Medicine:Lysinuric protein intolerance
| Lysinuric protein intolerance | |
|---|---|
| Other names | Hyperdibasic aminoaciduria type 2,Cationic aminoaciduria or Familial protein intolerance |
 | |
| Lysine | |
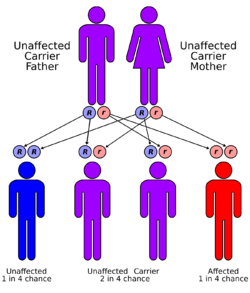
Lysinuric protein intolerance (LPI) is an autosomal recessive[1] metabolic disorder affecting amino acid transport. It is characterised by the body's inability to properly digest and use certain proteins. [2] This condition leads to various metabolic complications and is typically diagnosed in infancy or early childhood.[3]
About 140 patients have been reported, almost half of them of Finnish origin. Individuals from Japan, Italy, Morocco and North Africa have also been reported plus one in Bixby, Oklahoma.
Signs and symptoms
Infants with LPI are usually symptom-free when breastfed because of the low protein concentration in human milk, but develop vomiting and diarrhea after weaning. The patients show failure to thrive, poor appetite, growth retardation, enlarged liver and spleen, prominent osteoporosis and osteopenia,[4] delayed bone age and spontaneous protein aversion. Forced feeding of protein may lead to convulsions and coma. Mental development is normal if prolonged episode of hyperammonemia can be avoided. Some patients develop severe pulmonary and kidney complications. High levels of plasma glutamine and glycine are observed.
Genetic Basis
LPI has been associated with SLC7A7.[5] LPI is caused by mutations in the SLC7A7 gene, which encodes for a protein involved in the transport of amino acids across cell membranes. Mutations in this gene impair the transport function, leading to the characteristic amino acid imbalances seen in LPI patients.[6]
Mechanism
Clinical Features
The symptoms of LPI typically appear after weaning from breast milk to a protein-rich diet. Common symptoms include poor growth, muscle weakness, enlarged liver and spleen, and frequent infections. Neurological symptoms such as confusion and seizures can also occur.[7]
Diagnosis
The diagnosis is based on the biochemical findings (increased concentrations of lysine, arginine and ornithine in urine and low concentrations of these amino acids in plasma, elevation of urinary orotic acid excretion after protein-rich meals, and inappropriately high concentrations of serum ferritin and lactate dehydrogenase isoenzymes) and the screening of known mutations of the causative gene from a DNA sample.[8]
Treatment
Treatment of LPI consists of protein-restricted diet and supplementation with oral citrulline.[9] Citrulline is a neutral amino acid that improves the function of the urea cycle and allows sufficient protein intake without hyperammonemia.[10]
Prognosis
Under proper dietary control and supplementation, the majority of the LPI patients are able to have a nearly normal life. However, severe complications including pulmonary alveolar proteinosis and chronic kidney disease may develop even with proper treatment.[11]Fertility appears to be normal in women, but mothers with LPI have an increased risk for complications during pregnancy and delivery.[12]
References
- ↑ "Lysinuric protein intolerance" (Free full text). The American Journal of Medicine 59 (2): 229–240. August 1975. doi:10.1016/0002-9343(75)90358-7. PMID 1155480. http://toxnet.nlm.nih.gov/cgi-bin/sis/search/r?dbs+hsdb:@term+@rn+56-41-7.
- ↑ Simell, O. (1990), "Lysinuric Protein Intolerance", Inborn Metabolic Diseases (Berlin, Heidelberg: Springer Berlin Heidelberg): pp. 577–583, doi:10.1007/978-3-662-02613-7_44, ISBN 978-3-662-02615-1, http://dx.doi.org/10.1007/978-3-662-02613-7_44, retrieved 2024-07-22
- ↑ Simell, O. (1990), "Lysinuric Protein Intolerance", Inborn Metabolic Diseases (Berlin, Heidelberg: Springer Berlin Heidelberg): pp. 577–583, doi:10.1007/978-3-662-02613-7_44, ISBN 978-3-662-02615-1, http://dx.doi.org/10.1007/978-3-662-02613-7_44, retrieved 2024-07-22
- ↑ Online Mendelian Inheritance in Man (OMIM) 222700
- ↑ "SLC7A7, encoding a putative permease-related protein, is mutated in patients with lysinuric protein intolerance". Nat. Genet. 21 (3): 297–301. March 1999. doi:10.1038/6815. PMID 10080183.
- ↑ Borsani, Giuseppe; Bassi, Maria Teresa; Sperandeo, Maria Pia; Grandi, Alessandro De; Buoninconti, Anna; Riboni, Mirko; Manzoni, Marta; Incerti, Barbara et al. (March 1999). "SLC7A7, encoding a putative permease-related protein, is mutated in patients with lysinuric protein intolerance". Nature Genetics 21 (3): 297–301. doi:10.1038/6815. ISSN 1061-4036. PMID 10080183. http://dx.doi.org/10.1038/6815.
- ↑ Douda, David N; Farmakovski, Nicole; Dell, Sharon; Grasemann, Hartmut; Palaniyar, Nades (December 2009). "SP-D counteracts GM-CSF-mediated increase of granuloma formation by alveolar macrophages in lysinuric protein intolerance". Orphanet Journal of Rare Diseases 4 (1): 29. doi:10.1186/1750-1172-4-29. ISSN 1750-1172. PMID 20030831.
- ↑ Sebastio, Gianfranco; Schiff, Manuel; de Baulny, Hélène Ogier (September 2016). "Lysinuric Protein Intolerance and Hartnup Disease". Oxford Medicine Online. doi:10.1093/med/9780199972135.003.0025. http://dx.doi.org/10.1093/med/9780199972135.003.0025.
- ↑ Nunes, Virginia; Niinikoski, Harri (1993). "Lysinuric Protein Intolerance". University of Washington, Seattle. https://www.ncbi.nlm.nih.gov/books/NBK1361/.
- ↑ Sebastio, Gianfranco; Schiff, Manuel; de Baulny, Hélène Ogier (September 2016). "Lysinuric Protein Intolerance and Hartnup Disease". Oxford Medicine Online. doi:10.1093/med/9780199972135.003.0025. http://dx.doi.org/10.1093/med/9780199972135.003.0025.
- ↑ "Nephropathy advancing to end-stage renal disease: a novel complication of lysinuric protein intolerance". J. Pediatr. 150 (6): 161–164. June 2007. doi:10.1016/j.jpeds.2007.01.043. PMID 17517249.
- ↑ "Hazards associated with pregnancies and deliveries in lysinuric protein intolerance". Metabolism 55 (2): 224–231. February 2006. doi:10.1016/j.metabol.2005.08.016. PMID 16423630.
External links
| Classification | |
|---|---|
| External resources |
 |
