Biology:Statin
| Statin | |
|---|---|
| Drug class | |
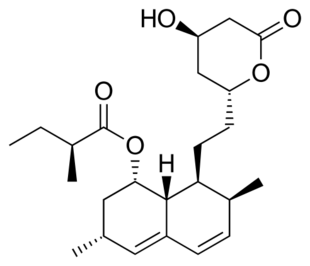 Lovastatin, a compound isolated from Aspergillus terreus, was the first statin to be marketed. | |
| Class identifiers | |
| Synonyms | HMG-CoA reductase inhibitors |
| Use | High cholesterol |
| ATC code | C10AA |
| Biological target | HMG-CoA reductase |
| Clinical data | |
| Drugs.com | Drug Classes |
| External links | |
| MeSH | D019161 |
Statins are a class of medications that reduce illness and mortality in people who are at high risk of cardiovascular disease. They are the most commonly prescribed cholesterol-lowering drugs, and are also known as HMG-CoA reductase inhibitors.[1]
Low-density lipoprotein (LDL) carriers of cholesterol play a key role in the development of atherosclerosis and coronary heart disease via the mechanisms described by the lipid hypothesis. As lipid-lowering medications, statins are effective in lowering LDL cholesterol and so are widely used for primary prevention in people at high risk of cardiovascular disease, as well as in secondary prevention for those who have developed cardiovascular disease.[2][3][4]
Side effects of statins include muscle pain, increased risk of diabetes mellitus, and abnormal blood levels of certain liver enzymes.[5] Additionally, they have rare but severe adverse effects, particularly muscle damage, and very rarely rhabdomyolysis.[6][7]
They act by inhibiting the enzyme HMG-CoA reductase which plays a central role in the production of cholesterol. High cholesterol levels have been associated with cardiovascular disease.[8]
There are various forms of statins, some of which include atorvastatin, fluvastatin, lovastatin, pitavastatin, pravastatin, rosuvastatin, and simvastatin.[9] Combination preparations of a statin and another agent, such as ezetimibe/simvastatin, are also available. The class is on the World Health Organization's List of Essential Medicines with simvastatin being the listed medicine.[10] In 2005, sales were estimated at US$18.7 billion in the United States.[11] The best-selling statin is atorvastatin, also known as Lipitor, which in 2003 became the best-selling pharmaceutical in history.[12] The manufacturer Pfizer reported sales of US$12.4 billion in 2008.[13]
Patient compliance with statin usage has been problematic for many medical practitioners, despite robust evidence of the benefits to the majority of patients.[14]
Medical uses
Statins are usually used to lower blood cholesterol levels and reduce risk for illnesses related to atherosclerosis, with a varying degree of effect depending on underlying risk factors and history of cardiovascular disease.[15] Clinical practice guidelines generally recommend people start with lifestyle modification through a cholesterol-lowering diet and physical exercise. For those unable to meet their lipid-lowering goals through such methods, statins can be helpful.[16][17] The medication appears to work equally well regardless of sex,[18] although some sex-related differences in treatment response were described.[19]
If there is an underlying history of cardiovascular disease, it has a significant impact on the effects of statin. This can be used to divide medication usage into broad categories of primary and secondary prevention.[20]
Primary prevention
For the primary prevention of cardiovascular disease, the United States Preventive Services Task Force (USPSTF) 2016 guidelines recommend statins for those who have at least one risk factor for coronary heart disease, are between 40 and 75 years old, and have at least a 10% 10-year risk of heart disease, as calculated by the 2013 ACC/AHA Pooled Cohort algorithm.[20][21][22] Risk factors for coronary heart disease included abnormal lipid levels in the blood, diabetes mellitus, high blood pressure, and smoking.[21] They recommended selective use of low-to-moderate doses statins in the same adults who have a calculated 10-year cardiovascular disease event risk of 7.5–10% or greater.[21] In people over the age of 70, statins decrease the risk of cardiovascular disease but only in those with a history of heavy cholesterol blockage in their arteries.[23]
Most evidence suggests that statins are also effective in preventing heart disease in those with high cholesterol but no history of heart disease. A 2013 Cochrane review found a decrease in risk of death and other poor outcomes without any evidence of harm.[4] For every 138 people treated for 5 years, one fewer dies; for every 49 treated, one fewer has an episode of heart disease.[11] A 2011 review reached similar conclusions,[24] and a 2012 review found benefits in both women and men.[25] A 2010 review concluded that treatment without history of cardiovascular disease reduces cardiovascular events in men but not women, and provides no mortality benefit in either sex.[26] Two other meta-analyses published that year, one of which used data obtained exclusively from women, found no mortality benefit in primary prevention.[27][28]
The National Institute for Health and Clinical Excellence (NICE) recommends statin treatment for adults with an estimated 10 year risk of developing cardiovascular disease that is greater than 10%.[29] Guidelines by the American College of Cardiology and the American Heart Association recommend statin treatment for primary prevention of cardiovascular disease in adults with LDL cholesterol ≥ 190 mg/dL or those with diabetes, age 40–75 with LDL-C 70–190 mg/dL; or in those with a 10-year risk of developing heart attack or stroke of 7.5% or more. In this latter group, statin assignment was not automatic, but was recommended to occur only after a clinician-patient risk discussion with shared decision making where other risk factors and lifestyle are addressed, the potential for benefit from a statin is weighed against the potential for adverse effects or drug interactions and informed patient preference is elicited. Moreover, if a risk decision was uncertain, factors such as family history, coronary calcium score, ankle-brachial index, and an inflammation test (hs-CRP ≥ 2.0 mg/L) were suggested to inform the risk decision. Additional factors that could be used were an LDL-C ≥ 160 or a very high lifetime risk.[30] However, critics such as Steven E. Nissen say that the AHA/ACC guidelines were not properly validated, overestimate the risk by at least 50%, and recommend statins for people who will not benefit, based on populations whose observed risk is lower than predicted by the guidelines.[31] The European Society of Cardiology and the European Atherosclerosis Society recommend the use of statins for primary prevention, depending on baseline estimated cardiovascular score and LDL thresholds.[32]
Secondary prevention
Statins are effective in decreasing mortality in people with pre-existing cardiovascular disease.[33] Pre-existing disease can have many manifestations. Defining illnesses include a prior heart attack, stroke, stable or unstable angina, aortic aneurysm, or other arterial ischemic disease, in the presence of atherosclerosis.[20] They are also advocated for use in people at high risk of developing coronary heart disease.[34] On average, statins can lower LDL cholesterol by 1.8 mmol/L (70 mg/dL), which translates into an estimated 60% decrease in the number of cardiac events (heart attack, sudden cardiac death) and a 17% reduced risk of stroke after long-term treatment.[35] A greater benefit is observed with high-intensity statin therapy.[36] They have less effect than the fibrates or niacin in reducing triglycerides and raising HDL-cholesterol ("good cholesterol").[37][38]
No studies have examined the effect of statins on cognition in patients with prior stroke. However, two large studies (HPS and PROSPER) that included people with vascular diseases reported that simvastatin and pravastatin did not impact cognition.[39]
Statins have been studied for improving operative outcomes in cardiac and vascular surgery.[40] Mortality and adverse cardiovascular events were reduced in statin groups.[41]
Older adults who receive statin therapy at time of discharge from the hospital after an inpatient stay have been studied. People with cardiac ischemia not previously on statins at the time of admission have a lower risk of major cardiac adverse events and hospital readmission two years post-hospitalization.[42][43]
Statin product offerings - comparative effectiveness
All statins appear effective regardless of potency or degree of cholesterol reduction.[24][44][45] Simvastatin and pravastatin appear to have a reduced incidence of side-effects.[5][46][47]
Women
According to the 2015 Cochrane systematic review, atorvastatin showed greater cholesterol-lowering effect in women than in men compared to rosuvastatin.[48]
Children
In children statins are effective at reducing cholesterol levels in those with familial hypercholesterolemia.[49] Their long term safety is, however, unclear.[49][50] Some recommend that if lifestyle changes are not enough statins should be started at 8 years old.[51]
Familial hypercholesterolemia
Statins may be less effective in reducing LDL cholesterol in people with familial hypercholesterolemia, especially those with homozygous deficiencies.[52] These people have defects usually in either the LDL receptor or apolipoprotein B genes, both of which are responsible for LDL clearance from the blood.[53] Statins remain a first-line treatment in familial hypercholesterolemia,[52] although other cholesterol-reducing measures may be required.[54] In people with homozygous deficiencies, statins may still prove helpful, albeit at high doses and in combination with other cholesterol-reducing medications.[55]
Contrast-induced nephropathy
A 2014 meta-analysis found that statins could reduce the risk of contrast-induced nephropathy by 53% in people undergoing coronary angiography/percutaneous interventions. The effect was found to be stronger among those with preexisting kidney dysfunction or diabetes mellitus.[56]
Chronic kidney disease
The risk of cardiovascular disease is similar in people with chronic kidney disease and coronary artery disease and statins are often suggested.[15] There is some evidence that appropriate use of statin medications in people with chronic kidney disease who do not require dialysis may reduce mortality and the incidence of major cardiac events by up to 20% and are not that likely to increase the risk of stroke or kidney failure.[15]
Asthma
Statins have been identified as having a possible adjunct role in the treatment of asthma though anti-inflammatory pathways.[57] There is low quality evidence for the use of statins in treating asthma, however further research is required to determine the effectiveness and safety of this therapy in those with asthma.[57]
Adverse effects
| Choosing a statin for people with special considerations[58] | |||
|---|---|---|---|
| Condition | Commonly recommended statins | Explanation | |
| Kidney transplantation recipients taking ciclosporin | Pravastatin or fluvastatin | Drug interactions are possible, but studies have not shown that these statins increase exposure to ciclosporin.[59] | |
| HIV-positive people taking protease inhibitors | Atorvastatin, pravastatin or fluvastatin | Negative interactions are more likely with other choices.[60] | |
| Persons taking gemfibrozil, a non-statin lipid-lowering drug | Atorvastatin | Combining gemfibrozil and a statin increases risk of rhabdomyolysis and subsequently kidney failure[61][62] | |
| Persons taking the anticoagulant warfarin | Any statin | The statin use may require that the warfarin dose be changed, as some statins increase the effect of warfarin.[63] | |
