Biology:Listeria
| Listeria | |
|---|---|

| |
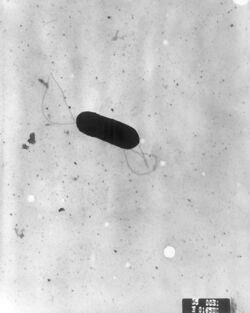
| micrograph of Listeria monocytogenes bacterium in tissue | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Bacillota |
| Class: | Bacilli |
| Order: | Bacillales |
| Family: | Listeriaceae |
| Genus: | Listeria Pirie 1940 |
| Species | |
|
L. aquatica | |
Listeria is a genus of bacteria that acts as an intracellular parasite in mammals. Until 1992, 10 species were known,[1][2] each containing two subspecies. By 2020, 21 species had been identified.[3] The genus is named in honour of the British pioneer of sterile surgery Joseph Lister. Listeria species are Gram-positive, rod-shaped, and facultatively anaerobic, and do not produce endospores.[4] The major human pathogen in the genus Listeria is L. monocytogenes. It is usually the causative agent of the relatively rare bacterial disease listeriosis, an infection caused by eating food contaminated with the bacteria. Listeriosis can cause serious illness in pregnant women, newborns, adults with weakened immune systems and the elderly, and may cause gastroenteritis in others who have been severely infected.
Listeriosis is a serious disease for humans; the overt form of the disease has a case-fatality rate of around 20–30%. The two main clinical manifestations are sepsis and meningitis. Meningitis is often complicated by encephalitis, when it is known as meningoencephalitis, a pathology that is unusual for bacterial infections. L. ivanovii is a pathogen of mammals, specifically ruminants, and has rarely caused listeriosis in humans.[5] The incubation period can vary from three to 70 days.[6]
Background
The first documented human case of listeriosis was in 1929 described by the Danish physician Aage Nyfeldt ("Etiologie de la mononucleose infectieuse,” Comptes Rendus des Seances de la Societe de Biologie, vol. 101, pp. 590–591, 1929). In the late 1920s, two researchers independently identified L. monocytogenes from animal outbreaks. They proposed the genus Listerella in honour of surgeon and early antiseptic advocate Joseph Lister, but that name was already in use for a slime mould and a protozoan. Eventually, the genus Listeria was proposed and accepted. All species within the genus Listeria are Gram-positive, catalase-positive rods and do not produce endospores. The genus Listeria was classified in the family Corynebacteriaceae through the seventh edition (1957) of Bergey's Manual of Systematic Bacteriology. The 16S rRNA cataloging studies of Stackebrandt, et al. demonstrated that L. monocytogenes is a distinct taxon within the Lactobacillus-Bacillus branch of the bacterial phylogeny constructed by Woese. In 2004, the genus was placed in the newly created family Listeriaceae. The only other genus in the family is Brochothrix.[7]
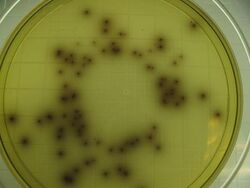
The genus Listeria (As of 2020) is known to contain 21 species: L. aquatica, L. booriae, L. cornellensis, L. costaricensis, L. goaensis, L. fleischmannii, L. floridensis, L. grandensis, L. grayi, L. innocua, L. ivanovii, L. marthii, L. monocytogenes, L. newyorkensis, L. riparia, L. rocourtiae, L. seeligeri, L. thailandensis, L. valentina, L. weihenstephanensis, and L. welshimeri.[8][9][10] Listeria dinitrificans, previously thought to be part of the genus Listeria, was reclassified into the new genus Jonesia.[11] Under the microscope, Listeria species appear as small rods, which are sometimes arranged in short chains. In direct smears, they may be coccoid, and can be mistaken for streptococci. Longer cells may resemble corynebacteria. Flagella are produced at room temperature, but not at 37 °C. Hemolytic activity on blood agar has been used as a marker to distinguish L. monocytogenes from other Listeria species, but it is not an absolutely definitive criterion. Further biochemical characterization may be necessary to distinguish between the different species of Listeria.[citation needed]
Listeria can be found in soil, which can lead to vegetable contamination. Animals can be carriers. Listeria has been found in uncooked meats, uncooked vegetables, fruits including cantaloupe[12] and apples,[13] pasteurized or unpasteurized milk, foods made from milk, and processed foods. Pasteurization and sufficient cooking kill Listeria; however, contamination may occur after cooking and before packaging. For example, meat-processing plants producing ready-to-eat foods, such as hot dogs and deli meats, must follow extensive sanitation policies and procedures to prevent Listeria contamination.[14] Listeria monocytogenes is commonly found in soil, stream water, sewage, plants, and food.[15] Listeria is responsible for listeriosis, a rare but potentially lethal foodborne illness. The case fatality rate for those with a severe form of infection may approach 25%.[16] (Salmonellosis, in comparison, has a mortality rate estimated at less than 1%.[17]) Although L. monocytogenes has low infectivity, it is hardy and can grow in temperatures from 4 °C (39.2 °F) (the temperature of a refrigerator) to 37 °C (98.6 °F), (the body's internal temperature).[15] Listeriosis is a serious illness, and the disease may manifest as meningitis, or affect newborns due to its ability to penetrate the endothelial layer of the placenta.[16]
