Medicine:Budd–Chiari syndrome
| Budd–Chiari syndrome | |
|---|---|
 | |
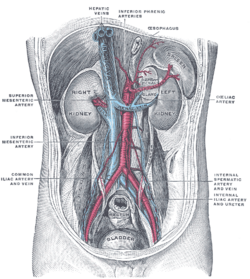
| Budd–Chiari syndrome secondary to cancer; note clot in the inferior vena cava and the metastasis in the liver | |
| Specialty | Hepatology |
| Complications | Liver failure |
| Treatment | Anticoagulant medication, Transjugular intrahepatic portosystemic shunt, Liver transplantation |
Budd–Chiari syndrome is a very rare condition, affecting one in a million adults.[1][2] The condition is caused by occlusion of the hepatic veins (usually due to a blood clot) that drain the liver. The symptoms are non-specific and vary widely, but it may present with the classical triad of abdominal pain, ascites, and liver enlargement. It is usually seen in younger adults, with the median age at diagnosis between the ages of 35 and 40, and it has a similar incidence in males and females.[2] The syndrome can be fulminant, acute, chronic, or asymptomatic. Subacute presentation is the most common form.
Signs and symptoms
The acute syndrome presents with rapidly progressive severe upper abdominal pain, yellow discoloration of the skin and whites of the eyes, liver enlargement, enlargement of the spleen, fluid accumulation within the peritoneal cavity, elevated liver enzymes, and eventually encephalopathy. The fulminant syndrome presents early with encephalopathy and ascites. Liver cell death and severe lactic acidosis may be present as well. Caudate lobe enlargement is often present. The majority of patients have a slower-onset form of Budd–Chiari syndrome. This can be painless. A system of venous collaterals may form around the occlusion which may be seen on imaging as a "spider's web". Patients may progress to cirrhosis and show the signs of liver failure.[3]
Causes
The cause of Budd–Chiari syndrome can be found in more than 80% of patients.[12] However, in 20% of cases, there is no underlying cause discovered. These cases are known as idiopathic Budd–Chiari syndrome.[2] In about 75% of cases, there is an underlying hypercoagulability disorder, with a third of these people having two or more hypercoagulable disorders.[2]
Primary Budd–Chiari syndrome occurs due to thrombosis of the hepatic vein. The most common cause is due to acquired hypercoagulability associated with myeloproliferative disorders (accounting for 40–50% of cases).[13][2] Other acquired hypercoagulable disorders that may result in Budd–Chiari syndrome include antiphospholipid syndrome and paroxysmal nocturnal hemoglobinuria, which are responsible for 10–12% and 7–12% of Budd–Chiari syndrome cases, respectively.[2] Inherited disorders of hypercoagulability may lead to thrombosis of the hepatic vein and Budd–Chiari syndrome. Factor V Leiden is responsible for 8% of cases.[2] Other less common inherited disorders leading to the condition include factor II mutation (3%), protein C deficiency (5%), protein S deficiency (4%), and antithrombin III deficiency(1%).[2][14] Budd–Chiari syndrome may be the presenting sign of these hypercoagulable disorders.
Secondary Budd–Chiari syndrome, which is very rare compared to the primary variant, is due to compression of the hepatic vein by an outside structure (such as a tumor or polycystic kidney disease).[15]
Budd–Chiari syndrome is also seen in tuberculosis, congenital venous webs and occasionally in inferior vena caval stenosis.