The most important adverse side effects are muscle problems, an increased risk of diabetes mellitus, and increased liver enzymes in the blood due to liver damage.[5][64] Over 5 years of treatment statins result in 75 cases of diabetes, 7.5 cases of bleeding stroke, and 5 cases of muscle damage per 10,000 people treated.[33] This could be due to the statins inhibiting the enzyme (HMG-CoA reductase), which is necessary to make cholesterol, but also for other processes, such as CoQ10 production, which is important for muscle function and sugar regulation.[65]
Other possible adverse effects include neuropathy,[66] pancreatic and liver dysfunction, and sexual dysfunction.[67] The rate at which such events occur has been widely debated, in part because the risk/benefit ratio of statins in low-risk populations is highly dependent on the rate of adverse events.[68][69][70] A Cochrane meta-analysis of statin clinical trials in primary prevention found no evidence of excess adverse events among those treated with statins compared to placebo.[4] Another meta-analysis found a 39% increase in adverse events in statin treated people relative to those receiving placebo, but no increase in serious adverse events.[71] The author of one study argued that adverse events are more common in clinical practice than in randomized clinical trials.[67] A systematic review concluded that while clinical trial meta-analyses underestimate the rate of muscle pain associated with statin use, the rates of rhabdomyolysis are still "reassuringly low" and similar to those seen in clinical trials (about 1–2 per 10,000 person years).[72] Another systematic review from the International Centre for Circulatory Health of the National Heart and Lung Institute in London concluded that only a small fraction of side effects reported by people on statins are actually attributable to the statin.[73]
Cognitive effects
Multiple systematic reviews and meta-analyses have concluded that the available evidence does not support an association between statin use and cognitive decline.[74][75][76][77][78] A 2010 meta-review of medical trials involving over 65,000 people concluded that Statins decreased the risk of dementia, Alzheimer's disease, and even improved cognitive impairment in some cases.[79][needs update] Additionally, both the Patient-Centered Research into Outcomes Stroke Patients Prefer and Effectiveness Research (PROSPER) study[80] and the Health Protection Study (HPS) demonstrated that simvastatin and pravastatin did not affect cognition for patients with risk factors for, or a history of, vascular diseases.[81]
There are reports of reversible cognitive impairment with statins.[82] The U.S. Food and Drug Administration (FDA) package insert on statins includes a warning about the potential for non-serious and reversible cognitive side effects with the medication (memory loss, confusion).[83]
Muscles
In observational studies 10–15% of people who take statins experience muscle problems; in most cases these consist of muscle pain.[6] These rates, which are much higher than those seen in randomized clinical trials[72] have been the topic of extensive debate and discussion.[33][84]
Muscle and other symptoms often cause patients to stop taking a statin.[85] This is known as statin intolerance. A 2021 double-blind multiple crossover randomized controlled trial (RCT) in statin-intolerant patients found that adverse effects, including muscle pain, were similar between atorvastatin and placebo.[86] A smaller double-blind RCT obtained similar results.[87] The results of these studies help explain why statin symptom rates in observational studies are so much higher than in double-blind RCTs and support the notion that the difference results from the nocebo effect; that the symptoms are caused by expectations of harm.[88]
Media reporting on statins is often negative, and patient leaflets inform patients that rare but potentially serious muscle problems can occur during statin treatment. These create expectations of harm. Nocebo symptoms are real and bothersome and are a major barrier to treatment. Because of this, many people stop taking statins,[89] which have been proven in numerous large-scale RCTs to reduce heart attacks, stroke, and deaths[90] – as long as people continue to take them.
Serious muscle problems such as rhabdomyolysis (destruction of muscle cells) and statin-associated autoimmune myopathy occur in less than 0.1% of treated people.[91] Rhabdomyolysis can in turn result in life-threatening kidney injury. The risk of statin-induced rhabdomyolysis increases with older age, use of interacting medications such as fibrates, and hypothyroidism.[92][93] Coenzyme Q10 (ubiquinone) levels are decreased in statin use;[94] CoQ10 supplements are sometimes used to treat statin-associated myopathy, though evidence of their efficacy is lacking as of 2017[update].[95] The gene SLCO1B1 (Solute carrier organic anion transporter family member 1B1) codes for an organic anion-transporting polypeptide that is involved in the regulation of the absorption of statins. A common variation in this gene was found in 2008 to significantly increase the risk of myopathy.[96]
Records exist of over 250,000 people treated from 1998 to 2001 with the statin drugs atorvastatin, cerivastatin, fluvastatin, lovastatin, pravastatin, and simvastatin.[97] The incidence of rhabdomyolysis was 0.44 per 10,000 patients treated with statins other than cerivastatin. However, the risk was over 10-fold greater if cerivastatin was used, or if the standard statins (atorvastatin, fluvastatin, lovastatin, pravastatin, or simvastatin) were combined with a fibrate (fenofibrate or gemfibrozil) treatment. Cerivastatin was withdrawn by its manufacturer in 2001.[98]
Some researchers have suggested hydrophilic statins, such as fluvastatin, rosuvastatin, and pravastatin, are less toxic than lipophilic statins, such as atorvastatin, lovastatin, and simvastatin, but other studies have not found a connection.[99] Lovastatin induces the expression of gene atrogin-1, which is believed to be responsible in promoting muscle fiber damage.[99] Tendon rupture does not appear to occur.[100]
Diabetes
The relationship between statin use and risk of developing diabetes remains unclear and the results of reviews are mixed.[101][102][103][104] Higher doses have a greater effect, but the decrease in cardiovascular disease outweighs the risk of developing diabetes.[105] Use in postmenopausal women is associated with an increased risk for diabetes.[106] The exact mechanism responsible for the possible increased risk of diabetes mellitus associated with statin use is unclear.[103] However, recent findings have indicated the inhibition of HMGCoAR as a key mechanism.[107] Statins are thought to decrease cells' uptake of glucose from the bloodstream in response to the hormone insulin.[103] One way this is thought to occur is by interfering with cholesterol synthesis which is necessary for the production of certain proteins responsible for glucose uptake into cells such as GLUT1.[103]
Cancer
Several meta-analyses have found no increased risk of cancer, and some meta-analyses have found a reduced risk.[108][109][110][111][112] Specifically, statins may reduce the risk of esophageal cancer,[113] colorectal cancer,[114] gastric cancer,[115][116] hepatocellular carcinoma,[117] and possibly prostate cancer.[118][119] They appear to have no effect on the risk of lung cancer,[120] kidney cancer,[121] breast cancer,[122] pancreatic cancer,[123] or bladder cancer.[124]
Drug interactions
Combining any statin with a fibrate or niacin (other categories of lipid-lowering drugs) increases the risks for rhabdomyolysis to almost 6.0 per 10,000 person-years.[97] Monitoring liver enzymes and creatine kinase is especially prudent in those on high-dose statins or in those on statin/fibrate combinations, and mandatory in the case of muscle cramps or of deterioration in kidney function.[citation needed]
Consumption of grapefruit or grapefruit juice inhibits the metabolism of certain statins, and bitter oranges may have a similar effect.[125] Furanocoumarins in grapefruit juice (i.e. bergamottin and dihydroxybergamottin) inhibit the cytochrome P450 enzyme CYP3A4, which is involved in the metabolism of most statins (however, it is a major inhibitor of only lovastatin, simvastatin, and to a lesser degree, atorvastatin) and some other medications[126] (flavonoids (i.e. naringin) were thought to be responsible). This increases the levels of the statin, increasing the risk of dose-related adverse effects (including myopathy/rhabdomyolysis). The absolute prohibition of grapefruit juice consumption for users of some statins is controversial.[127]
The U.S. Food and Drug Administration (FDA) notified healthcare professionals of updates to the prescribing information concerning interactions between protease inhibitors and certain statin drugs. Protease inhibitors and statins taken together may increase the blood levels of statins and increase the risk for muscle injury (myopathy). The most serious form of myopathy, rhabdomyolysis, can damage the kidneys and lead to kidney failure, which can be fatal.[128]
Osteoporosis and fractures
Studies have found that the use of statins may protect against getting osteoporosis and fractures or may induce osteoporosis and fractures.[129][130][131][132] A cross-sectional retrospective analysis of the entire Austrian population found that the risk of getting osteoporosis is dependent on the dose used.[133]
Neuropathy
Statin consumption has been connected with increased prevalence of neuropathy.[134][135]
Mechanism of action
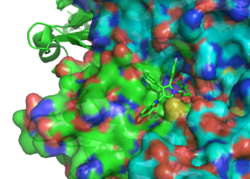

Statins act by competitively inhibiting HMG-CoA reductase, the rate-limiting enzyme of the mevalonate pathway. Because statins are similar in structure to HMG-CoA on a molecular level, they will fit into the enzyme's active site and compete with the native substrate (HMG-CoA). This competition reduces the rate by which HMG-CoA reductase is able to produce mevalonate, the next molecule in the cascade that eventually produces cholesterol. A variety of natural statins are produced by Penicillium and Aspergillus fungi as secondary metabolites. These natural statins probably function to inhibit HMG-CoA reductase enzymes in bacteria and fungi that compete with the producer.[137]
Inhibiting cholesterol synthesis
By inhibiting HMG-CoA reductase, statins block the pathway for synthesizing cholesterol in the liver. This is significant because most circulating cholesterol comes from internal manufacture rather than the diet. When the liver can no longer produce cholesterol, levels of cholesterol in the blood will fall. Cholesterol synthesis appears to occur mostly at night,[138] so statins with short half-lives are usually taken at night to maximize their effect. Studies have shown greater LDL and total cholesterol reductions in the short-acting simvastatin taken at night rather than the morning,[139][140] but have shown no difference in the long-acting atorvastatin.[141]
Increasing LDL uptake
In rabbits, liver cells sense the reduced levels of liver cholesterol and seek to compensate by synthesizing LDL receptors to draw cholesterol out of the circulation.[142] This is accomplished via proteases that cleave membrane-bound sterol regulatory element binding proteins, which then migrate to the nucleus and bind to the sterol response elements. The sterol response elements then facilitate increased transcription of various other proteins, most notably, LDL receptor. The LDL receptor is transported to the liver cell membrane and binds to passing LDL and VLDL particles, mediating their uptake into the liver, where the cholesterol is reprocessed into bile salts and other byproducts. This results in a net effect of less LDL circulating in blood.
