Chemistry:Endothelium-derived relaxing factor
The Endothelium-derived relaxing factor (EDRF) is a strong vasodilator produced by cardiac endothelial cells in response to stress signals such as high levels of ADP accumulation or hypoxia.[1] Robert F. Furchgott is widely recognised for this discovery, even going so far as to be a co-recipient of the 1998 Nobel Prize in Medicine with his colleagues Louis J. Ignarro and Ferid Murad. Nitric oxide (NO) is a key component in any EDRF as these compounds either include NO or are structurally in the form of NO.[2][3]
Physiological Functions and production
EDRF serves various functions, of which the most common and topical are vasodilation and the prevention of platelet adhesion. EDRF also plays a role in the production of cyclic GMP.
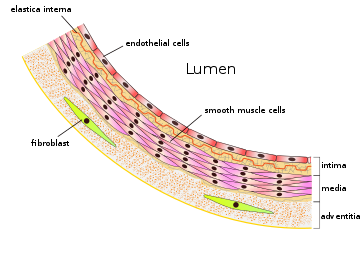
EDRF is produced from L-arginine by an enzyme (endothelial nitric oxide synthase) that is dependent on calcium-calmodulin and NADPH - this occurs in the cardiac endothelium.
EDRF then diffuses to the smooth muscle in vascular tissue (vessels may be large or small), here it enacts endogenous vasodilation. Moreover, it serves the function of preventing sympathetic vasoconstriction - when the sympathetic nervous system, reacting to a situation perceived as dangerous, attempts to raise blood pressure through vasoconstriction.
The NO compound is also capable of reducing clotting in the blood stream due to its ability to prevent platelet adhesion and aggregation.[4]
Related pathology
Atherosclerosis and hypertension are grave contributors in the group of pathological conditions under the umbrella of Cardiovascular disease. Among these conditions is also the disfunction of the endothelium, which given its properties of vasodilation when functional, can cause excessive vasoconstriction, thus leading back to hypertension. Another effect of this particular disfunction may also be excessive platelet adhesion, signifying a significant increase in blood clots, thus the promotion of a prothrombotic state.[4]
References
- ↑ "Endothelium Derived Relaxing Factor - an overview | ScienceDirect Topics". https://www.sciencedirect.com/topics/medicine-and-dentistry/endothelium-derived-relaxing-factor#:~:text=Endothelium-derived%20relaxing%20factor%20(EDRF,as%20hypoxia,%20and%20ADP%20accumulation..
- ↑ Bauer, Viktor; Sotníková, Ružena (29 December 2010). "Nitric oxide--the endothelium-derived relaxing factor and its role in endothelial functions". General Physiology and Biophysics 29 (4): 319–340. doi:10.4149/gpb_2010_04_319. ISSN 0231-5882. PMID 21156995. https://pubmed.ncbi.nlm.nih.gov/21156995/.
- ↑ Francis, S. H.; Busch, J. L.; Corbin, J. D. (2010-09-01). "cGMP-Dependent Protein Kinases and cGMP Phosphodiesterases in Nitric Oxide and cGMP Action" (in en). Pharmacological Reviews 62 (3): 525–563. doi:10.1124/pr.110.002907. ISSN 0031-6997. PMID 20716671.
- ↑ 4.0 4.1 Pirahanchi, Yasaman; Marsidi, Jennifer L.; Brown, Kristen N. (2022), "Physiology, Endothelial Derived Relaxation Factor", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 30725695, http://www.ncbi.nlm.nih.gov/books/NBK537010/, retrieved 2023-01-21
External links
- Pirahanchi, Yasaman; Marsidi, Jennifer L.; Brown, Kristen N. (2022), "Physiology, Endothelial Derived Relaxation Factor", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 30725695, http://www.ncbi.nlm.nih.gov/books/NBK537010/, retrieved 2022-01-29
- Ignarro, L. J.; Buga, G. M.; Wood, K. S.; Byrns, R. E.; Chaudhuri, G. (1987-12-01). "Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide" (in en). Proceedings of the National Academy of Sciences 84 (24): 9265–9269. doi:10.1073/pnas.84.24.9265. ISSN 0027-8424. PMID 2827174. Bibcode: 1987PNAS...84.9265I.
- Vanhoutte, P.-M.; Boulanger, C.-M.; Mombouli, J.-V. (1995-11-24). "Endothelium-derived relaxing factors and converting enzyme inhibition" (in English). American Journal of Cardiology 76 (15): 3E–12E. doi:10.1016/S0002-9149(99)80496-2. ISSN 0002-9149. PMID 7484885. https://www.ajconline.org/article/S0002-9149(99)80496-2/abstract.
 |