Pathogenesis
Listeria uses the cellular machinery to move around inside the host cell. It induces directed polymerization of actin by the ActA transmembrane protein, thus pushing the bacterial cell around.[18]
Listeria monocytogenes, for example, encodes virulence genes that are thermoregulated. The expression of virulence factor is optimal at 39 °C, and is controlled by a transcriptional activator, PrfA, whose expression is thermoregulated by the PrfA thermoregulator UTR element. At low temperatures, the PrfA transcript is not translated due to structural elements near the ribosome binding site. As the bacteria infect the host, the temperature of the host denatures the structure and allows translation initiation for the virulent genes.[citation needed]
The majority of Listeria bacteria are attacked by the immune system before they are able to cause infection. Those that escape the immune system's initial response, however, spread through intracellular mechanisms, which protects them from circulating immune factors (AMI).[16]
To invade, Listeria induces macrophage phagocytic uptake by displaying D-galactose in their teichoic acids that are then bound by the macrophage's polysaccharides. Other important adhesins are the internalins.[17] Listeria uses internalin A and B to bind to cellular receptors. Internalin A binds to E-cadherin, while internalin B binds to the cell's Met receptors. If both of these receptors have a high enough affinity to Listeria's internalin A and B, then it will be able to invade the cell via an indirect zipper mechanism.[citation needed] Once phagocytosed, the bacterium is encapsulated by the host cell's acidic phagolysosome organelle.[15] Listeria, however, escapes the phagolysosome by lysing the vacuole's entire membrane with secreted hemolysin,[19] now characterized as the exotoxin listeriolysin O.[15] The bacteria then replicate inside the host cell's cytoplasm.[16]
Listeria must then navigate to the cell's periphery to spread the infection to other cells. Outside the body, Listeria has flagellar-driven motility, sometimes described as a "tumbling motility". However, at 37 °C, flagella cease to develop and the bacterium instead usurps the host cell's cytoskeleton to move.[16] Listeria, inventively, polymerizes an actin tail or "comet",[19] from actin monomers in the host's cytoplasm[20] with the promotion of virulence factor ActA.[16] The comet forms in a polar manner[21] and aids the bacterial migration to the host cell's outer membrane. Gelsolin, an actin filament severing protein, localizes at the tail of Listeria and accelerates the bacterium's motility.[21] Once at the cell surface, the actin-propelled Listeria pushes against the cell's membrane to form protrusions called filopods[15] or "rockets". The protrusions are guided by the cell's leading edge[22] to contact adjacent cells, which then engulf the Listeria rocket and the process is repeated, perpetuating the infection.[16] Once phagocytosed, the bacterium is never again extracellular: it is an intracellular parasite[19] like S. flexneri, Rickettsia spp., and C. trachomatis.[16]
Epidemiology
The Center for Science in the Public Interest has published a list of foods that have sometimes caused outbreaks of Listeria: hot dogs, deli meats, milk (even if pasteurized), cheeses (particularly soft-ripened cheeses such as feta, Brie, Camembert, blue-veined, or Mexican-style queso blanco), raw and cooked poultry, raw meats, ice cream, raw fruit,[23] vegetables, and smoked fish.[24] Cold-cut meats were implicated in an outbreak in Canada in 2008; improperly handled cantaloupe was implicated in both the outbreak of listeriosis from Jensen Farms in Colorado in 2011,[25] and a similar listeriosis outbreak across eastern Australia in early 2018.[26][27] 35 people died across these two outbreaks.[25][28] The Australian company GMI Food Wholesalers was fined A$236,000 for providing L. monocytogenes-contaminated chicken wraps to the airline Virgin Blue in 2011.[29] Caramel apples have also been cited as a source of listerial infections which hospitalized 26 people, of whom five died.[30][31] In 2019, the United Kingdom experienced nine cases of the disease, of which six[32] were fatal, in an outbreak caused by contaminated meat (produced by North Country Cooked Meats) in hospital sandwiches.[33] In 2019, two people in Australia died after probably eating smoked salmon and a third fell ill but survived the disease.[34] In September 2019, three deaths and a miscarriage were reported in the Netherlands after the consumption of listeria-infected deli meats produced by Offerman.[35]
Prevention
Preventing listeriosis as a foodborne illness requires effective sanitation of food contact surfaces.[36] Ethanol is an effective topical sanitizer against Listeria. Quaternary ammonium can be used in conjunction with alcohol as a food-contact safe sanitizer with increased duration of the sanitizing action.