Decreasing of specific protein prenylation
Statins, by inhibiting the HMG CoA reductase pathway, inhibit downstream synthesis of isoprenoids, such as farnesyl pyrophosphate and geranylgeranyl pyrophosphate. Inhibition of protein prenylation for proteins such as RhoA (and subsequent inhibition of Rho-associated protein kinase) may be involved, at least partially, in the improvement of endothelial function, modulation of immune function, and other pleiotropic cardiovascular benefits of statins,[143][144][145][146][147][148] as well as in the fact that a number of other drugs that lower LDL have not shown the same cardiovascular risk benefits in studies as statins,[149] and may also account for some of the benefits seen in cancer reduction with statins.[150] In addition, the inhibitory effect on protein prenylation may also be involved in a number of unwanted side effects associated with statins, including muscle pain (myopathy)[151] and elevated blood sugar (diabetes).[152]
Other effects
As noted above, statins exhibit action beyond lipid-lowering activity in the prevention of atherosclerosis through so-called "pleiotropic effects of statins."[146] The pleiotropic effects of statins remain controversial.[153] The ASTEROID trial showed direct ultrasound evidence of atheroma regression during statin therapy.[154] Researchers hypothesize that statins prevent cardiovascular disease via four proposed mechanisms (all subjects of a large body of biomedical research):[153]
- Improve endothelial function
- Modulate inflammatory responses
- Maintain plaque stability
- Prevent blood clot formation
In 2008, the JUPITER trial showed statins provided benefit in those who had no history of high cholesterol or heart disease, but only in those with elevated high-sensitivity C-reactive protein (hsCRP) levels, an indicator for inflammation.[155] The study has been criticized due to perceived flaws in the study design,[156][157][158] although Paul M. Ridker, lead investigator of the JUPITER trial, has responded to these criticisms at length.[159]
As the target of statins, the HMG-CoA reductase, is highly similar between eukaryota and archaea, statins also act as antibiotics against archaea by inhibiting archaeal mevalonate biosynthesis. This has been shown in vivo and in vitro.[160] Since patients with a constipation phenotype present with higher abundance of methanogenic archaea in the gut, the use of statins for management of irritable bowel syndrome has been proposed and may actually be one of the hidden benefits of statin use.[161][162]
Available forms
The statins are divided into two groups: fermentation-derived and synthetic. Some specific types are listed in the table below. Note that the associated brand names may vary between countries.
| Statin | Image | Brand name | Derivation | Metabolism[61] | Half-life |
|---|---|---|---|---|---|
| Atorvastatin | 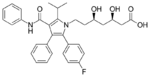 |
Arkas, Ator, Atoris, Lipitor, Torvast, Totalip | Synthetic | CYP3A4 | 14–19 hours.[163] |
| Cerivastatin | 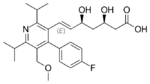 |
Baycol, Lipobay (withdrawn from the market in August 2001 due to risk of serious rhabdomyolysis) | Synthetic | various CYP3A isoforms[164] | |
| Fluvastatin | 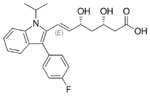 |
Lescol, Lescol XL, Lipaxan, Primesin | Synthetic | CYP2C9 | 1–3 hours.[163] |
| Lovastatin | 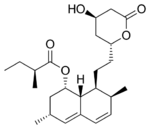 |
Altocor, Altoprev, Mevacor | Naturally occurring, fermentation-derived compound. It is found in oyster mushrooms and red yeast rice | CYP3A4 | 1–3 hours.[163] |
| Mevastatin | 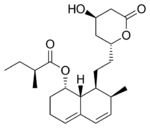 |
Compactin | Naturally occurring compound found in red yeast rice | CYP3A4 | |
| Pitavastatin | 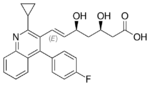 |
Alipza, Livalo, Livazo, Pitava, Zypitamag | Synthetic | CYP2C9 and CYP2C8 (minimally) | |
| Pravastatin | 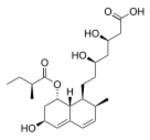 |
Aplactin, Lipostat, Prasterol, Pravachol, Pravaselect, Sanaprav, Selectin, Selektine, Vasticor | Fermentation-derived (a fermentation product of bacterium Nocardia autotrophica) | Non-CYP[165] | 1–3 hours.[163] |
| Rosuvastatin | 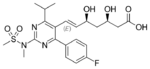 |
Colcardiol, Colfri, Crativ, Crestor, Dilivas, Exorta, Koleros, Lipidover, Miastina, Provisacor, Rosastin, Simestat, Staros | Synthetic | CYP2C9 and CYP2C19 | 14–19 hours.[163] |
| Simvastatin | 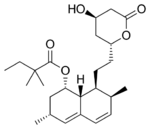 |
Alpheus, Krustat, Lipenil, Lipex, Liponorm, Medipo, Omistat, Rosim, Setorilin, Simbatrix, Sincol, Sinvacor, Sinvalip, Sivastin, Sinvat, Vastgen, Vastin, Xipocol, Zocor | Fermentation-derived (simvastatin is a synthetic derivate of a fermentation product of Aspergillus terreus) | CYP3A4 | 1–3 hours.[163] |
| Atorvastatin + amlodipine | Caduet, Envacar | Combination therapy: statin + calcium antagonist | |||
| Atorvastatin + perindopril + amlodipine | Lipertance, Triveram[166][167][168] | Combination therapy: statin + ACE inhibitor + calcium antagonist | |||
| Lovastatin + niacin extended-release | Advicor, Mevacor | Combination therapy | |||
| Rosuvastatin + ezetimibe | Cholecomb, Delipid Plus, Росулип плюс, Rosulip, Rosumibe, Viazet[169][170][171][172] | Combination therapy: statin + cholesterol absorption inhibitor | |||
| Simvastatin + ezetimibe | Goltor, Inegy, Staticol, Vytorin, Zestan, Zevistat | Combination therapy: statin + cholesterol absorption inhibitor | |||
| Simvastatin + niacin extended-release | Simcor, Simcora | Combination therapy |
LDL-lowering potency varies between agents. Cerivastatin is the most potent, (withdrawn from the market in August 2001 due to risk of serious rhabdomyolysis) followed by (in order of decreasing potency), rosuvastatin, atorvastatin, simvastatin, lovastatin, pravastatin, and fluvastatin.[173] The relative potency of pitavastatin has not yet been fully established, but preliminary studies indicate a potency similar to rosuvastatin.[174]

Some types of statins are naturally occurring, and can be found in such foods as oyster mushrooms and red yeast rice. Randomized controlled trials have found these foodstuffs to reduce circulating cholesterol, but the quality of the trials has been judged to be low.[175] Due to patent expiration, most of the block-buster branded statins have been generic since 2012, including atorvastatin, the largest-selling[citation needed] branded drug.[176][177][178][179][180][181][182]
| Statin equivalent dosages | ||||||
|---|---|---|---|---|---|---|
| % LDL reduction (approx.) | Atorvastatin | Fluvastatin | Lovastatin | Pravastatin | Rosuvastatin | Simvastatin |
| 10–20% | – | 20 mg | 10 mg | 10 mg | – | 5 mg |
| 20–30% | – | 40 mg | 20 mg | 20 mg | – | 10 mg |
| 30–40% | 10 mg | 80 mg | 40 mg | 40 mg | 5 mg | 20 mg |
| 40–45% | 20 mg | – | 80 mg | 80 mg | 5–10 mg | 40 mg |
| 46–50% | 40 mg | – | – | – | 10–20 mg | 80 mg* |
| 50–55% | 80 mg | – | – | – | 20 mg | – |
| 56–60% | – | – | – | – | 40 mg | – |
| * 80 mg dose no longer recommended due to increased risk of rhabdomyolysis | ||||||
| Starting dose | ||||||
| Starting dose | 10–20 mg | 20 mg | 10–20 mg | 40 mg | 10 mg; 5 mg if hypothyroid, >65 yo, Asian | 20 mg |
| If higher LDL reduction goal | 40 mg if >45% | 40 mg if >25% | 20 mg if >20% | – | 20 mg if LDL >190 mg/dL (4.87 mmol/L) | 40 mg if >45% |
| Optimal timing | Anytime | Evening | With evening meals | Anytime | Anytime | Evening |
History
The role of cholesterol in the development of cardiovascular disease was elucidated in the second half of the 20th century.[183] This lipid hypothesis prompted attempts to reduce cardiovascular disease burden by lowering cholesterol. Treatment consisted mainly of dietary measures, such as a low-fat diet, and poorly tolerated medicines, such as clofibrate, cholestyramine, and nicotinic acid. Cholesterol researcher Daniel Steinberg writes that while the Coronary Primary Prevention Trial of 1984 demonstrated cholesterol lowering could significantly reduce the risk of heart attacks and angina, physicians, including cardiologists, remained largely unconvinced.[184] Scientists in academic settings and the pharmaceutical industry began trying to develop a drug to reduce cholesterol more effectively. There were several potential targets, with 30 steps in the synthesis of cholesterol from acetyl-coenzyme A.[185]
In 1971, Akira Endo, a Japanese biochemist working for the pharmaceutical company Sankyo, began to investigate this problem. Research had already shown cholesterol is mostly manufactured by the body in the liver with the enzyme HMG-CoA reductase.[12] Endo and his team reasoned that certain microorganisms may produce inhibitors of the enzyme to defend themselves against other organisms, as mevalonate is a precursor of many substances required by organisms for the maintenance of their cell walls or cytoskeleton (isoprenoids).[137] The first agent they identified was mevastatin (ML-236B), a molecule produced by the fungus Penicillium citrinum.
