Medicine:Oculocerebrorenal syndrome
| Oculocerebrorenal syndrome | |
|---|---|
| Other names | Lowe syndrome |
 | |
| Infant with oculocerebrorenal syndrome | |
| Symptoms | Cataracts[1] |
| Causes | Mutations in OCRL gene[1] |
| Diagnostic method | MRI, urinalysis[2] |
| Treatment | Physical therapy, clomipramine[3] |
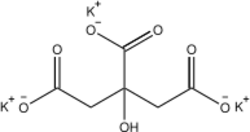
Oculocerebrorenal syndrome (also called Lowe syndrome) is a rare X-linked recessive disorder characterized by congenital cataracts, hypotonia, intellectual disability, proximal tubular acidosis, aminoaciduria and low-molecular-weight proteinuria. Lowe syndrome can be considered a cause of Fanconi syndrome (bicarbonaturia, renal tubular acidosis, potassium loss and sodium loss[4]).[5][6]
Signs and symptoms
Boys with Lowe syndrome are born with cataracts in both eyes; glaucoma is present in about half of the individuals with Lowe syndrome, though usually not at birth. While not present at birth, kidney problems develop in many affected boys at about one year of age.[1] Renal pathology is characterized by an abnormal loss of certain substances into the urine, including bicarbonate, sodium, potassium, amino acids, organic acids, albumin, calcium and L-carnitine. This problem is known as Fanconi-type renal tubular dysfunction.
Genetics
This syndrome is caused by mutations in the OCRL gene which encodes an inositol polyphosphate-5-phosphatase. At least one mechanism by which these mutations cause this syndrome is by loss of its Rab-binding domain.[7][8]
This protein is associated with the primary cilia of the retinal pigment epithelial cells, fibroblasts and kidney tubular cells. This suggests that this syndrome is due to dysfunction of the cilia in these cells.[8] About 120 mutations are associated with this condition and OCRL gene which is associated with oculocerebrorenal syndrome[9]
-
Fibroblasts
-
X-link recessive inheritance
Diagnosis
Diagnosis of oculocerebrorenal syndrome can be done via genetic testing[10] Among the different investigations that can de done are:[2]
- Urinalysis
- MRI
- Blood test
Treatment
In terms of treatment of oculocerebrorenal syndrome for those individuals who are affected by this condition includes the following:[3]
- Glaucoma control (via medication)
- Nasogastric tube feeding
- Physical therapy
- Clomipramine
- Potassium citrate
Epidemiology
Because oculocerebrorenal syndrome is an X-linked recessive condition, the disease develops mostly in men with very rare occurrences in women, while women are carriers of the disease; it has an estimated prevalence of 1 in 500,000 people.[11]
History
It was first described in 1952 by American paediatrician Charles Upton Lowe (August 24, 1921 – February 9, 2012)[12][13] and colleagues at the Massachusetts General Hospital in Boston.[14] Because of the three major organ systems involved (eyes, brain and kidney), it is known as oculocerebrorenal syndrome.[1]
See also
References
- ↑ 1.0 1.1 1.2 1.3 Oculocerebrorenal Syndrome: Background, Pathophysiology, Epidemiology. 2016-06-01. http://emedicine.medscape.com/article/1214184-overview.
- ↑ 2.0 2.1 "Lowe's (Oculo-Cerebro-Renal) Syndrome | Doctor | Patient". http://patient.info/doctor/lowe-(oculo-cerebro-renal)-syndrome.htm.
- ↑ 3.0 3.1 RESERVED, INSERM US14 -- ALL RIGHTS. "Orphanet: Oculocerebrorenal syndrome of Lowe". http://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=EN&Expert=534.
- ↑ "Fanconi syndrome: MedlinePlus Medical Encyclopedia". https://medlineplus.gov/ency/article/000333.htm.
- ↑ Lewis, Richard Alan; Nussbaum, Robert L.; Brewer, Eileen D. (1993-01-01). "Lowe Syndrome". in Pagon, Roberta A.. GeneReviews. Seattle (WA): University of Washington, Seattle. https://www.ncbi.nlm.nih.gov/books/NBK1480/.update 2012
- ↑ "OMIM Entry - # 309000 - LOWE OCULOCEREBRORENAL SYNDROME; OCRL". https://omim.org/entry/309000.
- ↑ Hagemann, Nina; Hou, Xiaomin; Goody, Roger S.; Itzen, Aymelt; Erdmann, Kai S. (2017-06-01). "Crystal structure of the Rab binding domain of OCRL1 in complex with Rab8 and functional implications of the OCRL1/Rab8 module for Lowe syndrome". Small GTPases 3 (2): 107–110. doi:10.4161/sgtp.19380. ISSN 2154-1256. PMID 22790198.
- ↑ 8.0 8.1 Reference, Genetics Home. "Lowe syndrome". https://ghr.nlm.nih.gov/condition/lowe-syndrome.
- ↑ Reference, Genetics Home. "OCRL gene". https://ghr.nlm.nih.gov/gene/OCRL#conditions.
- ↑ "Lowe syndrome - Conditions - GTR - NCBI". https://www.ncbi.nlm.nih.gov/gtr/conditions/C0028860/.
- ↑ Loi M (2006). "Lowe Syndrome". Orphanet Journal of Rare Diseases 1: 16. doi:10.1186/1750-1172-1-16. PMID 16722554.
- ↑ Kelly, Evelyn B. (2013) (in en). Encyclopedia of human genetics and disease. Santa Barbara, Calif.: Greenwood. ISBN 9780313387142. https://books.google.com/books?id=SjfKybobUIYC&q=Charles+Upton+Lowe+Oculocerebrorenal+syndrome&pg=PA498. Retrieved 21 December 2016.
- ↑ Loring, David W.; Bowden, Stephen (2015) (in en). INS Dictionary of Neuropsychology and Clinical Neurosciences. Oxford University Press, Incorporated. ISBN 9780195366457. https://books.google.com/books?id=Vi5mBgAAQBAJ&q=Charles+Upton+Lowe+named+for+Lowe++syndrome&pg=PA268. Retrieved 21 December 2016.
- ↑ "Organic-aciduria, decreased renal ammonia production, hydrophthalmos, and mental retardation; a clinical entity". American Journal of Diseases of Children 83 (2): 164–84. 1952. doi:10.1001/archpedi.1952.02040060030004. PMID 14884753.
Further reading
- Bökenkamp, Arend; Ludwig, Michael (1 January 2016). "The oculocerebrorenal syndrome of Lowe: an update". Pediatric Nephrology (Berlin, Germany) 31 (12): 2201–2212. doi:10.1007/s00467-016-3343-3. ISSN 0931-041X. PMID 27011217.
External links
| Classification | |
|---|---|
| External resources |
 |