Keeping foods in the home refrigerated below 4 °C (39 °F) discourages bacterial growth. Unpasteurized dairy products may pose a risk.[37] Cooking all meats (including beef, pork, poultry, and seafood) to a safe internal temperature, typically 73 °C (165 °F), will kill the food-borne pathogen.[38]
Treatment
Non-invasive listeriosis: bacteria are retained within the digestive tract. Symptoms are mild, lasting only a few days and requiring only supportive care. Muscle pain and fever can be treated with over-the-counter pain relievers; diarrhea and gastroenteritis can be treated with over-the-counter medications.[38]
Invasive listeriosis: bacteria have spread to the bloodstream and central nervous system. Treatment includes intravenous delivery of high-dose antibiotics and hospital in-patient care of (probably) not less than two weeks stay, depending on the extent of the infection.[38] Ampicillin, penicillin, or amoxicillin are typically administered for invasive listeriosis; gentamicin may be added in cases of patients with compromised immune systems.[39] In cases of allergy to penicillin, trimethoprim-sulfamethoxazole, vancomycin, and fluoroquinolones may be used.[39] For effective treatment the antibiotic must penetrate the host cell and bind to penicillin-binding protein 3 (PBP3). Cephalosporins are not effective for treating listeriosis.[39]
In cases of pregnancy, prompt treatment is critical to prevent bacteria from infecting the fetus; antibiotics may be given to pregnant women even in non-invasive listeriosis.[40] Mirena Nikolova, et al., states that applying antibiotics is crucial during the third trimester because cell-mediated immunity is reduced during this time. Pfaff and Tillet say that listeriosis can cause long-term consequences—including meningitis, preterm labor, newborn sepsis, stillbirths—when contracted during pregnancy. Oral therapies in less severe cases may include amoxicillin or erythromycin.[39] Higher doses may be given to pregnant women to ensure penetration of the umbilical cord and placenta.[41] Infected pregnant women may receive ultrasound scans to monitor the health of the fetus.
Asymptomatic patients who have been exposed to Listeria typically are not treated, but are informed of the signs and symptoms of the disease and advised to return for treatment if any develop.[38]
Research
Some Listeria species are opportunistic pathogens: L. monocytogenes is most prevalent in the elderly, pregnant mothers, and patients infected with HIV. With improved healthcare leading to a growing elderly population and extended life expectancies for HIV infected patients, physicians are more likely to encounter this otherwise-rare infection (only seven per 1,000,000 healthy people are infected with virulent Listeria each year).[15] Better understanding the cell biology of Listeria infections, including relevant virulence factors, may lead to better treatments for listeriosis and other intracytoplasmic parasite infections.
In oncology, researchers are investigating the use of Listeria as a cancer vaccine, taking advantage of its "ability to induce potent innate and adaptive immunity" by activating gamma delta T cells. [20][42]
See also
- 2008 Canada listeriosis outbreak
- 2011 United States listeriosis outbreak
- 2017–2018 South African listeriosis outbreak
- 2018 Australian rockmelon listeriosis outbreak
- List of foodborne illness outbreaks
References
- ↑ Jones, D. 1992. Current classification of the genus Listeria. In: Listeria 1992. Abstracts of ISOPOL XI, Copenhagen, Denmark). p. 7-8. ocourt, J., P. Boerlin, F.Grimont, C. Jacquet, and J-C. Piffaretti. 1992. Assignment of Listeria grayi and Listeria murrayi to a single species, Listeria grayi, with a revised description of Listeria grayi. Int. J. Syst. Bacteriol. 42:171-174.