An important non-genetic risk factor is the use of estrogen-containing forms of hormonal contraception, which is implicated in 22% of cases of Budd–Chiari syndrome.[2] Other less common risk factors include systemic diseases such as aspergillosis, Behçet's disease, connective tissue disease, mastocytosis, inflammatory bowel disease HIV infection, sarcoidosis or myeloma.[2] Medications such as dacarbazine, pregnancy, trauma or recent abdominal surgery are other causes.[16]
People who have paroxysmal nocturnal hemoglobinuria (PNH) appear to be especially at risk for Budd–Chiari syndrome, more than other forms of thrombophilia: up to 39% develop venous thromboses,[17] and 12% may acquire Budd–Chiari.[18]
Pathophysiology
Any obstruction of the venous vasculature of the liver is referred to as Budd–Chiari syndrome, from the venules to the right atrium. This leads to increased portal vein and hepatic sinusoid pressures as the blood flow stagnates. The increased portal pressure causes increased filtration of vascular fluid with the formation of ascites in the abdomen and collateral venous flow through alternative veins leading to esophageal, gastric and rectal varices. Obstruction also causes centrilobular necrosis and peripheral lobule fatty change due to ischemia. If this condition persists chronically what is known as nutmeg liver will develop. Kidney failure may occur, perhaps due to the body sensing an "underfill" state and subsequent activation of the renin-angiotensin pathways and excess sodium retention.[15]
Diagnosis
Budd Chiari syndrome may present with elevated liver enzymes; alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are often elevated in the acute phase and then decrease over time as chronic liver disease develops.[2] Liver dysfunction can be indirectly measured with labs such as an elevated INR, decreased albumin level, and an elevated bilirubin level.[2]
Budd–Chiari syndrome is most commonly diagnosed using ultrasound studies of the abdomen and retrograde angiography. Ultrasound may show obliteration of hepatic veins, thrombosis or stenosis, spiderweb vessels, large collateral vessels, or a hyperechoic cord replacing a normal vein. Computed tomography (CT) or magnetic resonance imaging (MRI) is sometimes employed although these methods are generally not as sensitive. Liver biopsy is nonspecific but sometimes necessary to differentiate between Budd–Chiari syndrome and other causes of hepatomegaly and ascites, such as galactosemia or Reye's syndrome. Evaluation for a JAK2 V617F mutation is recommended.[citation needed]
Treatment
Identifying and treating the secondary cause of the hypercoagulability, or the primary hypercoagulable disorder leading to the Budd–Chiari syndrome is essential.[2] With regards to secondary causes of hypercoagulability, 40–50% of cases of Budd–Chiari syndrome are due to myeloproliferative disorders, and these conditions each have their own specific treatments.[2] A beta-blocker is indicated for prophylaxis against esophageal variceal bleeding and as needed diuretics can be used in cases of fluid overload in people with ascites.[2] Anti-coagulation is required for all patient's with Budd–Chiari syndrome, even if a cause of hypercoagulability is not found.[2] Warfarin is the preferred, and best studied anticoagulant, but direct factor Xa inhibitors may also be used.[2]
Many patients will require further intervention. Some forms of Budd–Chiari may be treated with surgical shunts (such as portacaval shunt) to divert blood flow around the obstruction or the liver itself. Shunts must be placed early after diagnosis for best results.[19] TIPS (transjugular intrahepatic portosystemic shunt) has replaced shunt surgery as it is less invasive and overcomes intrahepatic outflow obstruction by diverting hepatic and portal blood flow to the inferior vena cava. TIPS accomplishes the same goal as a surgical shunt but has a lower procedure-related mortality, a factor that has led to a growth in its popularity. It is very effective in treating ascites and preventing further variceal bleeding.[20] The TIPS procedure has shown to have good outcomes, with a 78% five-year transplant-free survival rate.[2] If all the hepatic veins are blocked, the portal vein can be approached via the intrahepatic part of inferior vena cava, a procedure called DIPS (direct intrahepatic portocaval shunt).
Segmental occlusions of the inferior vena cava or portal vein can be treated with percutaneous transluminal angioplasty in which a balloon is passed via a guidewire to the site of the venous obstruction and then inflated to open the blockage, this may be followed by stent placement (either immediate stent placement or deferred (when the stent is placed later, if needed)).[21][2] Limited studies on thrombolysis with direct infusion of urokinase and tissue plasminogen activator into the obstructed vein have shown moderate success in treating Budd–Chiari syndrome; however, it is not routinely attempted.[citation needed]
Liver transplantation is an effective treatment for Budd–Chiari. It is generally reserved for patients with fulminant liver failure, failure of shunts, or progression of cirrhosis that reduces the life expectancy to one year.[22] Survival rates in Budd–Chiari syndrome after liver transplantation are 76%, 71% and 68% after 1, 5 and 10 years respectively.[2] It is recommended to continue anticoagulant treatment after liver transplantation, especially if the secondary or primary cause of hypercoagulability is still present, and to monitor for blood clots after liver transplantation.[2]
Pregnancy is not contraindicated in those with Budd Chiari syndrome and if it occurs, anticoagulants should be continued with low molecular weight heparin as the preferred agent, as warfarin is teratogenic (associated with birth defects).[2] Budd Chiari syndrome in pregnancy is associated with an increased risk of miscarriage and prematurity.[2] Screening for esophageal varices is recommended in the second trimester, especially in those not on beta blocker prophylaxis. Screening for portopulmonary hypertension is also recommended for all pregnant patients with Budd Chiari syndrome.[2]
Prognosis
Several studies have attempted to predict the survival of patients with Budd–Chiari syndrome. In general, nearly two-thirds of patients with Budd–Chiari are alive at 10 years. [19] Important negative prognostic indicators include ascites, encephalopathy, elevated Child–Pugh scores, elevated prothrombin time, and altered serum levels of various substances (sodium, creatinine, albumin, and bilirubin). Survival is also highly dependent on the underlying cause of the Budd–Chiari syndrome. For example, a patient with an underlying myeloproliferative disorder may progress to acute leukemia, independently of Budd–Chiari syndrome.[23]
Eponym
It is named after George Budd,[24][25] a British physician, and Hans Chiari,[26] an Austrian pathologist.