A British group isolated the same compound from Penicillium brevicompactum, named it compactin, and published their report in 1976.[186] The British group mentions antifungal properties, with no mention of HMG-CoA reductase inhibition. Mevastatin was never marketed, because of its adverse effects of tumors, muscle deterioration, and sometimes death in laboratory dogs. P. Roy Vagelos, chief scientist and later CEO of Merck & Co, was interested, and made several trips to Japan starting in 1975. By 1978, Merck had isolated lovastatin (mevinolin, MK803) from the fungus Aspergillus terreus, first marketed in 1987 as Mevacor.[12]
In the 1990s, as a result of public campaigns, people in the United States became familiar with their cholesterol numbers and the difference between HDL and LDL cholesterol, and various pharmaceutical companies began producing their own statins, such as pravastatin (Pravachol), manufactured by Sankyo and Bristol-Myers Squibb. In April 1994, the results of a Merck-sponsored study, the Scandinavian Simvastatin Survival Study, were announced. Researchers tested simvastatin, later sold by Merck as Zocor, on 4,444 patients with high cholesterol and heart disease. After five years, the study concluded the patients saw a 35% reduction in their cholesterol, and their chances of dying of a heart attack were reduced by 42%.[12][187] In 1995, Zocor and Mevacor both made Merck over US$1 billion.[12]
Though he did not profit from his original discovery, Endo was awarded the 2006 Japan Prize, and the Lasker-DeBakey Clinical Medical Research Award in 2008, for his pioneering research.[188] Endo was also inducted into the National Inventors Hall of Fame in Alexandria, Virginia in 2012. Michael S. Brown and Joseph Goldstein, who won the Nobel Prize for related work on cholesterol, said of Endo: "The millions of people whose lives will be extended through statin therapy owe it all to Akira Endo."[189]
As of 2016[update] misleading claims exaggerating the adverse effects of statins had received widespread media coverage, with a consequent negative impact to public health.[33] Controversy over the effectiveness of statins in the medical literature was amplified in popular media in the early 2010s, leading an estimated 200,000 people in the UK to stop using statins over a six-month period to mid 2016, according to the authors of a study funded by the British Heart Foundation. They estimated that there could be up to 2,000 extra heart attacks or strokes over the following 10 years as a consequence.[190] An unintended effect of the academic statin controversy has been the spread of scientifically questionable alternative therapies. Cardiologist Steven Nissen at Cleveland Clinic commented "We are losing the battle for the hearts and minds of our patients to Web sites..."[191] promoting unproven medical therapies. Harriet Hall sees a spectrum of "statin denialism" ranging from pseudoscientific claims to the understatement of benefits and overstatement of side effects, all of which is contrary to the scientific evidence.[192]
Several statins have been approved as generic drugs in the United States:
- Lovastatin (Mevacor) in December 2001[193][194][195]
- Pravastatin (Pravachol) in April 2006[196][197][198]
- Simvastatin (Zocor) in June 2006[199][200][201]
- Atorvastatin (Lipitor) in November 2011[202][203][204][205]
- Fluvastatin (Lescol) in April 2012[206][207]
- Pitavastatin (Livalo) and rosuvastatin (Crestor) in 2016[208][209]
- Ezetimibe/simvastatin (Vytorin) and ezetimibe/atorvastatin (Liptruzet) in 2017[210]
Research
Clinical studies have been conducted on the use of statins in dementia,[211] lung cancer,[212] nuclear cataracts,[213] hypertension,[214][215] and prostate cancer[216] and breast cancer.[217] There is no high quality evidence that statins are useful for pneumonia.[218] The small number of available trials do not support the use of statins as an adjunctive therapy or as a monotherapy in multiple sclerosis.[219]
References
- ↑ "Cholesterol Drugs". https://watchlearnlive.heart.org/?moduleSelect=chldrg.
- ↑ "Management of Blood Cholesterol". JAMA 321 (8): 800–801. February 2019. doi:10.1001/jama.2019.0015. PMID 30715135.
- ↑ Lipid Modification: Cardiovascular Risk Assessment and the Modification of Blood Lipids for the Primary and Secondary Prevention of Cardiovascular Disease. National Institute for Health and Clinical Excellence: Guidance. London: National Institute for Health and Care Excellence (UK). July 2014. NICE Clinical Guidelines, No. 181. https://www.ncbi.nlm.nih.gov/books/NBK248067/.
- ↑ 4.0 4.1 4.2 "Statins for the primary prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews 2013 (1): CD004816. January 2013. doi:10.1002/14651858.CD004816.pub5. PMID 23440795.
- ↑ 5.0 5.1 5.2 "Comparative tolerability and harms of individual statins: a study-level network meta-analysis of 246 955 participants from 135 randomized, controlled trials". Circulation. Cardiovascular Quality and Outcomes 6 (4): 390–399. July 2013. doi:10.1161/CIRCOUTCOMES.111.000071. PMID 23838105.
- ↑ 6.0 6.1 "Statin-induced myopathy: a review and update". Expert Opinion on Drug Safety 10 (3): 373–387. May 2011. doi:10.1517/14740338.2011.540568. PMID 21342078.
- ↑ "Should you be worried about severe muscle pain from statins?" (in en). https://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/expert-answers/rhabdomyolysis/faq-20057817.
- ↑ "Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths". Lancet 370 (9602): 1829–1839. December 2007. doi:10.1016/S0140-6736(07)61778-4. PMID 18061058.
- ↑ "Cardiovascular drugs". Martindale: the complete drug reference (36th ed.). London: Pharmaceutical Press. 2009. pp. 1155–1434. ISBN 978-0-85369-840-1.
- ↑ World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. 2019. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ 11.0 11.1 "Statin therapy for primary prevention of cardiovascular disease". JAMA 310 (22): 2451–2452. December 2013. doi:10.1001/jama.2013.281348. PMID 24276813.
- ↑ 12.0 12.1 12.2 12.3 12.4 "The $10 billion pill". Fortune 147 (1): 58–62, 66, 68. January 2003. PMID 12602122. http://archive.fortune.com/magazines/fortune/fortune_archive/2003/01/20/335643/index.htm.
- ↑ "Doing Things Differently" , Pfizer 2008 Annual Review, 23 April 2009, p. 15.
- ↑ "How do we improve patient compliance and adherence to long-term statin therapy?". Current Atherosclerosis Reports 15 (1): 291. January 2013. doi:10.1007/s11883-012-0291-7. PMID 23225173.
- ↑ 15.0 15.1 15.2 Tunnicliffe, David J.; Palmer, Suetonia C.; Cashmore, Brydee A.; Saglimbene, Valeria M.; Krishnasamy, Rathika; Lambert, Kelly; Johnson, David W.; Craig, Jonathan C. et al. (2023-11-29). "HMG CoA reductase inhibitors (statins) for people with chronic kidney disease not requiring dialysis". The Cochrane Database of Systematic Reviews 11 (11): CD007784. doi:10.1002/14651858.CD007784.pub3. ISSN 1469-493X. PMID 38018702. PMC 10685396. https://pubmed.ncbi.nlm.nih.gov/38018702.
- ↑ National Cholesterol Education Program (2001). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III): Executive Summary. Bethesda, MD: National Institutes of Health. National Heart, Lung, and Blood Institute. p. 40. NIH Publication No. 01-3670.
- ↑ National Collaborating Centre for Primary Care (2010). NICE clinical guideline 67: Lipid modification. London: National Institute for Health and Clinical Excellence. p. 38. http://www.nice.org.uk/nicemedia/live/11982/40689/40689.pdf.
- ↑ "Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials". Lancet 385 (9976): 1397–1405. April 2015. doi:10.1016/s0140-6736(14)61368-4. PMID 25579834.
- ↑ "Gender related differences in treatment and response to statins in primary and secondary cardiovascular prevention: The never-ending debate". Pharmacological Research 117: 148–155. March 2017. doi:10.1016/j.phrs.2016.12.027. PMID 28012963.
- ↑ 20.0 20.1 20.2 "2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Journal of the American College of Cardiology 73 (24): e285–e350. June 2019. doi:10.1016/j.jacc.2018.11.003. PMID 30423393.
- ↑ 21.0 21.1 21.2 "Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: US Preventive Services Task Force Recommendation Statement". JAMA 316 (19): 1997–2007. November 2016. doi:10.1001/jama.2016.15450. PMID 27838723.
- ↑ "ACC/AHA ASCVD Risk Calculator". http://www.cvriskcalculator.com/.
- ↑ "Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials". Lancet 393 (10170): 407–415. February 2019. doi:10.1016/S0140-6736(18)31942-1. PMID 30712900.
- ↑ 24.0 24.1 "Efficacy of statins for primary prevention in people at low cardiovascular risk: a meta-analysis". CMAJ 183 (16): E1189–E1202. November 2011. doi:10.1503/cmaj.101280. PMID 21989464.
- ↑ "Meta-analysis of statin effects in women versus men". Journal of the American College of Cardiology 59 (6): 572–582. February 2012. doi:10.1016/j.jacc.2011.09.067. PMID 22300691.
- ↑ "Impact of gender in primary prevention of coronary heart disease with statin therapy: a meta-analysis". International Journal of Cardiology 138 (1): 25–31. January 2010. doi:10.1016/j.ijcard.2008.08.001. PMID 18793814.
- ↑ "Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants". Archives of Internal Medicine 170 (12): 1024–1031. June 2010. doi:10.1001/archinternmed.2010.182. PMID 20585067.
- ↑ "Statins for primary prevention of cardiovascular mortality in women: a systematic review and meta-analysis". Preventive Cardiology 13 (2): 84–90. 2010. doi:10.1111/j.1751-7141.2009.00059.x. PMID 20377811.
- ↑ "Cardiovascular disease: risk assessment and reduction, including lipid modification at www.nice.org.uk". 18 July 2014. http://www.nice.org.uk/guidance/cg181/chapter/1-recommendations.
- ↑ "2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation 129 (25 Suppl 2): S1-45. June 2014. doi:10.1161/01.cir.0000437738.63853.7a. PMID 24222016.
- ↑ "Prevention guidelines: bad process, bad outcome". JAMA Internal Medicine 174 (12): 1972–1973. December 2014. doi:10.1001/jamainternmed.2014.3278. PMID 25285604.
- ↑ "[ESC/EAS Guidelines for the management of dyslipidaemias]". Revista Espanola de Cardiologia 64 (12): 1168.e1–1168.e60. December 2011. doi:10.1016/j.rec.2011.09.015. PMID 22115524.
- ↑ 33.0 33.1 33.2 33.3 "Interpretation of the evidence for the efficacy and safety of statin therapy". Lancet 388 (10059): 2532–2561. November 2016. doi:10.1016/S0140-6736(16)31357-5. PMID 27616593.
- ↑ National Institute for Health and Clinical Excellence (March 2010). "Lipid modification – Cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease – Quick reference guide". http://www.nice.org.uk/nicemedia/live/11982/40675/40675.pdf.
- ↑ "Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis". BMJ 326 (7404): 1423–0. June 2003. doi:10.1136/bmj.326.7404.1423. PMID 12829554.
- ↑ "Ongoing challenges for pharmacotherapy for dyslipidemia". Expert Opinion on Pharmacotherapy 16 (3): 347–356. February 2015. doi:10.1517/14656566.2014.986094. PMID 25476544.
- ↑ "Hypertriglyceridemia: the importance of identifying patients at risk". Postgraduate Medicine 128 (8): 848–858. November 2016. doi:10.1080/00325481.2016.1243005. PMID 27710158.
- ↑ "Management of low levels of high-density lipoprotein-cholesterol". Circulation 128 (1): 72–78. July 2013. doi:10.1161/CIRCULATIONAHA.112.000443. PMID 23817482.
- ↑ "Post-stroke dementia - a comprehensive review". BMC Medicine 15 (1): 11. January 2017. doi:10.1186/s12916-017-0779-7. PMID 28095900.