- ↑ Boerlin et al. 1992. L. ivanovii subsp. londoniensis subsp. novi. Int. J. Syst. Bacteriol. 42:69-73. Jones, D., and H.P.R. Seeliger. 1986. International committee on systematic bacteriology. Subcommittee the taxonomy of Listeria. Int. J. Syst. Bacteriol. 36:117-118.
- ↑ Quereda, Juan J.; Leclercq, Alexandre; Moura, Alexandra; Vales, Guillaume; Gómez-Martín, Ángel; García-Muñoz, Ángel; Thouvenot, Pierre; Tessaud-Rita, Nathalie et al. (2020-10-05). "Listeria valentina sp. nov., isolated from a water trough and the faeces of healthy sheep" (in en). International Journal of Systematic and Evolutionary Microbiology 70 (11): 5868–5879. doi:10.1099/ijsem.0.004494. ISSN 1466-5026. PMID 33016862.
- ↑ Singleton P (1999). Bacteria in Biology, Biotechnology and Medicine (5th ed.). Wiley. pp. 444–454. ISBN 0-471-98880-4.
- ↑ Christelle Guillet, Olivier Join-Lambert, Alban Le Monnier, Alexandre Leclercq, Frédéric Mechaï, Marie-France Mamzer-Bruneel, Magdalena K. Bielecka, Mariela Scortti, Olivier Disson, Patrick Berche, José Vazquez-Boland, Olivier Lortholary, and Marc Lecuit. "Human Listeriosis Caused by Listeria ivanovii". Emerg Infect Dis. 2010 January; 16(1): 136–138.
- ↑ "Listeria". 12 April 2019. https://www.foodsafety.gov/poisoning/causes/bacteriaviruses/listeria/index.html.
- ↑ Elliot T. Ryser, Elmer H. Marth. Listeria, Listeriosis, and Food Safety. Second edition. Elmer Marth. 1999.
- ↑ Daniel Weller, Alexis Andrus, Martin Wiedmann and Henk C. den Bakker. Listeria booriae sp. nov. and Listeria newyorkensis sp. nov., from food processing environments in the USA. International Journal of Systematic and Evolutionary Microbiology (2015), 65, 286–292.
- ↑ Swapnil P. Doijad, Krupali V. Poharkar, Satyajit B. Kale, Savita Kerkar, Dewanand R. Kalorey, Nitin V. Kurkure, Deepak B. Rawool, Satya Veer Singh Malik, Rafed Yassin Ahmad, Martina Hudel, Sandeep P. Chaudhari, Birte Abt, Jörg Overmann, Markus Weigel, Torsten Hain, Sukhadeo B. Barbuddhe andTrinad Chakraborty. "Listeria goaensis sp. nov."International Journal of Systematic and Evolutionary Microbiology (2018),68: 3285-3291. doi: 10.1099/ijsem.0.002980.
- ↑ Leclercq, Alexandre; Moura, Alexandra; Vales, Guillaume; Tessaud-Rita, Nathalie; Aguilhon, Christine; Lecuit, Marc (2019). "Listeria thailandensis sp. nov.". International Journal of Systematic and Evolutionary Microbiology 69 (1): 74–81. doi:10.1099/ijsem.0.003097. PMID 30457511. https://hal-pasteur.archives-ouvertes.fr/pasteur-02319983/file/IJSEM_Lthailandensis_20181004%2Bfigs_HAL.pdf.
- ↑ M. D. Collins, S. Wallbanks, D. J. Lane, J. Shah, R. Nietupskin, J. Smida, M. Dorsch and E. Stackebrandt. Phylogenetic Analysis of the Genus Listeria Based on Reverse Transcriptase Sequencing of 16S rRNA. International Journal of Systematic and Evolutionary Microbiology. April 1991 vol. 41 no. 2 240–246
- ↑ "Listeria outbreak expected to cause more deaths across US in coming weeks". The Guardian (London). 29 September 2011. https://www.theguardian.com/world/2011/sep/29/listeria-outbreak-us-cantaloupe-melons?newsfeed=true.
- ↑ Times, Los Angeles (16 January 2015). "California plant issues massive apple recall due to listeria". http://www.latimes.com/food/dailydish/la-dd-california-farm-massive-apple-recall-listeria-found-20150116-story.html.
- ↑ "Controlling Listeria Contamination in Your Meat Processing Plant". Government of Ontario. 27 February 2007. http://www.omafra.gov.on.ca/english/food/inspection/meatinsp/controllinglisteria.htm.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 Southwick, F. S.; D. L. Purich. "More About Listeria". University of Florida Medical School. http://www.med.ufl.edu/biochem/DLPURICH/morelist.html. [No longer accessible. Archived version available here.]
