Medicine:Post-polio syndrome
| Post-polio syndrome | |
|---|---|
| Other names | Post-poliomyelitis syndrome, Post-polio sequelae |
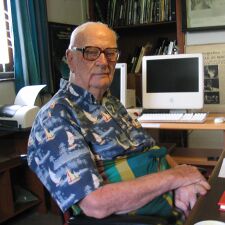 | |
| Science fiction writer Arthur C. Clarke developed post-polio syndrome in 1988 after initially contracting polio in 1962.[1] | |
Post-polio syndrome (PPS, poliomyelitis sequelae) is a group of latent symptoms of poliomyelitis (polio), occurring at about a 25–40% rate (latest data greater than 80%). These symptoms are caused by the damaging effects of the viral infection on the nervous system. Symptoms typically occur 15 to 30 years after an initial acute paralytic attack. Symptoms include decreasing muscular function or acute weakness with pain and fatigue. The same symptoms may also occur years after a nonparalytic polio (NPP) infection.
The precise mechanism that causes PPS is unknown. It shares many features with chronic fatigue syndrome, but unlike that disorder it tends to be progressive and can cause loss of muscle strength. Treatment is primarily limited to adequate rest, conservation of available energy, and supportive measures, such as leg braces and energy-saving devices such as powered wheelchairs, analgesia (pain relief), and sleep aids.
Signs and symptoms
After a period of prolonged stability, individuals who had been infected and recovered from polio begin to experience new signs and symptoms, characterised by muscular atrophy (decreased muscle mass), weakness, pain, and fatigue in limbs that were originally affected or in limbs that did not seem to have been affected at the time of the initial polio illness.[2] PPS is a very slowly progressing condition marked by periods of stability followed by new declines in the ability to carry out usual daily activities.[3] Most patients become aware of their decreased capacity to carry out daily routines due to significant changes in mobility and decreasing upper limb function and lung capability. Fatigue is often the most disabling symptom; even slight exertion often produces disabling fatigue and can also intensify other symptoms.[4] Problems breathing or swallowing, sleep-related breathing disorders, such as sleep apnea, and decreased tolerance for cold temperatures are other notable symptoms.[2]
Increased activity during healthy years between the original infection and onset of PPS can amplify the symptoms. Thus, contracting polio at a young age can result in particularly disabling PPS symptoms.[5]
A possible early occurring and long-lasting sign is a slight jitter exhibited in handwriting.[citation needed]
Mechanism
Numerous theories have been proposed to explain post-polio syndrome. Despite this, no absolutely defined causes of PPS are known. The most widely accepted theory of the mechanism behind the disorder is "neural fatigue". A motor unit is a nerve cell (or neuron) and the muscle fibers it activates. Poliovirus attacks specific neurons in the brainstem and the anterior horn cells of the spinal cord, generally resulting in the death of a substantial fraction of the motor neurons controlling skeletal muscles. In an effort to compensate for the loss of these neurons, surviving motor neurons sprout new nerve terminals to the orphaned muscle fibers. The result is some recovery of movement and the development of enlarged motor units.[3]
The neural fatigue theory proposes that the enlargement of the motor neuron fibers places added metabolic stress on the nerve cell body to nourish the additional fibers. After years of use, this stress may be more than the neuron can handle, leading to the gradual deterioration of the sprouted fibers, and eventually, the neuron itself. This causes muscle weakness and paralysis. Restoration of nerve function may occur in some fibers a second time, but eventually, nerve terminals malfunction and permanent weakness occurs.[3] When these neurons no longer carry on sprouting, fatigue occurs due to the increasing metabolic demand of the nervous system.[6] The normal aging process also may play a role. Denervation and reinnervation are going on, but the reinnervation process has an upper limit where the reinnervation cannot compensate for the ongoing denervation, and loss of motor units takes place.[7] What disturbs the denervation-reinnervation equilibrium and causes peripheral denervation, though, is still unclear. With age, most people experience a decrease in the number of spinal motor neurons. Because polio survivors have already lost a considerable number of motor neurons, further age-related loss of neurons may contribute substantially to new muscle weakness. The overuse and underuse of muscles also may contribute to muscle weakness.[8]