- ↑ "Perioperative statin therapy in patients at high risk for cardiovascular morbidity undergoing surgery: a review". British Journal of Anaesthesia 114 (1): 44–52. January 2015. doi:10.1093/bja/aeu295. PMID 25186819.
- ↑ "Meta-analysis of the effects of statins on perioperative outcomes in vascular and endovascular surgery". Journal of Vascular Surgery 61 (2): 519–532.e1. February 2015. doi:10.1016/j.jvs.2014.10.021. PMID 25498191.
- ↑ "ROCK as a therapeutic target for ischemic stroke". Expert Review of Neurotherapeutics 17 (12): 1167–1177. December 2017. doi:10.1080/14737175.2017.1395700. PMID 29057688.
- ↑ "2017 Taiwan lipid guidelines for high risk patients". Journal of the Formosan Medical Association = Taiwan Yi Zhi 116 (4): 217–248. April 2017. doi:10.1016/j.jfma.2016.11.013. PMID 28242176.
- ↑ Sheng, Xia; Murphy, Michael J.; MacDonald, Thomas M.; Wei, Li (2012-08-30). "The comparative effectiveness of statin therapy in selected chronic diseases compared with the remaining population". BMC Public Health 12 (1): 712. doi:10.1186/1471-2458-12-712. ISSN 1471-2458. PMID 22935195.
- ↑ "Assessing Severity of Statin Side Effects: Fact Versus Fiction". https://www.acc.org/Latest-in-Cardiology/Articles/2018/04/09/13/25/http%3a%2f%2fwww.acc.org%2fLatest-in-Cardiology%2fArticles%2f2018%2f04%2f09%2f13%2f25%2fAssessing-Severity-of-Statin-Side-Effects.
- ↑ Bansal, Agam B.; Cassagnol, Manouchkathe (2023), "HMG-CoA Reductase Inhibitors", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 31194369, http://www.ncbi.nlm.nih.gov/books/NBK542212/, retrieved 2023-11-11
- ↑ Zhang, Xiaodan; Xing, Lu; Jia, Xiaona; Pang, Xiaocong; Xiang, Qian; Zhao, Xia; Ma, Lingyue; Liu, Zhiyan et al. (2020-04-27). "Comparative Lipid-Lowering/Increasing Efficacy of 7 Statins in Patients with Dyslipidemia, Cardiovascular Diseases, or Diabetes Mellitus: Systematic Review and Network Meta-Analyses of 50 Randomized Controlled Trials" (in en). Cardiovascular Therapeutics 2020: e3987065. doi:10.1155/2020/3987065. ISSN 1755-5914.
- ↑ "Lipid-lowering efficacy of atorvastatin". The Cochrane Database of Systematic Reviews 2015 (3): CD008226. March 2015. doi:10.1002/14651858.CD008226.pub3. PMID 25760954.
- ↑ 49.0 49.1 "Statins for children with familial hypercholesterolemia". The Cochrane Database of Systematic Reviews 2019 (11). November 2019. doi:10.1002/14651858.CD006401.pub5. PMID 31696945.
- ↑ "The safety of statins in children". Acta Paediatrica 102 (9): 857–862. September 2013. doi:10.1111/apa.12280. PMID 23631461.
- ↑ "Drug therapy of hypercholesterolaemia in children and adolescents". Drugs 72 (6): 759–772. April 2012. doi:10.2165/11632810-000000000-00000. PMID 22512364.
- ↑ 52.0 52.1 "Preventing early cardiovascular death in patients with familial hypercholesterolemia". The Journal of the American Osteopathic Association 114 (2): 99–108. February 2014. doi:10.7556/jaoa.2014.023. PMID 24481802.
- ↑ "Update on the molecular biology of dyslipidemias". Clinica Chimica Acta; International Journal of Clinical Chemistry 454: 143–185. February 2016. doi:10.1016/j.cca.2015.10.033. PMID 26546829.
- ↑ "Monogenic hypercholesterolemia: new insights in pathogenesis and treatment". The Journal of Clinical Investigation 111 (12): 1795–1803. June 2003. doi:10.1172/JCI18925. PMID 12813012.
- ↑ "Statins in homozygous familial hypercholesterolemia". Current Atherosclerosis Reports 4 (1): 19–25. January 2002. doi:10.1007/s11883-002-0058-7. PMID 11772418.
- ↑ "Statins for the Prevention of Contrast-Induced Nephropathy After Coronary Angiography/Percutaneous Interventions: A Meta-analysis of Randomized Controlled Trials". Journal of Cardiovascular Pharmacology and Therapeutics 20 (2): 181–192. March 2015. doi:10.1177/1074248414549462. PMID 25193735.
- ↑ 57.0 57.1 "Statins for asthma". The Cochrane Database of Systematic Reviews 2020 (7): CD013268. July 2020. doi:10.1002/14651858.CD013268.pub2. PMID 32668027.
- ↑ table adapted from the following source, but check individual references for technical explanations
- Consumer Reports; Drug Effectiveness Review Project (March 2013), "Evaluating statin drugs to treat High Cholesterol and Heart Disease: Comparing Effectiveness, Safety, and Price", Best Buy Drugs (Consumer Reports): p. 9, http://www.consumerreports.org/health/resources/pdf/best-buy-drugs/StatinsUpdate-FINAL.pdf, retrieved 27 March 2013
- ↑ "Interactions between cyclosporin and lipid-lowering drugs: implications for organ transplant recipients". Drugs 63 (4): 367–378. 2003. doi:10.2165/00003495-200363040-00003. PMID 12558459.
- ↑ "FDA Drug Safety Communication: Interactions between certain HIV or hepatitis C drugs and cholesterol-lowering statin drugs can increase the risk of muscle injury". U.S. Food and Drug Administration (FDA). 1 March 2012. https://www.fda.gov/Drugs/DrugSafety/ucm293877.htm. Current URL
- ↑ 61.0 61.1 "Safety of statins: focus on clinical pharmacokinetics and drug interactions". Circulation 109 (23 Suppl 1): III50–III57. June 2004. doi:10.1161/01.CIR.0000131519.15067.1f. PMID 15198967.
- ↑ "FDA adverse event reports on statin-associated rhabdomyolysis". The Annals of Pharmacotherapy 36 (2): 288–295. February 2002. doi:10.1345/aph.1A289. PMID 11847951.
- ↑ "The safety of statins in clinical practice". Lancet 370 (9601): 1781–1790. November 2007. doi:10.1016/S0140-6736(07)60716-8. PMID 17559928.
- ↑ "Statin drug interactions and related adverse reactions". Expert Opinion on Drug Safety 11 (6): 933–946. November 2012. doi:10.1517/14740338.2012.712959. PMID 22866966.
- ↑ "Statin treatment and new-onset diabetes: a review of proposed mechanisms". Metabolism 63 (6): 735–745. June 2014. doi:10.1016/j.metabol.2014.02.014. PMID 24641882.
- ↑ Lehrer S, Rheinstein P. Statins combined with niacin reduce the risk of peripheral neuropathy. Int J Funct Nutr . Sep-Oct 2020;1(1):3 PMID 33330853
- ↑ 67.0 67.1 "Statin adverse effects : a review of the literature and evidence for a mitochondrial mechanism". American Journal of Cardiovascular Drugs 8 (6): 373–418. 2008. doi:10.2165/0129784-200808060-00004. PMID 19159124.
- ↑ "New analysis fuels debate on merits of prescribing statins to low risk people". BMJ 348: g2370. March 2014. doi:10.1136/bmj.g2370. PMID 24671956.
- ↑ "Open letter raises concerns about NICE guidance on statins". BMJ 348: g3937. June 2014. doi:10.1136/bmj.g3937. PMID 24920699.
- ↑ "Muscular adverse effects are common with statins". BMJ 348: g3724. June 2014. doi:10.1136/bmj.g3724. PMID 24920687.
- ↑ "Statin-related adverse events: a meta-analysis". Clinical Therapeutics 28 (1): 26–35. January 2006. doi:10.1016/j.clinthera.2006.01.005. PMID 16490577.
- ↑ 72.0 72.1 "Diagnosis, prevention, and management of statin adverse effects and intolerance: proceedings of a Canadian Working Group Consensus Conference". The Canadian Journal of Cardiology 27 (5): 635–662. 2011. doi:10.1016/j.cjca.2011.05.007. PMID 21963058.
- ↑ "What proportion of symptomatic side effects in patients taking statins are genuinely caused by the drug? Systematic review of randomized placebo-controlled trials to aid individual patient choice". European Journal of Preventive Cardiology 21 (4): 464–474. April 2014. doi:10.1177/2047487314525531. PMID 24623264.
- ↑ "Statins and cognition: a systematic review and meta-analysis of short- and long-term cognitive effects". Mayo Clinic Proceedings 88 (11): 1213–1221. November 2013. doi:10.1016/j.mayocp.2013.07.013. PMID 24095248.
- ↑ "Diagnosis, prevention, and management of statin adverse effects and intolerance: Canadian Working Group Consensus update". The Canadian Journal of Cardiology 29 (12): 1553–1568. December 2013. doi:10.1016/j.cjca.2013.09.023. PMID 24267801.
- ↑ "Statins and cognitive function: a systematic review". Annals of Internal Medicine 159 (10): 688–697. November 2013. doi:10.7326/0003-4819-159-10-201311190-00007. PMID 24247674.
- ↑ "ACP Journal Club. Review: statins are not associated with cognitive impairment or dementia in cognitively intact adults". Annals of Internal Medicine 160 (10): JC11, JC10. May 2014. doi:10.7326/0003-4819-160-10-201405200-02011. PMID 24842433.
- ↑ "Remembering Statins: Do Statins Have Adverse Cognitive Effects?". Diabetes Care 39 (Supplement 2): S253–S259. August 2016. doi:10.2337/dcS15-3022. PMID 27440840.
- ↑ "Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants". Archives of Internal Medicine 170 (12): 1024–1031. June 2010. doi:10.1001/archinternmed.2010.182. PMID 20585067.
- ↑ "Clinical Effectiveness of Statin Therapy After Ischemic Stroke: Primary Results From the Statin Therapeutic Area of the Patient-Centered Research Into Outcomes Stroke Patients Prefer and Effectiveness Research (PROSPER) Study". Circulation 132 (15): 1404–1413. October 2015. doi:10.1161/CIRCULATIONAHA.115.016183. PMID 26246175.
- ↑ "Post-stroke dementia - a comprehensive review". BMC Medicine 15 (1): 11. January 2017. doi:10.1186/s12916-017-0779-7. PMID 28095900.