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 16.6 16.7 "Todar's Online Textbook of Bacteriology". Listeria monocytogenes and Listeriosis. Kenneth Todar University of Wisconsin-Madison Department of Biology. 2003. http://textbookofbacteriology.net/Listeria.html.
- ↑ 17.0 17.1 "Statistics about Salmonella food poisoning". WrongDiagnosis.com. 27 February 2007. http://www.wrongdiagnosis.com/s/salmonella_food_poisoning/stats.htm.
- ↑ Smith, G. A.; Portnoy D. A. (July 1997). "Trends in Microbiology". How the Listeria Monocytogenes ActA Protein Converts Actin Polymerization into a Motile Force (Cell Press) 5 (7, number 7): 272–276. doi:10.1016/S0966-842X(97)01048-2. PMID 9234509.
- ↑ 19.0 19.1 19.2 Tinley, L. G. et al. (1989). "Actin Filaments and the Growth, Movement, and Spread of the Intracellular Bacterial Parasite, Listeria monocytogenes". The Journal of Cell Biology 109 (4 Pt 1): 1597–1608. doi:10.1083/jcb.109.4.1597. PMID 2507553. PMC 2115783. http://www.jcb.org/cgi/reprint/109/4/1597.
- ↑ 20.0 20.1 "Listeria". MicrobeWiki.Kenyon.edu. 16 August 2006. http://microbewiki.kenyon.edu/index.php?title=Listeria&oldid=5472.
- ↑ 21.0 21.1 Laine R. O.; Phaneuf K. L.; Cunningham C. C.; Kwiatkowski D.; Azuma T.; Southwick F. S. (1 August 1998). "Gelsolin, a protein that caps the barbed ends and severs actin filaments, enhances the actin-based motility of Listeria monocytogenes in host cells". Infect. Immun. 66 (8): 3775–82. doi:10.1128/IAI.66.8.3775-3782.1998. PMID 9673261.
- ↑ Galbraith C. G.; Yamada K. M.; Galbraith J. A. (February 2007). "Polymerizing actin fibers position integrins primed to probe for adhesion sites". Science 315 (5814): 992–5. doi:10.1126/science.1137904. PMID 17303755. Bibcode: 2007Sci...315..992G. https://zenodo.org/record/1230882.
- ↑ "Granny Smith, Gala apples recalled due to listeria". 16 January 2015. http://abc7news.com/food/granny-smith-gala-apples-recalled-due-to-listeria/478302/.
- ↑ Center for Science in the Public Interest – Nutrition Action Healthletter – Food Safety Guide – Meet the Bugs
- ↑ 25.0 25.1 William Neuman (27 September 2011). "Deaths From Cantaloupe Listeria Rise". The New York Times. https://www.nytimes.com/2011/09/28/business/deaths-from-cantaloupe-listeria-rises.html?_r=1.
- ↑ Claughton, David; Kontominas, Bellinda; Logan, Tyne (14 March 2018). "Rockmelon listeria: Rombola Family Farms named as source of outbreak" (in en-AU). Australian Broadcasting Corporation. http://www.abc.net.au/news/rural/2018-03-13/rockmelon-disaster-may-take-industry-years-to-recover/9543346.
- ↑ "Third death confirmed in Australia's rockmelon listeria outbreak". 3 March 2018. https://www.theguardian.com/australia-news/2018/mar/03/third-death-confirmed-in-australias-rockmelon-listeria-outbreak.
- ↑ "Fifth person dies as a result of rockmelon listeria outbreak" (in en-AU). Special Broadcasting Service. 16 March 2018. https://www.sbs.com.au/news/fifth-person-dies-as-a-result-of-rockmelon-listeria-outbreak.
- ↑ Josephine Tovey (16 November 2011). "$236,000 fine for foul flight chicken". The Sydney Morning Herald. http://www.smh.com.au/travel/travel-incidents/236000-fine-for-foul-flight-chicken-20111115-1nh99.html.
- ↑ "Warning: Prepackaged Caramel Apples Linked To 5 Deaths". Yahoo Health. December 19, 2014. https://www.yahoo.com/health/warning-prepackaged-caramel-apples-linked-to-5-105611703552.html.
- ↑ "Listeria outbreak from caramel apples has killed four". USA TODAY. December 20, 2014. https://www.usatoday.com/story/news/nation/2014/12/19/caramel-apples-listeria-outbreak/20636809/.
