Medicine:Rhinitis
| Rhinitis | |
|---|---|
| Other names | Coryza |
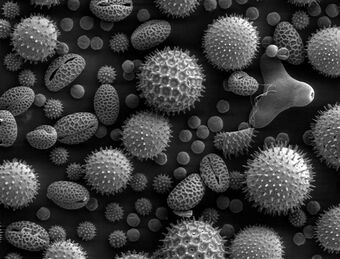 | |
| Pollen grains from a variety of common plants can cause hay fever. | |
| Pronunciation |
|
| Specialty | Infectious disease, allergy and immunology |
Rhinitis, also known as coryza,[3] is irritation and inflammation of the mucous membrane inside the nose. Common symptoms are a stuffy nose, runny nose, sneezing, and post-nasal drip.[4]
The inflammation is caused by viruses, bacteria, irritants or allergens. The most common kind of rhinitis is allergic rhinitis,[5] which is usually triggered by airborne allergens such as pollen and dander.[6] Allergic rhinitis may cause additional symptoms, such as sneezing and nasal itching, coughing, headache,[7] fatigue, malaise, and cognitive impairment.[8][9] The allergens may also affect the eyes, causing watery, reddened, or itchy eyes and puffiness around the eyes.[7] The inflammation results in the generation of large amounts of mucus, commonly producing a runny nose, as well as a stuffy nose and post-nasal drip. In the case of allergic rhinitis, the inflammation is caused by the degranulation of mast cells in the nose. When mast cells degranulate, they release histamine and other chemicals,[10] starting an inflammatory process that can cause symptoms outside the nose, such as fatigue and malaise.[11] In the case of infectious rhinitis, it may occasionally lead to pneumonia, either viral or bacterial. Sneezing also occurs in infectious rhinitis to expel bacteria and viruses from the respiratory tract.
Rhinitis is very common. Allergic rhinitis is more common in some countries than others; in the United States, about 10–30% of adults are affected annually.[12] Mixed rhinitis (MR) refers to patients with nonallergic rhinitis and allergic rhinitis. MR is a specific rhinitis subtype. It may represent between 50 and 70% of all AR patients. However, true prevalence of MR has not been confirmed yet.[13]
Types
Rhinitis is categorized into three types (although infectious rhinitis is typically regarded as a separate clinical entity due to its transient nature): (i) infectious rhinitis includes acute and chronic bacterial infections; (ii) nonallergic rhinitis[14] includes vasomotor, idiopathic, hormonal, atrophic, occupational, and gustatory rhinitis, as well as rhinitis medicamentosa (rebound congestion); (iii) allergic rhinitis, triggered by pollen, mold, animal dander, dust, Balsam of Peru, and other inhaled allergens.[15]
Infectious
Rhinitis is commonly caused by a viral or bacterial infection, including the common cold, which is caused by Rhinoviruses, Coronaviruses, and influenza viruses, others caused by adenoviruses, human parainfluenza viruses, human respiratory syncytial virus, enteroviruses other than rhinoviruses, metapneumovirus, and measles virus, or bacterial sinusitis, which is commonly caused by Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Symptoms of the common cold include rhinorrhea, sneezing, sore throat (pharyngitis), cough, congestion, and slight headache.[16][citation needed]
Nonallergic rhinitis
Nonallergic rhinitis refers to rhinitis that is not due to an allergy. The category was formerly referred to as vasomotor rhinitis, as the first cause discovered was vasodilation due to an overactive parasympathetic nerve response. As additional causes were identified, additional types of nonallergic rhinitis were recognized. Vasomotor rhinitis is now included among these under the more general classification of nonallergic rhinitis.[17] The diagnosis is made upon excluding allergic causes.[18] It is an umbrella term of rhinitis of multiple causes, such as occupational (chemical), smoking, gustatory, hormonal, senile (rhinitis of the elderly), atrophic, medication-induced (including rhinitis medicamentosa), local allergic rhinitis, non-allergic rhinitis with eosinophilia syndrome (NARES) and idiopathic (vasomotor or non-allergic, non-infectious perennial allergic rhinitis (NANIPER), or non-infectious non-allergic rhinitis (NINAR).[19]
In vasomotor rhinitis,[20][21] certain nonspecific stimuli, including changes in environment (temperature, humidity, barometric pressure, or weather), airborne irritants (odors, fumes), dietary factors (spicy food, alcohol), sexual arousal, exercise,[22] and emotional factors trigger rhinitis.[23] There is still much to be learned about this, but it is thought that these non-allergic triggers cause dilation of the blood vessels in the lining of the nose, which results in swelling and drainage.
