Nadia; Carroll, Darin S. et al. (30 October 2015). "Further Assessment of Monkeypox Virus Infection in Gambian Pouched Rats (Cricetomys gambianus) Using In Vivo Bioluminescent Imaging". PLOS Neglected Tropical Diseases 9 (10): e0004130. doi:10.1371/journal.pntd.0004130. PMID 26517839.
- ↑ 54.0 54.1 54.2 54.3 "Transmission". 11 May 2015. https://www.cdc.gov/poxvirus/monkeypox/transmission.html.
- ↑ "Monkeypox multi-country outbreak - RAPID RISK ASSESSMENT". https://www.ecdc.europa.eu/sites/default/files/documents/risk-assessment-monkeypox-multi-country-outbreak.pdf.
- ↑ 56.0 56.1 Lapa, Daniele; Carletti, Fabrizio; Mazzotta, Valentina; Matusali, Giulia; Pinnetti, Carmela; Meschi, Silvia; Gagliardini, Roberta; Colavita, Francesca et al. (2 August 2022). "Monkeypox virus isolation from a semen sample collected in the early phase of infection in a patient with prolonged seminal viral shedding". Lancet Infectious Diseases. doi:10.1016/S1473-3099(22)00513-8. PMID 35931095. https://doi.org/10.1016/S1473-3099(22)00513-8. Retrieved 3 August 2022.
- ↑ Vaughan, Aisling; Aarons, Emma; Astbury, John; Brooks, Tim; Chand, Meera; Flegg, Peter et al. (April 2020). "Human-to-Human Transmission of Monkeypox Virus, United Kingdom, October 2018" (in en-us). Emerging Infectious Diseases 26 (4): 782–785. doi:10.3201/eid2604.191164. PMID 32023204. PMC 7101111. https://wwwnc.cdc.gov/eid/article/26/4/19-1164_article.
- ↑ Kozlov, Max (2 June 2022). "Monkeypox goes global: why scientists are on alert". Nature 606 (7912): 15–16. doi:10.1038/d41586-022-01421-8. PMID 35595996.
- ↑ Le Page, Michael. "First monkeypox genome from latest outbreak shows links to 2018 strain". https://www.newscientist.com/article/2321407-first-monkeypox-genome-from-latest-outbreak-shows-links-to-2018-strain/.
- ↑ Philpott, David (2022). "Epidemiologic and Clinical Characteristics of Monkeypox Cases — United States, May 17–July 22, 2022" (in en-us). MMWR. Morbidity and Mortality Weekly Report 71. doi:10.15585/mmwr.mm7132e3. ISSN 0149-2195. https://www.cdc.gov/mmwr/volumes/71/wr/mm7132e3.htm.
- ↑ Thornhill, John P.; Barkati, Sapha; Walmsley, Sharon; Rockstroh, Juergen; Antinori, Andrea; Harrison, Luke B.; Palich, Romain; Nori, Achyuta et al. (2022-08-25). "Monkeypox Virus Infection in Humans across 16 Countries — April–June 2022" (in en). New England Journal of Medicine 387 (8): 679–691. doi:10.1056/NEJMoa2207323. ISSN 0028-4793. http://www.nejm.org/doi/10.1056/NEJMoa2207323.
- ↑ Tarín-Vicente, Eloy José; Alemany, Andrea; Agud-Dios, Manuel; Ubals, Maria; Suñer, Clara; Antón, Andrés; Arando, Maider; Arroyo-Andrés, Jorge et al. (2022-08-27). "Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: a prospective observational cohort study" (in English). The Lancet 400 (10353): 661–669. doi:10.1016/S0140-6736(22)01436-2. ISSN 0140-6736. PMID 35952705. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)01436-2/abstract.
- ↑ "Many monkeypox cases among men living with HIV, but no sign yet of poorer outcomes" (in en). https://www.aidsmap.com/news/aug-2022/many-monkeypox-cases-among-men-living-hiv-no-sign-yet-poorer-outcomes.
- ↑ pharmacyinfoline (2022-08-22). "Monkeypox testing kit: India's first kit by Mumbai-based Transasia Bio-Medicals" (in en-US). https://pharmacyinfoline.com/disease/monkeypox-testing-kit/.