- ↑ Listeria outbreak: Toll rises to six as Sussex patient dies 1 August 2019 bbc.co.uk accessed 2 August 2019
- ↑ "Two more deaths brings death toll up to five". BBC News. 14 June 2019. https://www.bbc.co.uk/news/uk-england-48636206.
- ↑ "'Smoked salmon' listeria kills two in Australia" (in en-GB). 2019-07-24. https://www.bbc.com/news/world-australia-49094165.
- ↑ "Three deaths, miscarriage tied to meat supplier in listeria cases". 4 October 2019. https://nltimes.nl/2019/10/04/three-deaths-miscarriage-tied-meat-supplier-listeria-cases.
- ↑ "Maple Leaf Foods assessing Listeria-killing chemical". ctv.ca. The Canadian Press (ctvglobemedia). 2008-10-12. https://www.ctvnews.ca/maple-leaf-foods-assessing-listeria-killing-chemical-1.333029.
- ↑ "Food Safety - Listeria". http://www.foodsafety.gov/poisoning/causes/bacteriaviruses/listeria/.
- ↑ 38.0 38.1 38.2 38.3 "CDC - Listeria - Home". cdc.gov/listeria. https://www.cdc.gov/listeria/index.html.
- ↑ 39.0 39.1 39.2 39.3 Temple, M. E.; Nahata, M. C. (May 2000). "Treatment of listeriosis". Annals of Pharmacotherapy 34 (5): 656–61. doi:10.1345/aph.19315. PMID 10852095.
- ↑ "Listeria infection (listeriosis): symptoms and causes". mayoclinic.org. https://www.mayoclinic.org/diseases-conditions/listeria-infection/symptoms-causes/syc-20355269.
- ↑ Janakiraman V (2008). "Listeriosis in pregnancy: diagnosis, treatment, and prevention". Rev Obstet Gynecol 1 (4): 179–85. PMID 19173022.
- ↑ Greenemeier L (21 May 2008). "Recruiting a Dangerous Foe to Fight Cancer and HIV". Scientific American. http://www.sciam.com/article.cfm?id=recruiting-a-dangerous-foe&sc=rss.
Further reading
- Abrishami S. H.; Tall B. D.; Bruursema T. J.; Epstein P. S.; Shah D. B. (1994). "Bacterial adherence and viability on cutting board surfaces". Journal of Food Safety 14 (2): 153–172. doi:10.1111/j.1745-4565.1994.tb00591.x.
- Zhifa Liu; Changhe Yuan; Stephen B. Pruett (2012). "Machine learning analysis of the relationship between changes in immunological parameters and changes in resistance to Listeria monocytogenes: a new approach for risk assessment and systems immunology". Toxicol. Sci. 129 (1): 1:57–73. doi:10.1093/toxsci/kfs201. PMID 22696237.
- Allerberger F (2003). "Listeria: growth, phenotypic differentiation and molecular microbiology". FEMS Immunology and Medical Microbiology 35 (3): 183–189. doi:10.1016/S0928-8244(02)00447-9. PMID 12648835.
- Bayles D. O.; Wilkinson B. J. (2000). "Osmoprotectants and cryoprotectants for Listeria monocytogenes". Letters in Applied Microbiology 30 (1): 23–27. doi:10.1046/j.1472-765x.2000.00646.x. PMID 10728555.
- Bredholt S.; Maukonen J.; Kujanpaa K.; Alanko T.; Olofson U.; Husmark U.; Sjoberg A. M.; Wirtanen G. (1999). "Microbial methods for assessment of cleaning and disinfection of food-processing surfaces cleaned in a low-pressure system". European Food Research and Technology 209 (2): 145–152. doi:10.1007/s002170050474.
- Chae M. S.; Schraft H. (2000). "Comparative evaluation of adhesion and biofilm formation of different Listeria monocytogenes strains". International Journal of Food Microbiology 62 (1–2): 103–111. doi:10.1016/S0168-1605(00)00406-2. PMID 11139010.
- Chen Y. H.; Jackson K. M.; Chea F. P.; Schaffner D. W. (2001). "Quantification and variability analysis of bacterial cross-contamination rates in common food service tasks". Journal of Food Protection 64 (1): 72–80. doi:10.4315/0362-028X-64.1.72. PMID 11198444.