Non-allergic rhinitis can co-exist with allergic rhinitis, and is referred to as "mixed rhinitis".[24] The pathology of vasomotor rhinitis appears to involve neurogenic inflammation[25] and is as yet not very well understood. The role of transient receptor potential ion channels on the non-neuronal nasal epithelial cells has also been suggested. Overexpression of these receptors have influence the nasal airway hyper-responsiveness to non-allergic irritant environmental stimuli (e.g., extremes of temperature, changes in osmotic or barometric pressure).[26] Vasomotor rhinitis appears to be significantly more common in women than men, leading some researchers to believe that hormone imbalance plays a role.[27][28] In general, age of onset occurs after 20 years of age, in contrast to allergic rhinitis which can be developed at any age. Individuals with vasomotor rhinitis typically experience symptoms year-round, though symptoms may be exacerbated in the spring and autumn when rapid weather changes are more common.[17] An estimated 17 million United States citizens have vasomotor rhinitis.[17]
Drinking alcohol may cause rhinitis as well as worsen asthma (see alcohol-induced respiratory reactions). In certain populations, particularly those of East Asian countries such as Japan, these reactions have a nonallergic basis.[29] In other populations, particularly those of European descent, a genetic variant in the gene that metabolizes ethanol to acetaldehyde, ADH1B, is associated with alcohol-induced rhinitis. It is suggested that this variant metabolizes ethanol to acetaldehyde too quickly for further processing by ALDH2 and thereby leads to the accumulation of acetaldehyde and rhinitis symptoms.[30] In these cases, alcohol-induced rhinitis may be of the mixed rhinitis type and, it seems likely, most cases of alcohol-induced rhinitis in non-Asian populations reflect true allergic response to the non-ethanol and/or contaminants in alcoholic beverages, particularly when these beverages are wines or beers.[29] Alcohol-exacerbated rhinitis is more frequent in individuals with a history of rhinitis exacerbated by aspirin.[31]
Aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs), particularly those that inhibit cyclooxygenase 1 (COX1), can worsen rhinitis and asthma symptoms in individuals with a history of either one of these diseases.[32] These exacerbations most often appear due to NSAID hypersensitivity reactions rather than NSAID-induced allergic reactions.[33]
The antihistamine azelastine, applied as a nasal spray, may be effective for vasomotor rhinitis.[34] Fluticasone propionate or budesonide (both are steroids) in nostril spray form may also be used for symptomatic treatment. The antihistamine cyproheptadine is also effective, probably due to its antiserotonergic effects.
A systematic review on non-allergic rhinitis reports improvement of overall function after treatment with capsaicin (the active component of chili peppers). The quality of evidence is low, however.[35]
Allergic
Allergic rhinitis or hay fever may follow when an allergen such as pollen, dust, or Balsam of Peru[36] is inhaled by an individual with a sensitized immune system, triggering antibody production. These antibodies mostly bind to mast cells, which contain histamine. When the mast cells are stimulated by an allergen, histamine (and other chemicals) are released. This causes itching, swelling, and mucus production.