Another theory is that people who have recovered from polio lose remaining healthy neurons at a faster rate than normal. However, little evidence exists to support this idea.[9] Finally, the initial polio infection is thought to cause an autoimmune reaction, in which the body's immune system attacks normal cells as if they were foreign substances. Again, compared to neural fatigue, the evidence supporting this theory is quite limited.[9]
Diagnosis
Diagnosis of PPS can be difficult, since the symptoms are hard to separate from complications due to the original polio infection, and from the normal infirmities of aging. No laboratory test for post-polio syndrome is known, nor are any other specific diagnostic criteria. Three important criteria are recognized, including previous diagnosis of polio, long interval after recovery, and gradual onset of weakness.[10]
In general, PPS is a diagnosis of exclusion whereby other possible causes of the symptoms are eliminated.[11] Neurological examination aided by other laboratory studies can help to determine what component of a neuromuscular deficit occurred with polio and what components are new and to exclude all other possible diagnoses. Objective assessment of muscle strength in PPS patients may not be easy. Changes in muscle strength are determined in specific muscle groups using various muscle scales that quantify] strength, such as the Medical Research Council (MRC) scale. magnetic resonance imaging, neuroimaging, and electrophysiological studies, muscle biopsies, or spinal fluid analysis may also be useful in establishing a PPS diagnosis.[11]
Management
PPS treatment concerns comfort (relieving pain via analgesics) and rest (via use of mechanisms to make life easier, such as a powered wheelchair) and is generally of palliative care. No reversive therapies are known. Fatigue is usually the most disabling symptom. Energy conservation can significantly reduce fatigue episodes. Such can be achieved by lifestyle changes, such as additional (daytime) sleep, reducing workload, and weight loss for obesity. Some require lower-limb orthotics to reduce energy usage.[citation needed]
Medications for fatigue, such as amantadine and pyridostigmine, are ineffective in the management of PPS.[12] Muscle strength and endurance training are more important in managing the symptoms of PPS than the ability to perform enduring aerobic activity. Management should focus on treatments such as hydrotherapy and developing other routines that encourage strength, but do not affect fatigue levels.[6] A recent trend toward use of intravenous immunoglobulin, which had yielded promising albeit modest results,[13] but (As of 2010) proves insufficient to recommend as a treatment.[12]
PPS increasingly stresses the musculoskeletal system from progressive muscular atrophy. In a review of 539 PPS patients, 80% reported pain in muscles and joints and 87% had fatigue.[14] Joint instability can cause appreciable pain and should be adequately treated with painkillers. Directed activity, such as decreasing mechanical stress with braces and adaptive equipment, is recommended.[4][6]
Because PPS can fatigue facial muscles, as well as cause dysphagia (difficulty swallowing), dysarthria (difficulty speaking) or aphonia (inability to produce speech), persons may become malnourished from difficulty eating. Compensatory routines can help relieve these symptoms, such as eating smaller portions at a time and sitting down whilst eating.[15] PPS with respiratory involvement requires exceptional therapy management, such as breathing exercises and chest percussion to expel secretions (clearing of the lungs) on a periodic basis (monitored via stethoscope). Failure to properly assess PPS with respiratory involvement can increase the risk of overlooking an aspiration pneumonia (a life-threatening infection of the lower respiratory tract, especially so if not caught early on). Severe cases may require permanent ventilation or tracheostomy. Sleep apnoea may also occur. Other management strategies that show improvement include smoking cessation, treatment of other respiratory diseases, and vaccination against respiratory infections such as influenza.[4]
Prognosis