- Davidson C. A.; Griffith C. J.; Peters A. C.; Fieding L. M. (1999). "Evaluation of two methods for monitoring surface cleanliness ñ ATP bioluminescence and traditional hygiene swabbing". Luminescence 14 (1): 33–38. doi:10.1002/(SICI)1522-7243(199901/02)14:1<33::AID-BIO514>3.0.CO;2-I. PMID 10398558.
- Food and Drug Administration (FDA). 2005. "Foodborne Pathogenic Microorganisms and Natural Toxins Handbook: The ìBad Bug Book" Food and Drug Administration, College Park, MD. Accessed: 1 March 2006.
- Foschino R.; Picozzi C.; Civardi A.; Bandini M.; Faroldi P. (2003). "Comparison of surface sampling methods and cleanability assessment of stainless steel surfaces subjected or not to shot peening". Journal of Food Engineering 60 (4): 375–381. doi:10.1016/S0260-8774(03)00060-8.
- Frank, J. F. 2001. "Microbial attachment to food and food contact surfaces". In: Advances in Food and Nutrition Research, Vol. 43. ed. Taylor, S. L. San Diego, CA. Academic Press., Inc. 320–370.
- Gasanov U.; Hughes D.; Hansbro P. M. (2005). "Methods for the isolation and identification of Listeria spp. and Listeria monocytogenes: a review". FEMS Microbiology Reviews 29 (5): 851–875. doi:10.1016/j.femsre.2004.12.002. PMID 16219509.
- Gombas D. E.; Chen Y.; Clavero R. S.; Scott V. N. (2003). "Survey of Listeria monocytogenes in ready-to-eat foods". Journal of Food Protection 66 (4): 559–569. doi:10.4315/0362-028x-66.4.559. PMID 12696677.
- Helke D. M.; Somers E. B.; Wong A. C. L. (1993). "Attachment of Listeria monocytogenes and Salmonella typhimurium to stainless steel and Buna-N-rubber surfaces in the presence of milk and individual milk components". Journal of Food Protection 56 (6): 479–484. doi:10.4315/0362-028X-56.6.479. PMID 31084181.
- Kalmokoff M. L.; Austin J. W.; Wan X. D.; Sanders G.; Banerjee S.; Farber J. M. (2001). "Adsorption, attachment and biofilm formation among isolates of Listeria monocytogenes using model condit ions". Journal of Applied Microbiology 91 (4): 725–34. doi:10.1046/j.1365-2672.2001.01419.x. PMID 11576310.
- Kusumaningrum H. D.; Riboldi G.; Hazeleger W. C.; Beumer R. R. (2003). "Survival of foodborne pathogens on stainless steel surfaces and cross-contamination to foods". International Journal of Food Microbiology 85 (3): 227–236. doi:10.1016/S0168-1605(02)00540-8. PMID 12878381.
- Lin C.; Takeuchi K.; Zhang L.; Dohm C. B.; Meyer J. D.; Hall P. A.; Doyle M. P. (2006). "Cross-contamination between processing equipment and deli meats by Listeria monocytogenes". Journal of Food Protection 69 (1): 559–569. doi:10.4315/0362-028X-69.1.71. PMID 16416903.
- Low J. C.; Donachie W. (1997). "A review of Listeria monocytogenes and listeriosis". The Veterinary Journal 153 (1): 9–29. doi:10.1016/S1090-0233(97)80005-6. PMID 9125353.
- Nikolova, M., Todorova, T. T., Tsankova, G., & Ermenlieva, N. (2016). А possible case of а newborn premature baby with Listeria monocytogenes infection. Scripta Scientifica Medica, 48(2).
- MacNeill S.; Walters D. M.; Dey A.; Glaros A. G.; Cobb C. M. (1998). "Sonic and mechanical toothbrushes". Journal of Clinical Periodontology 25 (12): 988–993. doi:10.1111/j.1600-051X.1998.tb02403.x. PMID 9869348.
- Maxcy R. B. (1975). "Fate of bacteria exposed to washing and drying on stainless steel". Journal of Milk and Food Technology 38 (4): 192–194. doi:10.4315/0022-2747-38.4.192.
- McInnes C.; Engel D.; Martin R. W. (1993). "Fimbriae damage and removal of adherent bacteria after exposure to acoustic energy". Oral Microbiology and Immunology 8 (5): 277–282. doi:10.1111/j.1399-302X.1993.tb00574.x. PMID 7903443.
- McLauchlin J. (1996). "The relationship between Listeria and listeriosis". Food Control 7 (45): 187–193. doi:10.1016/S0956-7135(96)00038-2.