- ↑ "Statin-related cognitive impairment in the real world: you'll live longer, but you might not like it". JAMA Internal Medicine 174 (12): 1889. December 2014. doi:10.1001/jamainternmed.2014.5376. PMID 25347692.
- ↑ "FDA Drug Safety Communication: Important safety label changes to cholesterol-lowering statin drugs". 19 January 2016. https://www.fda.gov/Drugs/DrugSafety/ucm293101.htm.
- ↑ "Statin-associated muscle symptoms-Managing the highly intolerant". Journal of Clinical Lipidology 11 (1): 24–33. January–February 2017. doi:10.1016/j.jacl.2017.01.006. PMID 28391891.
- ↑ "Why do people not take life-saving medications? The case of statins". Lancet 388 (10048): 943–945. September 2016. doi:10.1016/s0140-6736(16)31532-x. PMID 27598664.
- ↑ "Statin treatment and muscle symptoms: series of randomised, placebo controlled n-of-1 trials". BMJ 372: n135. February 2021. doi:10.1136/bmj.n135. PMID 33627334.
- ↑ "N-of-1 Trial of a Statin, Placebo, or No Treatment to Assess Side Effects". The New England Journal of Medicine 383 (22): 2182–2184. November 2020. doi:10.1056/NEJMc2031173. PMID 33196154.
- ↑ "Placebo and Nocebo Effects". The New England Journal of Medicine 382 (6): 554–561. February 2020. doi:10.1056/NEJMra1907805. PMID 32023375.
- ↑ "Statins in a Distorted Mirror of Media". Current Atherosclerosis Reports 22 (8): 37. June 2020. doi:10.1007/s11883-020-00853-9. PMID 32557172.
- ↑ "Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials". Lancet 376 (9753): 1670–1681. November 2010. doi:10.1016/S0140-6736(10)61350-5. PMID 21067804.
- ↑ "Statin Safety and Associated Adverse Events: A Scientific Statement From the American Heart Association". Arteriosclerosis, Thrombosis, and Vascular Biology 39 (2): e38–e81. February 2019. doi:10.1161/ATV.0000000000000073. PMID 30580575.
- ↑ "Rhabdomyolysis and Other Causes of Myoglobinuria". 20 January 2015. http://www.patient.co.uk/doctor/rhabdomyolysis-and-other-causes-of-myoglobinuria.
- ↑ "Statin-induced rhabdomyolysis: a comprehensive review of case reports". Physiotherapy Canada. Physiotherapie Canada 66 (2): 124–132. 2014. doi:10.3138/ptc.2012-65. PMID 24799748.
- ↑ "Primary and secondary coenzyme Q10 deficiency: the role of therapeutic supplementation". Nutrition Reviews 71 (3): 180–188. March 2013. doi:10.1111/nure.12011. PMID 23452285.
- ↑ "Coenzyme Q10 supplementation in the management of statin-associated myalgia". American Journal of Health-System Pharmacy 74 (11): 786–793. June 2017. doi:10.2146/ajhp160714. PMID 28546301.
- ↑ "SLCO1B1 variants and statin-induced myopathy--a genomewide study". The New England Journal of Medicine 359 (8): 789–799. August 2008. doi:10.1056/NEJMoa0801936. PMID 18650507.
- ↑ 97.0 97.1 "Incidence of hospitalized rhabdomyolysis in patients treated with lipid-lowering drugs". JAMA 292 (21): 2585–2590. December 2004. doi:10.1001/jama.292.21.2585. PMID 15572716.
- ↑ "Role of Cytochrome P450 2C8 in Drug Metabolism and Interactions". Pharmacological Reviews 68 (1): 168–241. January 2016. doi:10.1124/pr.115.011411. PMID 26721703.
- ↑ 99.0 99.1 "The muscle-specific ubiquitin ligase atrogin-1/MAFbx mediates statin-induced muscle toxicity". The Journal of Clinical Investigation 117 (12): 3940–3951. December 2007. doi:10.1172/JCI32741. PMID 17992259.
- ↑ "Statins and tendinopathy: a systematic review". The Medical Journal of Australia 204 (3): 115–21.e1. February 2016. doi:10.5694/mja15.00806. PMID 26866552.
- ↑ "Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials". Lancet 375 (9716): 735–742. February 2010. doi:10.1016/S0140-6736(09)61965-6. PMID 20167359.
- ↑ "Statins for Prevention of Cardiovascular Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force". JAMA 316 (19): 2008–2024. November 2016. doi:10.1001/jama.2015.15629. PMID 27838722.
- ↑ 103.0 103.1 103.2 103.3 "Balancing Primary Prevention and Statin-Induced Diabetes Mellitus Prevention". The American Journal of Cardiology 120 (7): 1122–1128. October 2017. doi:10.1016/j.amjcard.2017.06.054. PMID 28797470. Bibcode: 1981AmJC...48..728H.
- ↑ "Statins and Multiple Noncardiovascular Outcomes: Umbrella Review of Meta-analyses of Observational Studies and Randomized Controlled Trials". Annals of Internal Medicine 169 (8): 543–553. October 2018. doi:10.7326/M18-0808. PMID 30304368.
- ↑ "Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis". JAMA 305 (24): 2556–2564. June 2011. doi:10.1001/jama.2011.860. PMID 21693744.
- ↑ "Statin use and risk of diabetes mellitus in postmenopausal women in the Women's Health Initiative". Archives of Internal Medicine 172 (2): 144–152. January 2012. doi:10.1001/archinternmed.2011.625. PMID 22231607.
- ↑ "Diabetogenic Action of Statins: Mechanisms". Current Atherosclerosis Reports 21 (6): 23. April 2019. doi:10.1007/s11883-019-0780-z. PMID 31037345.
- ↑ "The controversies of statin therapy: weighing the evidence". Journal of the American College of Cardiology 60 (10): 875–881. September 2012. doi:10.1016/j.jacc.2012.07.007. PMID 22902202.
- ↑ "Statins in clinical medicine". Swiss Medical Weekly 141: w13310. 21 November 2011. doi:10.4414/smw.2011.13310. PMID 22101921.
- ↑ "Effect of the magnitude of lipid lowering on risk of elevated liver enzymes, rhabdomyolysis, and cancer: insights from large randomized statin trials". Journal of the American College of Cardiology 50 (5): 409–418. July 2007. doi:10.1016/j.jacc.2007.02.073. PMID 17662392.
- ↑ "Statins and cancer risk: a meta-analysis". JAMA 295 (1): 74–80. January 2006. doi:10.1001/jama.295.1.74. PMID 16391219.
- ↑ "The relationship of statins to rhabdomyolysis, malignancy, and hepatic toxicity: evidence from clinical trials". Current Atherosclerosis Reports 11 (2): 100–104. March 2009. doi:10.1007/s11883-009-0016-8. PMID 19228482.
- ↑ "Statins are associated with reduced risk of esophageal cancer, particularly in patients with Barrett's esophagus: a systematic review and meta-analysis". Clinical Gastroenterology and Hepatology 11 (6): 620–629. June 2013. doi:10.1016/j.cgh.2012.12.036. PMID 23357487.
- ↑ "Association between statin use and colorectal cancer risk: a meta-analysis of 42 studies". Cancer Causes & Control 25 (2): 237–249. February 2014. doi:10.1007/s10552-013-0326-6. PMID 24265089.
- ↑ "Statins are associated with reduced risk of gastric cancer: a meta-analysis". European Journal of Clinical Pharmacology 69 (10): 1855–1860. October 2013. doi:10.1007/s00228-013-1547-z. PMID 23748751.
- ↑ "Statins are associated with reduced risk of gastric cancer: a systematic review and meta-analysis". Annals of Oncology 24 (7): 1721–1730. July 2013. doi:10.1093/annonc/mdt150. PMID 23599253.
- ↑ "Statins and primary liver cancer: a meta-analysis of observational studies". European Journal of Cancer Prevention 22 (3): 229–234. May 2013. doi:10.1097/cej.0b013e328358761a. PMID 23010949.
- ↑ "Association between statin usage and prostate cancer prevention: a refined meta-analysis based on literature from the years 2005-2010". Urologia Internationalis 90 (3): 259–262. 2013. doi:10.1159/000341977. PMID 23052323.
- ↑ "Statin use and risk of prostate cancer: a meta-analysis of observational studies". PLOS ONE 7 (10): e46691. 2012. doi:10.1371/journal.pone.0046691. PMID 23049713. Bibcode: 2012PLoSO...746691B.
- ↑ "Statins and the risk of lung cancer: a meta-analysis". PLOS ONE 8 (2): e57349. 2013. doi:10.1371/journal.pone.0057349. PMID 23468972. Bibcode: 2013PLoSO...857349T.
- ↑ "Statin use and risk of kidney cancer: a meta-analysis of observational studies and randomized trials". British Journal of Clinical Pharmacology 77 (3): 458–465. March 2014. doi:10.1111/bcp.12210. PMID 23879311.
- ↑ "Statin use and risk of breast cancer: a meta-analysis of observational studies". Breast Cancer Research and Treatment 135 (1): 261–269. August 2012. doi:10.1007/s10549-012-2154-x. PMID 22806241.
- ↑ "Statin use and risk of pancreatic cancer: a meta-analysis". Cancer Causes & Control 23 (7): 1099–1111. July 2012. doi:10.1007/s10552-012-9979-9. PMID 22562222.
- ↑ "Statin use and risk of bladder cancer: a meta-analysis". Cancer Causes & Control 24 (4): 769–776. April 2013. doi:10.1007/s10552-013-0159-3. PMID 23361339.
- ↑ Katherine Zeratsky, R.D., L.D., Mayo clinic: article on interference between grapefruit and medication Accessed 1 May 2017
- ↑ "Drug-grapefruit juice interactions". Mayo Clinic Proceedings 75 (9): 933–942. September 2000. doi:10.4065/75.9.933. PMID 10994829.
- ↑ "The grapefruit-drug interaction debate: role of statins". American Family Physician 76 (2): 190, 192; author reply 192. July 2007. PMID 17695563. http://www.aafp.org/afp/2007/0715/p190.html.
- ↑ "Statins and HIV or Hepatitis C Drugs: Drug Safety Communication – Interaction Increases Risk of Muscle Injury". 1 March 2012. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm294294.htm.
- ↑ "Long-term effect of statins on the risk of new-onset osteoporosis: A nationwide population-based cohort study". PLOS ONE 13 (5): e0196713. 2018. doi:10.1371/journal.pone.0196713. PMID 29723231. Bibcode: 2018PLoSO..1396713L.