In general, PPS is not life-threatening. The major exception is patients left with severe residual respiratory difficulties, who may experience new severe respiratory impairment. Compared to control populations, PPS patients lack any elevation of antibodies against the poliovirus, and because no poliovirus is excreted in the feces, it is not considered a recurrence of the original polio. Further, no evidence has shown that the poliovirus can cause a persistent infection in humans. PPS has been confused with amyotrophic lateral sclerosis (ALS), which progressively weakens muscles. PPS patients do not have an elevated risk of ALS.[6]
No sufficient longitudinal studies have been conducted on the prognosis of PPS, but speculations have been made by several physicians based on experience. Fatigue and mobility usually return to normal over a long period of time. The prognosis also differs depending upon different causes and factors affecting the individual.[5] An overall mortality rate of 25% exists due to possible respiratory paralysis of persons with PPS; otherwise, it is usually not lethal.[16]
Prognosis can be abruptly changed for the worse by the use of anesthesia, such as during surgery.[17]
Epidemiology
Old data show PPS occurs in roughly 25 to 50% of people who survive a polio infection.[18] However, newer data from countries that have contacted their polio survivors have shown 85% of their polio survivors to have symptoms of post polio syndrome.[19] Typically, it occurs 30–35 years afterwards, but delays between 8 and 71 years have been recorded.[20][21] The disease occurs sooner in persons with more severe initial infections.[21] Other factors that increase the risk of PPS include increasing length of time since acute poliovirus infection, presence of permanent residual impairment after recovery from the acute illness,[20][21] and being female.[22] PPS is documented to occur in cases of nonparalytic polio (NPP). One review states late-onset weakness and fatigue occur in 14–42% of NPP patients.[23]
See also
- History of polio
- List of polio survivors
References
- ↑ Jonas, Gerald (18 March 2008). "Arthur C. Clarke, Premier Science Fiction Writer, Dies at 90.". New York Times. https://www.nytimes.com/2008/03/18/books/18cnd-clarke.html.
- ↑ 2.0 2.1 "Post-polio syndrome: Symptoms". MayoClinic.com. http://www.mayoclinic.com/health/post-polio-syndrome/DS00494/DSECTION=symptoms.
- ↑ 3.0 3.1 3.2 "Post-Polio Syndrome Fact Sheet: National Institute of Neurological Disorders and Stroke (NINDS)". http://www.ninds.nih.gov/disorders/post_polio/detail_post_polio.htm.
- ↑ 4.0 4.1 4.2 "Characteristics and management of postpolio syndrome". JAMA 284 (4): 412–14. July 2000. doi:10.1001/jama.284.4.412. PMID 10904484. http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=10904484.
- ↑ 5.0 5.1 Howard RS (June 2005). "Poliomyelitis and the postpolio syndrome". BMJ 330 (7503): 1314–18. doi:10.1136/bmj.330.7503.1314. PMID 15933355.
- ↑ 6.0 6.1 6.2 6.3 Khan F (August 2004). "Rehabilitation for postpolio sequelae". Aust Fam Physician 33 (8): 621–24. PMID 15373379. http://www.racgp.org.au/afp/200408/20040803khan.pdf. Retrieved 24 December 2008.
- ↑ Dalakas, MC; Elder, G; Hallett, M; Ravits, J; Baker, M; Papadopoulos, N; Albrecht, P; Sever, J (10 April 1986). "A long-term follow-up study of patients with post-poliomyelitis neuromuscular symptoms.". The New England Journal of Medicine 314 (15): 959–63. doi:10.1056/NEJM198604103141505. PMID 3007983.
- ↑ "Post-polio syndrome: Causes". MayoClinic.com. http://www.mayoclinic.com/health/post-polio-syndrome/DS00494/DSECTION=causes.
- ↑ 9.0 9.1 "The course of functional status and muscle strength in patients with late-onset sequelae of poliomyelitis: a systematic review". Arch Phys Med Rehabil 86 (8): 1693–701. August 2005. doi:10.1016/j.apmr.2004.12.022. PMID 16084828.
- ↑ "Post-polio syndrome: Tests and diagnosis". MayoClinic.com. http://www.mayoclinic.com/health/post-polio-syndrome/DS00494/DSECTION=tests-and-diagnosis.
- ↑ 11.0 11.1 Postpolio Syndrome. Philadelphia: Hanley & Belfus. 2003. ISBN 978-1-56053-606-2. https://archive.org/details/postpoliosyndrom0000unse.[page needed]
- ↑ 12.0 12.1 Koopman, Fieke Sophia; Beelen, Anita; Gilhus, Nils Erik; de Visser, Marianne; Nollet, Frans (2015-05-18). "Treatment for postpolio syndrome". The Cochrane Database of Systematic Reviews (5): CD007818. doi:10.1002/14651858.CD007818.pub3. ISSN 1469-493X. PMID 25984923.