- Montville R.; Chen Y. H.; Schaffner D. W. (2001). "Glove barriers to bacterial cross contamination between hands to food". Journal of Food Protection 64 (6): 845–849. doi:10.4315/0362-028x-64.6.845. PMID 11403136.
- Moore G.; Griffith C.; Fielding L. (2001). "A comparison of traditional and recently developed methods for monitoring surface hygiene within the food industry: a laboratory study". Dairy, Food, and Environmental Sanitation 21: 478–488.
- Moore G.; Griffith C. (2002a). "Factors influencing recovery of microorganisms from surfaces by use of traditional hygiene swabbing". Dairy, Food, and Environmental Sanitation 22: 410–421.
- Parini M. R.; Pitt W. G. (2005). "Removal of oral biofilms by bubbles". Journal of the American Dental Association 136 (12): 1688–1693. doi:10.14219/jada.archive.2005.0112. PMID 16383051.
- Pfaff, N. F., & Tillett, J. (2016). Listeriosis and Toxoplasmosis in Pregnancy: Essentials for Healthcare Providers. The Journal of perinatal & neonatal nursing, 30(2), 131.
- Rocourt J. (1996). "Risk factors for listeriosis". Food Control 7 (4/5): 195–202. doi:10.1016/S0956-7135(96)00035-7.
- Ross, H. (2015). Food Hygiene: Rare Burgers. Eur. Food & Feed L. Rev., 382.
- Salo S.; Laine A.; Alanko T.; Sjoberg A. M.; Wirtanen G. (2000). "Validation of the microbiological methods Hygicult dipsilde, contact plate, and swabbing in surface hygiene control: a Nordic collaborative study". Journal of AOAC International 83 (6): 1357–1365. doi:10.1093/jaoac/83.6.1357. PMID 11128138.
- Schlech W. F. (1996). "Overview of listeriosis". Food Control 7 (4/5): 183–186. doi:10.1016/S0956-7135(96)00040-0.
- Seymour I. J.; Burfoot D.; Smith R. L.; Cox L. A.; Lockwood A. (2002). "Ultrasound decontamination of minimally processed fruits and vegetables". International Journal of Food Science and Technology 37 (5): 547–557. doi:10.1046/j.1365-2621.2002.00613.x.
- Stanford C. M.; Srikantha R.; Wu C. D. (1997). "Efficacy of the Sonicare toothbrush fluid dynamic action on removal of supragingival plaque". Journal of Clinical Dentistry 8 (1): 10–14.
- USDA-FSIS. (United States Department of Agriculture – Food Safety and Inspection Service) 2003. "FSIS Rule Designed To Reduce Listeria monocytogenes In Ready-To-Eat Meat And Poultry Products" . United States Department of Agriculture Food Safety and Inspection Service, Washington, DC. Accessed: 1 March 2006
- Vorst K. L.; Todd E. C. D.; Ryser E. T. (2004). "Improved quantitative recovery of Listeria monocytogenes from stainless steel surfaces using a one-ply composite tissue". Journal of Food Protection 67 (10): 2212–2217. doi:10.4315/0362-028x-67.10.2212. PMID 15508632.
- Whyte W.; Carson W.; Hambraeus A. (1989). "Methods for calculating the efficiency of bacterial surface sampling techniques". Journal of Hospital Infection 13 (1): 33–41. doi:10.1016/0195-6701(89)90093-5. PMID 2564016.
- Wu-Yuan C. D.; Anderson R. D. (1994). "Ability of the SonicareÆ electronic toothbrush to generate dynamic fluid activity that removes bacteria". The Journal of Clinical Dentistry 5 (3): 89–93.
- Zhao P.; Zhao T.; Doyle M. P.; Rubino J. R.; Meng J. (1998). "Development of a model for evaluation of microbial cross-contamination in the kitchen". Journal of Food Protection 61 (8): 960–963. doi:10.4315/0362-028x-61.8.960. PMID 9713754.
- Zottola E. A., Sasahara K. C.; Sasahara (1994). "Microbial biofilms in the food processing industry ñ should they be a concern?". International Journal of Food Microbiology 23 (2): 125–148. doi:10.1016/0168-1605(94)90047-7. PMID 7848776.
External links
- Listeriosis at Curlie
- Listeria genomes and related data at PATRIC, funded by the National Institute of Allergy and Infectious Diseases
- Listeria at BacDive - the Bacterial Diversity Metadatabase
Wikidata ☰ Q746209 entry
 |