Symptoms vary in severity between individuals. Very sensitive individuals can experience hives or other rashes. Particulate matter in polluted air and chemicals such as chlorine and detergents, which can normally be tolerated, can greatly aggravate the condition.[citation needed]
Characteristic physical findings in individuals who have allergic rhinitis include conjunctival swelling and erythema, eyelid swelling, lower eyelid venous stasis, lateral crease on the nose, swollen nasal turbinates, and middle ear effusion.[37]
Even if a person has negative skin-prick, intradermal and blood tests for allergies, they may still have allergic rhinitis, from a local allergy in the nose. This is called local allergic rhinitis.[38] Many people who were previously diagnosed with nonallergic rhinitis may actually have local allergic rhinitis.[39]
A patch test may be used to determine if a particular substance is causing the rhinitis.
Rhinitis medicamentosa
Rhinitis medicamentosa is a form of drug-induced nonallergic rhinitis which is associated with nasal congestion brought on by the use of certain oral medications (primarily sympathomimetic amine and 2-imidazoline derivatives) and topical decongestants (e.g., oxymetazoline, phenylephrine, xylometazoline, and naphazoline nasal sprays) that constrict the blood vessels in the lining of the nose.[40]
Chronic atrophic rhinitis
Chronic rhinitis is a form of atrophy of the mucous membrane and glands of the nose.
Rhinitis sicca
Chronic form of dryness of the mucous membranes.
Polypous rhinitis
Chronic rhinitis associated with polyps in the nasal cavity.
Pathophysiology
File:Neural abnormalities.tif File:Non-allergic rhinitis mechanism.tif Most prominent pathological changes observed are nasal airway epithelial metaplasia in which goblet cells replace ciliated columnar epithelial cells in the nasal mucous membrane.[26] This results in mucin hypersecretion by goblet cells and decreased mucociliary activity. Nasal secretion are not adequately cleared with clinical manifestation of nasal congestion, sinus pressure, post-nasal dripping, and headache. Over-expression of transient receptor potential (TRP) ion channels, such as TRPA1 and TRPV1, may be involved in the pathogenesis of non-allergic rhinitis.[41]
Association between rhinitis and asthma
Neurogenic inflammation produced by neuropeptides released from sensory nerve endings to the airways is a proposed common mechanism of association between both allergic and non-allergic rhinitis with asthma. This may explain higher association of rhinitis with asthma developing later in life.[42] Environmental irritants acts as modulators of airway inflammation in these contiguous airways. Development of occupational asthma is often preceded by occupational rhinitis. Among the causative agents are flours, enzymes used in processing food, latex, isocyanates, welding fumes, epoxy resins, and formaldehyde. Accordingly, prognosis of occupational asthma is contingent on early diagnosis and the adoption of protective measures for rhinitis.[43]
Diagnosis
The different forms of rhinitis are essentially diagnosed clinically.[clarification needed] Vasomotor rhinitis is differentiated from viral and bacterial infections by the lack of purulent exudate and crusting. It can be differentiated from allergic rhinitis because of the absence of an identifiable allergen.[44]
Evidence has been published from a few health apps for mobile devices that show potential to assist in the diagnosis of rhinitis and rhinosinusitis and to evaluate management and treatment adherence. While this shows promise for clinical management, (As of 2022) few had been validated in the scientific literature, and even fewer included considerations for multimorbidity.[45][46]
Prevention
In the case of infectious rhinitis, vaccination against influenza viruses, COVID-19 virus, adenoviruses, measles, rubella, Streptococcus pneumoniae, Haemophilus influenzae, diphtheria, Bacillus anthracis, and Bordetella pertussis may help prevent it.[citation needed]
Management
The management of rhinitis depends on the underlying cause.