- ↑ Marriott, Kathleen A.; Parkinson, Christopher V.; Morefield, Samantha I.; Davenport, Robert; Nichols, Richard; Monath, Thomas P. (January 2008). "Clonal vaccinia virus grown in cell culture fully protects monkeys from lethal monkeypox challenge". Vaccine 26 (4): 581–588. doi:10.1016/j.vaccine.2007.10.063. PMID 18077063.
- ↑ "Monkeypox vaccines in pregnancy: lessons must be learned from COVID-19". The Lancet. Global Health 10 (9): e1230–e1231. June 2022. doi:10.1016/S2214-109X(22)00284-4. PMID 35772413.
- ↑ "Infection Control: Hospital | Monkeypox | Poxvirus | CDC". 2019-01-03. https://www.cdc.gov/poxvirus/monkeypox/clinicians/infection-control-hospital.html.
- ↑ 68.0 68.1 Scalvini, Marco (2022-09-14). "Monkeypox: patients, clinicians, and the need for shared responsibility" (in en). BMJ 378: o2221. doi:10.1136/bmj.o2221. ISSN 1756-1833. PMID 36104032. https://www.bmj.com/content/378/bmj.o2221.
- ↑ "Tecovirimat SIGA". European Medicines Agency. 28 January 2022. https://www.ema.europa.eu/en/medicines/human/EPAR/tecovirimat-siga.
- ↑ "Poxvirus infection (monkeypox and smallpox) - Treatment algorithm | BMJ Best Practice". https://bestpractice.bmj.com/topics/en-gb/1611/treatment-algorithm.
- ↑ "A human infection caused by monkeypox virus in Basankusu Territory, Democratic Republic of the Congo". Bulletin of the World Health Organization 46 (5): 593–597. 1972. PMID 4340218.
- ↑ 72.0 72.1 72.2 72.3 72.4 72.5 "Emergence of Monkeypox as the Most Important Orthopoxvirus Infection in Humans". Frontiers in Public Health 6: 241. September 2018. doi:10.3389/fpubh.2018.00241. PMID 30234087.
- ↑ Heymann, D. L.; Szczeniowski, M.; Esteves, K. (1 January 1998). "Re-emergence of monkeypox in Africa: a review of the past six years". British Medical Bulletin 54 (3): 693–702. doi:10.1093/oxfordjournals.bmb.a011720. PMID 10326294.
- ↑ "Monkeypox fact sheet". World Health Organization. 19 May 2022. https://www.who.int/news-room/fact-sheets/detail/monkeypox.
- ↑ "Monkeypox: Four more cases detected in England". 17 May 2022. https://www.bbc.co.uk/news/health-61470940.
- ↑ "What You Should Know About Monkeypox". Fact Sheet. Centers for Disease Control and Prevention. 2003-06-12. https://www.cdc.gov/ncidod/monkeypox/pdf/factsheet2.pdf.
- ↑ "Discovery of monkeypox in Sudan". The New England Journal of Medicine 355 (9): 962–963. August 2006. doi:10.1056/NEJMc060792. PMID 16943415.
- ↑ "Phylogenetic and ecologic perspectives of a monkeypox outbreak, southern Sudan, 2005". Emerging Infectious Diseases 19 (2): 237–245. February 2013. doi:10.3201/eid1902.121220. PMID 23347770.
- ↑ Anderson, Michael G.; Frenkel, Lawrence D.; Homann, Scott; Guffey, Jennifer (December 2003). "A case of severe monkeypox virus disease in an American child: emerging infections and changing professional values". The Pediatric Infectious Disease Journal 22 (12): 1093–1096. doi:10.1097/01.inf.0000101821.61387.a5. PMID 14688573.
- ↑ "Medscape Monkeypox Review". Bcbsma.medscape.com. http://bcbsma.medscape.com/viewarticle/458671_11.
- ↑ "Monkeypox in the United States | Monkeypox | Poxvirus | CDC". 2021-11-19. https://www.cdc.gov/poxvirus/monkeypox/outbreak/us-outbreaks.html.