References
- ↑ "Budd–Chiari syndrome in Sweden: epidemiology, clinical characteristics and survival - an 18-year experience". Liver International 29 (2): 253–9. Feb 2009. doi:10.1111/j.1478-3231.2008.01838.x. PMID 18694401. http://www3.interscience.wiley.com/journal/121372822/abstract.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 Garcia-Pagán, Juan Carlos; Valla, Dominique-Charles (6 April 2023). "Primary Budd–Chiari Syndrome" (in en). New England Journal of Medicine 388 (14): 1307–1316. doi:10.1056/NEJMra2207738. ISSN 0028-4793. PMID 37018494.
- ↑ "Ascites". https://www.hopkinsmedicine.org/health/conditions-and-diseases/ascites.
- ↑ Etiology, management, and outcome of the Budd–Chiari syndrome..
- ↑ Hepatic vein thrombosis (Budd–Chiari syndrome)..
- ↑ The Budd–Chiari syndrome: a review..
- ↑ Budd–Chiari syndrome: long-term survival and factors affecting mortality..
- ↑ Budd–Chiari Syndrome: clinical patterns and therapy..
- ↑ Budd–Chiari syndrome: etiology, diagnosis and management..
- ↑ Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 51-1987. Progressive abdominal distention in a 51-year-old woman with polycythemia vera..
- ↑ Hepatic outflow obstruction (Budd–Chiari syndrome). Experience with 177 patients and a review of the literature..
- ↑ [4][5][6][7][8][9][10][11]
- ↑ "Prevalence of the activating JAK2 tyrosine kinase mutation V617F in the Budd–Chiari syndrome". Gastroenterology 130 (7): 2031–8. Jun 2006. doi:10.1053/j.gastro.2006.04.008. PMID 16762626.
- ↑ "Prothrombin Mutation G20210A as a Cause of Budd–Chiari Syndrome". Hospital Physician 39 (8): 41–4. Aug 2003. http://www.turner-white.com/pdf/hp_aug03_budd.pdf. Retrieved 2008-10-17.
- ↑ 15.0 15.1 Aydinli, M; Bayraktar, Y (21 May 2007). "Budd-Chiari syndrome: etiology, pathogenesis and diagnosis.". World Journal of Gastroenterology 13 (19): 2693–6. doi:10.3748/wjg.v13.i19.2693. PMID 17569137.
- ↑ "Budd-Chiari Syndrome". https://www.lecturio.com/concepts/budd-chiari-syndrome/.
- ↑ "Natural history of paroxysmal nocturnal hemoglobinuria". N Engl J Med 333 (19): 1253–8. Nov 1995. doi:10.1056/NEJM199511093331904. PMID 7566002.
- ↑ "Paroxysmal nocturnal haemoglobinuria: long-term follow-up and prognostic factors. French Society of Haematology". Lancet 348 (9027): 573–7. Aug 1996. doi:10.1016/S0140-6736(95)12360-1. PMID 8774569.
- ↑ 19.0 19.1 "Determinants of survival and the effect of portosystemic shunting in patients with Budd–Chiari syndrome". Hepatology 39 (2): 500–8. Feb 2004. doi:10.1002/hep.20064. PMID 14768004. https://openaccess.leidenuniv.nl/bitstream/handle/1887/5096/2_303_482.pdf?sequence=1.
- ↑ Tripathi, D. (2014). "Good Clinical outcomes following transjugular intrahepatic portosystemic stent-shunts in budd-chiari syndrome". Alimentary Pharmacology & Therapeutics 39 (8): 864–872. doi:10.1111/apt.12668. PMID 24611957.
- ↑ "Managing Budd–Chiari syndrome: a retrospective review of percutaneous hepatic vein angioplasty and surgical shunting". Gut 44 (4): 568–74. Apr 1999. doi:10.1136/gut.44.4.568. PMID 10075967.
- ↑ "A 27-year experience with surgical treatment of Budd–Chiari syndrome". Ann. Surg. 232 (3): 340–52. Sep 2000. doi:10.1097/00000658-200009000-00006. PMID 10973384.
- ↑ "Ascites". https://www.lecturio.com/concepts/ascites/.
- ↑ Budd–Chiari syndrome at Who Named It?
- ↑ Budd G (1845). On diseases of the liver. London: John Churchill. pp. 135. Brit Lib. 000518193.
- ↑ Chiari H (1898). "Erfahrungen über Infarktbildungen in der Leber des Menschen". Zeitschrift für Heilkunde, Prague 19: 475–512.
External links
| Classification | |
|---|---|
| External resources |
 |