- ↑ "Effects of Statins on Bone Mineral Density and Fracture Risk: A PRISMA-compliant Systematic Review and Meta-Analysis". Medicine 95 (22): e3042. May 2016. doi:10.1097/MD.0000000000003042. PMID 27258488.
- ↑ "Efficacy of statins for osteoporosis: a systematic review and meta-analysis". Osteoporosis International 28 (1): 47–57. January 2017. doi:10.1007/s00198-016-3844-8. PMID 27888285.
- ↑ "Association Between Cortical Bone Microstructure and Statin Use in Older Women". The Journal of Clinical Endocrinology and Metabolism 104 (2): 250–257. February 2019. doi:10.1210/jc.2018-02054. PMID 30423123.
- ↑ "Diagnosis of osteoporosis in statin-treated patients is dose-dependent". Annals of the Rheumatic Diseases 78 (12): 1706–1711. December 2019. doi:10.1136/annrheumdis-2019-215714. PMID 31558481.
- ↑ "Drug-Induced Peripheral Neuropathy: A Narrative Review". Current Clinical Pharmacology 15 (1): 38–48. 5 May 2020. doi:10.2174/1574884714666190121154813. PMID 30666914.
- ↑ "Statins combined with niacin reduce the risk of peripheral neuropathy". International Journal of Functional Nutrition 1 (1). 9 June 2020. doi:10.3892/ijfn.2020.3. PMID 33330853.
- ↑ "Structural mechanism for statin inhibition of HMG-CoA reductase". Science 292 (5519): 1160–1164. May 2001. doi:10.1126/science.1059344. PMID 11349148. Bibcode: 2001Sci...292.1160I.
- ↑ 137.0 137.1 "The discovery and development of HMG-CoA reductase inhibitors". Journal of Lipid Research 33 (11): 1569–1582. November 1992. doi:10.1016/S0022-2275(20)41379-3. PMID 1464741.
- ↑ "Diurnal variation of cholesterol precursors squalene and methyl sterols in human plasma lipoproteins". Journal of Lipid Research 23 (3): 466–473. March 1982. doi:10.1016/S0022-2275(20)38144-X. PMID 7200504.
- ↑ "Comparison between morning and evening doses of simvastatin in hyperlipidemic subjects. A double-blind comparative study". Arteriosclerosis and Thrombosis 11 (4): 816–826. Jul–Aug 1991. doi:10.1161/01.ATV.11.4.816. PMID 2065035.
- ↑ "Taking simvastatin in the morning compared with in the evening: randomised controlled trial". BMJ 327 (7418): 788. October 2003. doi:10.1136/bmj.327.7418.788. PMID 14525878.
- ↑ "Pharmacodynamic effects and pharmacokinetics of atorvastatin after administration to normocholesterolemic subjects in the morning and evening". Journal of Clinical Pharmacology 36 (7): 604–609. July 1996. doi:10.1002/j.1552-4604.1996.tb04224.x. PMID 8844442.
- ↑ "Mevinolin, an inhibitor of cholesterol synthesis, induces mRNA for low density lipoprotein receptor in livers of hamsters and rabbits". Proceedings of the National Academy of Sciences of the United States of America 83 (21): 8370–8374. November 1986. doi:10.1073/pnas.83.21.8370. PMID 3464957. Bibcode: 1986PNAS...83.8370M.
- ↑ "HMG-CoA reductase inhibitors in chronic heart failure: potential mechanisms of benefit and risk". Drugs 66 (2): 145–154. 2006. doi:10.2165/00003495-200666020-00002. PMID 16451090.
- ↑ "Statin therapy and autoimmune disease: from protein prenylation to immunomodulation". Nature Reviews. Immunology 6 (5): 358–370. May 2006. doi:10.1038/nri1839. PMID 16639429.
- ↑ "Endothelial dysfunction, oxidative stress and inflammation in atherosclerosis: beneficial effects of statins". Current Medicinal Chemistry 14 (2): 243–248. 2007. doi:10.2174/092986707779313381. PMID 17266583.
- ↑ 146.0 146.1 "The pleiotropic effects of statins on endothelial function, vascular inflammation, immunomodulation and thrombogenesis". Atherosclerosis 203 (2): 325–330. April 2009. doi:10.1016/j.atherosclerosis.2008.08.022. PMID 18834985.
- ↑ "Statins and myocardial remodelling: cell and molecular pathways". Expert Reviews in Molecular Medicine 13 (e22): e22. July 2011. doi:10.1017/S1462399411001931. PMID 21718586.
- ↑ "Rho/Rho-associated coiled-coil forming kinase pathway as therapeutic targets for statins in atherosclerosis". Antioxidants & Redox Signaling 20 (8): 1251–1267. March 2014. doi:10.1089/ars.2013.5524. PMID 23919640.
- ↑ "Questions Remain in Cholesterol Research". 15 August 2014. http://www.medpagetoday.com/Endocrinology/GeneralEndocrinology/47224.
- ↑ "Novel aspects of mevalonate pathway inhibitors as antitumor agents". Clinical Cancer Research 18 (13): 3524–3531. July 2012. doi:10.1158/1078-0432.CCR-12-0489. PMID 22529099.
- ↑ "Statins and skeletal muscles toxicity: from clinical trials to everyday practice". Pharmacological Research 88: 107–113. October 2014. doi:10.1016/j.phrs.2014.04.012. PMID 24835295.
- ↑ "Protein prenylation in glucose-induced insulin secretion from the pancreatic islet beta cell: a perspective". Journal of Cellular and Molecular Medicine 12 (1): 164–173. Jan 2008. doi:10.1111/j.1582-4934.2007.00168.x. PMID 18053094.
- ↑ 153.0 153.1 "Pleiotropic effects of statins". Annual Review of Pharmacology and Toxicology 45: 89–118. 2005. doi:10.1146/annurev.pharmtox.45.120403.095748. PMID 15822172.
- ↑ "Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial". JAMA 295 (13): 1556–1565. April 2006. doi:10.1001/jama.295.13.jpc60002. PMID 16533939.
- ↑ "Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein". The New England Journal of Medicine 359 (21): 2195–2207. November 2008. doi:10.1056/NEJMoa0807646. PMID 18997196.
- ↑ "Rosuvastatin, inflammation, C-reactive protein, JUPITER, and primary prevention of cardiovascular disease--a perspective". Drug Design, Development and Therapy 4: 383–413. December 2010. doi:10.2147/DDDT.S10812. PMID 21267417.
- ↑ "Are cardiovascular benefits in statin lipid effects dependent on baseline lipid levels?". Current Atherosclerosis Reports 13 (1): 64–72. February 2011. doi:10.1007/s11883-010-0149-9. PMID 21104458.
- ↑ "Statin therapy in metabolic syndrome and hypertension post-JUPITER: what is the value of CRP?". Current Atherosclerosis Reports 13 (1): 31–42. February 2011. doi:10.1007/s11883-010-0143-2. PMID 21046291.
- ↑ "The JUPITER Trial: responding to the critics". The American Journal of Cardiology 106 (9): 1351–1356. November 2010. doi:10.1016/j.amjcard.2010.08.025. PMID 21029837.
- ↑ "Crystal structure of archaeal HMG-CoA reductase: insights into structural changes of the C-terminal helix of the class-I enzyme". FEBS Letters 593 (5): 543–553. March 2019. doi:10.1002/1873-3468.13331. PMID 30702149.
- ↑ "Review article: inhibition of methanogenic archaea by statins as a targeted management strategy for constipation and related disorders". Alimentary Pharmacology & Therapeutics 43 (2): 197–212. January 2016. doi:10.1111/apt.13469. PMID 26559904.
- ↑ "Archaea in and on the Human Body: Health Implications and Future Directions". PLOS Pathogens 11 (6): e1004833. June 2015. doi:10.1371/journal.ppat.1004833. PMID 26066650.
- ↑ 163.0 163.1 163.2 163.3 163.4 163.5 "Statins". Clinical Lipidology. Elsevier. 2009. pp. 253–280. doi:10.1016/b978-141605469-6.50026-3. ISBN 978-1-4160-5469-6. "The elimination half-life of the statins varies from 1 to 3 hours for lovastatin, simvastatin, pravastatin, and fluvastatin, to 14 to 19 hours for atorvastatin and rosuvastatin (see Table 22-1). The longer the half-life of the statin, the longer the inhibition of reductase and thus a greater reduction in LDL cholesterol. However, the impact of inhibiting cholesterol synthesis persists even with statins that have a relatively short half-life. This is due to their ability to reduce blood levels of lipoproteins, which have a half-life of approximately 2 to 3 days. Because of this, all statins may be dosed once daily. The preferable time of administration is in the evening just before the peak in cholesterol synthesis."
- ↑ "Metabolism of cerivastatin by human liver microsomes in vitro. Characterization of primary metabolic pathways and of cytochrome P450 isozymes involved". Drug Metabolism and Disposition 25 (3): 321–331. March 1997. PMID 9172950. http://dmd.aspetjournals.org/cgi/pmidlookup?view=long&pmid=9172950.
- ↑ "Comparison of cytochrome P-450-dependent metabolism and drug interactions of the 3-hydroxy-3-methylglutaryl-CoA reductase inhibitors lovastatin and pravastatin in the liver". Drug Metabolism and Disposition 27 (2): 173–179. February 1999. PMID 9929499. http://dmd.aspetjournals.org/cgi/pmidlookup?view=long&pmid=9929499. Retrieved 8 November 2018.
- ↑ "Triveram" (in it) (PDF). https://farmaci.agenziafarmaco.gov.it/aifa/servlet/PdfDownloadServlet?pdfFileName=footer_000049_043427_FI.pdf&retry=0&sys=m0b1l3.
- ↑ "Triveram (2)" (in it) (PDF). https://farmaci.agenziafarmaco.gov.it/aifa/servlet/PdfDownloadServlet?pdfFileName=footer_000049_043427_RCP.pdf&retry=0&sys=m0b1l3.
- ↑ "Riclassificazione del medicinale per uso umano "Triveram", ai sensi dell'articolo 8, comma 10, della legge 24 dicembre 1993, n. 537. (Determina n. DG/1422/2019). (19A06231)" (in it). GU Serie Generale n.238. 10 October 2019. https://www.gazzettaufficiale.it/eli/id/2019/10/10/19A06231/SG.
- ↑ "Cholecomb" (in it) (PDF). https://farmaci.agenziafarmaco.gov.it/aifa/servlet/PdfDownloadServlet?pdfFileName=footer_001820_043496_FI.pdf&retry=0&sys=m0b1l3.