- ↑ Farbu E (2010). "Update on current and emerging treatment options for post-polio syndrome". Ther Clin Risk Manag 6: 307–13. doi:10.2147/TCRM.S4440. PMID 20668713.
- ↑ "Chronic pain secondary to disability: a review". Clin J Pain 19 (1): 3–17. 2003. doi:10.1097/00002508-200301000-00002. PMID 12514452.
- ↑ "Evaluation, treatment, and follow-up results of post polio patients with dysphagia". Otolaryngol Head Neck Surg 104 (3): 333–38. March 1991. doi:10.1177/019459989110400308. PMID 1902934.
- ↑ Lindsay, Kenneth W; Ian Bone; Robin Callander; J. van Gijn (1991). Neurology and Neurosurgery Illustrated. United States: Churchill Livingstone. pp. 489–90. ISBN 978-0-443-04345-1.
- ↑ Lambert, David A; Giannouli, Eleni; Schmidt, Brian J (2005). "Postpolio Syndrome and Anesthesia". Anesthesiology 103 (3): 638–44. doi:10.1097/00000542-200509000-00029. PMID 16129991.
- ↑ Jubelt, B; J Drucket (1999). Poliomyelitis and the Post-Polio Syndrome in Motor Disorders. Philadelphia: Lippincott Williams and Wilkins. p. 381.
- ↑ Takemura, J; Saeki, S; Hachisuka, K; Aritome, K (2004). "Prevalence of post-polio syndrome based on a cross-sectional survey in Kitakyushu, Japan". Journal of Rehabilitation Medicine 36 (1): 1–3. doi:10.1080/16501970310017423. PMID 15074431.
- ↑ 20.0 20.1 Jubelt, B; Cashman, N. R (1987). "Neurological manifestations of the post-polio syndrome". Critical Reviews in Neurobiology 3 (3): 199–220. PMID 3315237.
- ↑ 21.0 21.1 21.2 Ramlow, J; Alexander, M; Laporte, R; Kaufmann, C; Kuller, L (1992). "Epidemiology of the Post-Polio Syndrome". American Journal of Epidemiology 136 (7): 769–86. doi:10.1093/aje/136.7.769. PMID 1442743.
- ↑ Atkinson W, Hamborsky J, McIntyre L, Wolfe S (eds.) (2012). "11. Poliomyelitis". Epidemiology and Prevention of Vaccine-Preventable Diseases (The Pink Book) (12th ed.). Washington DC: Public Health Foundation. https://www.cdc.gov/vaccines/pubs/pinkbook/polio.html#post.
- ↑ Bruno, Richard L (2000). "Paralytic vs. "Nonparalytic" Polio". American Journal of Physical Medicine & Rehabilitation 79 (1): 4–12. doi:10.1097/00002060-200001000-00003. PMID 10678596.
Further reading
- Bruno, Richard L. (2002). The Polio Paradox. New York: Warner Books. ISBN 978-0-446-52907-5.
- Maynard, F.M., & Headley, J.H. (Eds.) (1999). Handbook on the Late Effects of Poliomyelitis for Physicians and Survivors. Saint Louis, MO: GINI (now Post-Polio Health International). Information on 90 post-polio topics; a compilation of the research and experience of over 40 experts.
- March of Dimes Birth Defects Foundation. (1999). Identifying Best Practices in Diagnosis & Care. Warm Springs, GA: March of Dimes International Conference on Post-Polio Syndrome
- Nollet F. "Perceived health and physical functioning in postpoliomyelitis syndrome". Vrije Universiteit Amsterdam, 2002.
- Nollet, F. "Post-polio syndrome". Orphanet Ecyclopaedia, 2003
- Silver, Julie K. (2001). Post-Polio Syndrome: A Guide for Polio Survivors and Their Families. New Haven: Yale University Press. (Dr. Silver is medical director, Spaulding-Framingham Outpatient Center; Assistant Professor, Department of Physical Medicine and Rehabilitation, Harvard Medical School.)
External links
| Classification | |
|---|---|
| External resources |
 |