- ↑ 82.0 82.1 Centers for Disease Control Prevention (CDC) (11 July 2003). "Update: multistate outbreak of monkeypox--Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003.". Morbidity and Mortality Weekly Report 52 (27): 642–646. PMID 12855947. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5227a5.htm.
- ↑ 83.0 83.1 Tomori, Oyewale. "Monkeypox in Nigeria: why the disease needs intense management". http://theconversation.com/monkeypox-in-nigeria-why-the-disease-needs-intense-management-165022.
- ↑ Yinka-Ogunleye, Adesola; Aruna, Olusola; Dalhat, Mahmood; Ogoina, Dimie; McCollum, Andrea; Disu, Yahyah; Mamadu, Ibrahim; Akinpelu, Afolabi et al. (2019-08-01). "Outbreak of human monkeypox in Nigeria in 2017–18: a clinical and epidemiological report". The Lancet Infectious Diseases 19 (8): 872–879. doi:10.1016/S1473-3099(19)30294-4. PMID 31285143.
- ↑ Ogoina, Dimie; Izibewule, James Hendris; Ogunleye, Adesola; Ederiane, Ebi; Anebonam, Uchenna; Neni, Aworabhi; Oyeyemi, Abisoye; Etebu, Ebimitula Nicholas et al. (2019-04-17). "The 2017 human monkeypox outbreak in Nigeria—Report of outbreak experience and response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria". PLOS ONE 14 (4): e0214229. doi:10.1371/journal.pone.0214229. PMID 30995249. Bibcode: 2019PLoSO..1414229O.
- ↑ "Monkeypox in Nigeria – Watch – Level 1, Practice Usual Precautions – Travel Health Notices". https://wwwnc.cdc.gov/travel/notices/watch/monkeypox-nigeria.
- ↑ "Monkeypox – Nigeria". WHO. 21 December 2017. https://www.who.int/csr/don/21-december-2017-monkeypox-nigeria/en/.
- ↑ "Monkeypox – Nigeria". WHO. 5 October 2018. https://www.who.int/csr/don/05-october-2018-monkeypox-nigeria/en/.
- ↑ 89.0 89.1 "Monkeypox – Singapore". WHO. 16 May 2019. https://www.who.int/csr/don/16-may-2019-monkeypox-singapore/en/.
- ↑ "Monthly Update on Monkeypox (MPX) in Nigeria, Epi-week: 8, February 28, 2022 – Nigeria | ReliefWeb". https://reliefweb.int/report/nigeria/monthly-update-monkeypox-mpx-nigeria-epi-week-8-february-28-2022.
- ↑ "Monkeypox in Nigeria". https://wwwnc.cdc.gov/travel/notices/watch/monkeypox-nigeria.
- ↑ "See the unusual places where monkeypox cases have popped up this month". https://www.nbcnews.com/health/health-news/map-countries-confirmed-monkeypox-cases-2022-outbreak-rcna30124.
- ↑ Ileyemi, Mariam (2022-05-10). "Monkeypox: Nigeria records 558 cases, eight deaths in five years". https://www.premiumtimesng.com/news/top-news/528825-monkeypox-nigeria-records-558-cases-eight-deaths-in-five-years.html.
- ↑ "First ever case of monkeypox recorded in the UK". The Guardian. 8 September 2018. https://www.theguardian.com/uk-news/2018/sep/08/first-ever-case-of-monkeypox-recorded-in-the-uk.
- ↑ "Monkeypox case in England". gov.uk. 8 September 2018. https://www.gov.uk/government/news/monkeypox-case-in-england.
- ↑ "Blackpool monkeypox case confirmed as second in UK". BBC News. 11 September 2018. https://www.bbc.co.uk/news/uk-england-lancashire-45490444.
- ↑ "Two cases of monkeypox imported to the United Kingdom, September 2018". Euro Surveillance 23 (38). September 2018. doi:10.2807/1560-7917.es.2018.23.38.1800509. PMID 30255836.
- ↑ Gayle, Damien (26 September 2018). "Medic becomes third person infected with monkeypox in England". https://www.theguardian.com/society/2018/sep/26/medic-becomes-third-person-infected-with-monkeypox-in-england.