- ↑ "Cholecomb (2)" (in it) (PDF). https://farmaci.agenziafarmaco.gov.it/aifa/servlet/PdfDownloadServlet?pdfFileName=footer_001820_043496_RCP.pdf&retry=0&sys=m0b1l3.
- ↑ "Rosumibe" (in it) (PDF). https://farmaci.agenziafarmaco.gov.it/aifa/servlet/PdfDownloadServlet?pdfFileName=footer_000194_045350_RCP.pdf&retry=0&sys=m0b1l3.
- ↑ "Rosumibe (2)" (in it) (PDF). https://farmaci.agenziafarmaco.gov.it/aifa/servlet/PdfDownloadServlet?pdfFileName=footer_000194_045350_FI.pdf&retry=0&sys=m0b1l3.
- ↑ "Guidelines for lowering lipids to reduce coronary artery disease risk: a comparison of rosuvastatin with atorvastatin, pravastatin, and simvastatin for achieving lipid-lowering goals". The American Journal of Cardiology 91 (5A): 11C–17C; discussion 17C–19C. March 2003. doi:10.1016/S0002-9149(03)00004-3. PMID 12646338.
- ↑ "Influence of ST 789 on murine thymocytes: a flow cytometry study of thymocyte subset distribution and of intracellular free Ca++ increase upon activation. Murine thymocytes and ST 789". Thymus 19 (2 Suppl 1): S53–S61. February 2005. doi:10.1111/j.1742-1241.2005.00461.x. PMID 1585420.
- ↑ "Chinese red yeast rice (Monascus purpureus) for primary hyperlipidemia: a meta-analysis of randomized controlled trials". Chinese Medicine 1 (1): 4. November 2006. doi:10.1186/1749-8546-1-4. PMID 17302963.
- ↑ "Patent expires today on pharmaceutical superstar Lipitor". 31 October 2019. https://www.zdnet.com/article/patent-expires-today-on-pharmaceutical-superstar-lipitor/.
- ↑ "Sandoz launches authorized fluvastatin generic in US". 31 October 2019. http://www.gabionline.net/Generics/News/Sandoz-launches-authorized-fluvastatin-generic-in-US.
- ↑ "Teva Announces Final Approval of Lovastatin Tablets". Teva Pharmaceutical Industries Ltd. (Press release). 31 October 2019. Archived from the original on 31 October 2019. Retrieved 31 October 2019.
- ↑ "FDA OKs Generic Version of Pravachol". 25 April 2006. https://www.webmd.com/cholesterol-management/news/20060425/fda-oks-generic-version-pravachol.
- ↑ "Generic Crestor Wins Approval, Dealing a Blow to AstraZeneca". 21 July 2016. https://www.nytimes.com/2016/07/21/business/generic-crestor-wins-approval-dealing-a-blow-to-astrazeneca.html.
- ↑ "Drug Firms Face Billions in Losses as Patents End". 6 March 2011. https://www.nytimes.com/2011/03/07/business/07drug.html.
- ↑ "Merck Loses Protection for Patent on Zocor". 23 June 2006. https://www.nytimes.com/2006/06/23/business/23statin.html.
- ↑ "A century of cholesterol and coronaries: from plaques to genes to statins". Cell 161 (1): 161–172. March 2015. doi:10.1016/j.cell.2015.01.036. PMID 25815993.
- ↑ The cholesterol wars: the skeptics vs. the preponderance of evidence. Academic Press. 2007. pp. 6–9. ISBN 978-0-12-373979-7.
- ↑ "A historical perspective on the discovery of statins". Proceedings of the Japan Academy. Series B, Physical and Biological Sciences 86 (5): 484–493. 2010. doi:10.2183/pjab.86.484. PMID 20467214. Bibcode: 2010PJAB...86..484E.
- ↑ "Crystal and molecular structure of compactin, a new antifungal metabolite from Penicillium brevicompactum". Journal of the Chemical Society, Perkin Transactions 1 (11): 1165–1170. 1976. doi:10.1039/P19760001165. PMID 945291.
- ↑ Scandinaviansimvastatinsurvival (November 1994). "Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S)". Lancet 344 (8934): 1383–1389. doi:10.1016/S0140-6736(94)90566-5. PMID 7968073.
- ↑ "National Inventors Hall of Fame Honors 2012 Inductees". 8 May 2012. http://news.thomasnet.com/IMT/2012/05/08/2012-inventors-hall-of-fame-inductees/.
- ↑ "How One Scientist Intrigued by Molds Found First Statin". The Wall Street Journal. 9 January 2006. https://www.wsj.com/articles/SB113677121574341250.
- ↑ "Statins prevent 80,000 heart attacks and strokes a year in UK, study finds". The Guardian. 8 September 2016. https://www.theguardian.com/society/2016/sep/08/statins-prevent-80000-heart-attacks-and-strokes-a-year-in-uk-study-finds.
- ↑ "Nissen Calls Statin Denialism A Deadly Internet-Driven Cult". CardioBrief. 24 July 2017. http://www.cardiobrief.org/2017/07/24/nissen-calls-statin-denialism-a-deadly-internet-driven-cult/.
- ↑ "Statin Denialism". Skeptical Inquirer 41 (3): 40–43. 2017. https://skepticalinquirer.org/2017/05/statin_denialism/. Retrieved 6 October 2018.
- ↑ "First-Time Generics – December 2001". https://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/DrugandBiologicApprovalReports/ANDAGenericDrugApprovals/ucm063397.htm.
- ↑ "Lovastatin: FDA-Approved Drugs". https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=075300.
- ↑ "ANDA Approval Reports - First-Time Generics - December 2001". http://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/DrugandBiologicApprovalReports/ANDAGenericDrugApprovals/ucm063397.htm.
- ↑ "First-Time Generics – April 2006". https://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/DrugandBiologicApprovalReports/ANDAGenericDrugApprovals/ucm064074.htm.
- ↑ "Pravastatin: FDA-Approved Drugs". https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=076056.
- ↑ "ANDA Approval Reports - First-Time Generics - April 2006". http://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/DrugandBiologicApprovalReports/ANDAGenericDrugApprovals/ucm064074.htm.
- ↑ "First-Time Generics – June 2006". https://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/DrugandBiologicApprovalReports/ANDAGenericDrugApprovals/ucm064061.htm.
- ↑ "Simvastatin: FDA-Approved Drugs". https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=076052.
- ↑ "ANDA Approval Reports - First-Time Generics - June 2006". http://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/DrugandBiologicApprovalReports/ANDAGenericDrugApprovals/ucm064061.htm.
- ↑ "FAQ: Generic Lipitor". 29 November 2011. https://www.webmd.com/cholesterol-management/news/20111129/faq-generic-lipitor.
- ↑ "First-Time Generic Drug Approvals – November 2011". https://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/DrugandBiologicApprovalReports/ANDAGenericDrugApprovals/ucm282392.htm.
- ↑ "Atorvastatin: FDA-Approved Drugs". https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=076477.
- ↑ "ANDA Approval Reports - First-Time Generic Drug Approvals - November 2011". http://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/DrugandBiologicApprovalReports/ANDAGenericDrugApprovals/ucm282392.htm.
- ↑ "First-Time Generic Drug Approvals – April 2012". https://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/DrugandBiologicApprovalReports/ANDAGenericDrugApprovals/ucm312283.htm.
- ↑ "ANDA Approval Reports - First-Time Generic Drug Approvals - April 2012". http://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/DrugandBiologicApprovalReports/ANDAGenericDrugApprovals/ucm312283.htm.
- ↑ "ANDA (Generic) Drug Approvals in 2016". 3 November 2018. https://www.fda.gov/drugs/first-generic-drug-approvals/anda-generic-drug-approvals-2016.
- ↑ "FDA approves first generic Crestor". U.S. Food and Drug Administration (FDA) (Press release). 29 April 2016. Retrieved 26 April 2020.
- ↑ "CDER 2017 First Generic Drug Approvals". 3 November 2018. https://www.fda.gov/drugs/first-generic-drug-approvals/2017-first-generic-drug-approvals.
- ↑ "Simvastatin is associated with a reduced incidence of dementia and Parkinson's disease". BMC Medicine 5 (1): 20. July 2007. doi:10.1186/1741-7015-5-20. PMID 17640385.
- ↑ "Statins reduce the risk of lung cancer in humans: a large case-control study of US veterans". Chest 131 (5): 1282–1288. May 2007. doi:10.1378/chest.06-0931. PMID 17494779.
- ↑ "Statin use and incident nuclear cataract". JAMA 295 (23): 2752–2758. June 2006. doi:10.1001/jama.295.23.2752. PMID 16788130.
- ↑ "Reduction in blood pressure with statins: results from the UCSD Statin Study, a randomized trial". Archives of Internal Medicine 168 (7): 721–727. April 2008. doi:10.1001/archinte.168.7.721. PMID 18413554.
- ↑ "Statins, the renin-angiotensin-aldosterone system and hypertension - a tale of another beneficial effect of statins". Journal of the Renin-Angiotensin-Aldosterone System 15 (3): 250–258. September 2014. doi:10.1177/1470320314531058. PMID 25037529.
- ↑ "Association of statin use with pathological tumor characteristics and prostate cancer recurrence after surgery". The Journal of Urology 185 (4): 1268–1273. April 2011. doi:10.1016/j.juro.2010.11.089. PMID 21334020.
- ↑ "The relationship between statins and breast cancer prognosis varies by statin type and exposure time: a meta-analysis". Breast Cancer Research and Treatment 164 (1): 1–11. July 2017. doi:10.1007/s10549-017-4246-0. PMID 28432513.
- ↑ "The Use of Statins and Risk of Community-Acquired Pneumonia". Current Infectious Disease Reports 19 (8): 26. August 2017. doi:10.1007/s11908-017-0581-x. PMID 28639080.
- ↑ "Statins for multiple sclerosis". The Cochrane Database of Systematic Reviews 2011 (12): CD008386. December 2011. doi:10.1002/14651858.CD008386.pub3. PMID 22161428.
External links
- "Statins". UK. 3 October 2018. https://www.nhs.uk/conditions/statins/.
- "Weighing the Pros and Cons of Statins". 16 April 2018. https://www.nytimes.com/2018/04/16/well/weighing-the-pros-and-cons-of-statins.html.
- "FDA requests removal of strongest warning against using cholesterol-lowering statins during pregnancy; still advises most pregnant patients should stop taking statins". 30 August 2021. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requests-removal-strongest-warning-against-using-cholesterol-lowering-statins-during-pregnancy.
 |