- ↑ "Monkeypox case confirmed in England". Public Health England. 4 December 2019. https://www.gov.uk/government/news/monkeypox-case-confirmed-in-england.
- ↑ "News Scan for May 09, 2019, Singapore sees first monkeypox case – in Nigerian national". Center for Infectious Disease Research and Policy, University of Minnesota. http://www.cidrap.umn.edu/news-perspective/2019/05/news-scan-may-09-2019.
- ↑ "Communicable disease threats report, Week 26, 27 June – 3 July 2021". 2 July 2021. https://www.ecdc.europa.eu/sites/default/files/documents/Communicable-disease-threats-report-3-july-2021.pdf.
- ↑ "Monkeypox 'outbreak' in north Wales as two treated for rare viral infection". ITV. 10 June 2021. https://www.itv.com/news/2021-06-10/monkeypox-outbreak-in-north-wales-as-two-treated-for-rare-viral-infection.
- ↑ "A Case of Monkeypox in a Returned Traveler". https://www.proquest.com/openview/78527319ec56ca1a4f45974d0a55d86d/1?pq-origsite=gscholar&cbl=136156.
- ↑ Parker, Scott; Buller, R. Mark (2013-02-01). "A review of experimental and natural infections of animals with monkeypox virus between 1958 and 2012". Future Virology 8 (2): 129–157. doi:10.2217/fvl.12.130. ISSN 1746-0794. PMID 23626656.
- ↑ 105.0 105.1 Cho, C. T.; Wenner, H. A. (March 1973). "Monkeypox virus". Bacteriological Reviews 37 (1): 1–18. doi:10.1128/br.37.1.1-18.1973. PMID 4349404.
- ↑ "Human monkeypox, 1970–79". Bulletin of the World Health Organization 58 (2): 165–182. 1980. PMID 6249508.
- ↑ 107.0 107.1 "Outbreaks of disease suspected of being due to human monkeypox virus infection in the Democratic Republic of Congo in 2001". Journal of Clinical Microbiology 40 (8): 2919–2921. August 2002. doi:10.1128/JCM.40.8.2919-2921.2002. PMID 12149352.
- ↑ Monkeypox at eMedicine
- ↑ 109.0 109.1 Vaughan, A; Aarons, E; Astbury, J; Brooks, T; Chand, M; Flegg, P et al. (April 2020). "Human-to-Human Transmission of Monkeypox Virus, United Kingdom, October 2018.". Emerging Infectious Diseases 26 (4): 782–785. doi:10.3201/eid2604.191164. PMID 32023204.
- ↑ 110.0 110.1 Mauldin, Matthew R.; McCollum, Andrea M.; Nakazawa, Yoshinori J.; Mandra, Anna; Whitehouse, Erin R.; Davidson, Whitni et al. (19 April 2022). "Exportation of Monkeypox Virus From the African Continent". The Journal of Infectious Diseases 225 (8): 1367–1376. doi:10.1093/infdis/jiaa559. PMID 2880628.
- ↑ Critics say 'monkeypox' is a racist name. But it's not going away anytime soon
- ↑ "India's first monkeypox death: Kerala youth had tested positive abroad; probe ordered". Indianexpress.com. 31 July 2022. https://indianexpress.com/article/india/indias-first-monkeypox-death-kerala-youth-had-tested-positive-in-uae-probe-ordered-8062463/.
External links
- CDC – Monkeypox Fact Sheet
- WHO – Monkeypox Fact Sheet
- Virology.net Picturebook: Monkeypox
- "Could Monkeypox Take Over Where Smallpox Left Off? Smallpox may be gone, but its viral cousins – monkeypox and cowpox – are staging a comeback". Scientific American, March 4, 2013.
- More than 80 cases confirmed in 12 countries, May 23, 2022.
- Monkeypox DNA sequencing hints virus circulating since 2017, June 7, 2022.
- MonkeypoxTracker – Monkeypox statistics visualization site
- PoxApp - the monkeypox app – Assess skin lesions and symptoms with artificial intelligence developed by Stanford University
| Classification |
|---|