For allergic rhinitis, intranasal corticosteroids are recommended.[47] For severe symptoms intranasal antihistamines may be added.[47]
Pronunciation and etymology
Rhinitis is pronounced /raɪˈnaɪtɪs/,[48] while coryza is pronounced /kəˈraɪzə/.[49]
Rhinitis comes from the Ancient Greek ῥίς rhis, gen.: ῥινός rhinos "nose". Coryza has a dubious etymology. Robert Beekes rejected an Indo-European derivation and suggested a Pre-Greek reconstruction *karutya.[50] According to physician Andrew Wylie, "we use the term [coryza] for a cold in the head, but the two are really synonymous. The ancient Romans advised their patients to clean their nostrils and thereby sharpen their wits."[51]
References
- ↑ "rhinitis | Definition, meaning & more | Collins Dictionary". www.collinsdictionary.com. https://www.collinsdictionary.com/dictionary/english/rhinitis.
- ↑ "coryza | Definition, meaning & more | Collins Dictionary". www.collinsdictionary.com. https://www.collinsdictionary.com/dictionary/english/coryza.
- ↑ Pfaltz, Carl Rudolf; Becker, Walter; Naumann, Hans Heinz (2009). Ear, nose, and throat diseases: with head and neck surgery (3rd ed.). Stuttgart: Thieme. p. 150. ISBN 978-3-13-671203-0. https://books.google.com/books?id=HlrHjWQsRGEC&pg=PA150.
- ↑ "Nonallergic rhinitis". http://www.mayoclinic.com/health/nonallergic-rhinitis/DS00809/DSECTION=symptoms.
- ↑ "Rhinitis: a dose of epidemiological reality". Allergy Asthma Proc 24 (3): 147–54. 2003. PMID 12866316.
- ↑ Sullivan, John B.; Krieger, Gary R. (2001). Clinical environmental health and toxic exposures. p. 341.
- ↑ 7.0 7.1 "Allergic rhinitis". http://www.umm.edu/altmed/articles/allergic-rhinitis-000003.htm.
- ↑ "Diagnosing rhinitis: allergic vs. nonallergic". American Family Physician 73 (9): 1583–90. May 2006. PMID 16719251.
- ↑ "Effects of seasonal allergic rhinitis on selected cognitive abilities". Annals of Allergy, Asthma & Immunology 84 (4): 403–10. April 2000. doi:10.1016/S1081-1206(10)62273-9. PMID 10795648.
- ↑ "Inflammatory Nature of Allergic Rhinitis: Pathophysiology". http://www.medscape.org/viewarticle/532192_2.
- ↑ "Immunopathogenesis of allergic rhinitis". http://www.espai-eg.org/Journal/8-1/Deraz.pdf.
- ↑ "Economic Impact and Quality-of-Life Burden of Allergic Rhinitis: Prevalence". http://www.medscape.com/viewarticle/472667_2.
- ↑ Bernstein, Jonathan A. (September 2010). "Allergic and mixed rhinitis: Epidemiology and natural history". Allergy and Asthma Proceedings 31 (5): 365–369. doi:10.2500/aap.2010.31.3380. ISSN 1539-6304. PMID 20929601.
- ↑ Kaliner, Michael A (2009-06-15). "Classification of Nonallergic Rhinitis Syndromes With a Focus on Vasomotor Rhinitis, Proposed to be Known henceforth as Nonallergic Rhinopathy". The World Allergy Organization Journal 2 (6): 98–101. doi:10.1097/WOX.0b013e3181a9d55b. ISSN 1939-4551. PMID 24229372.
- ↑ "Allergic rhinitis". 2018-12-26. http://emedicine.medscape.com/article/134825-overview.
- ↑ "Common cold symptoms in children: results of an Internet-based surveillance program". Journal of Medical Internet Research 16 (6): e144. June 2014. doi:10.2196/jmir.2868. PMID 24945090.
- ↑ 17.0 17.1 17.2 "Vasomotor rhinitis". American Family Physician 72 (6): 1057–62. September 2005. PMID 16190503.
- ↑ "Clinically relevant outcome measures of novel pharmacotherapy for nonallergic rhinitis". Current Opinion in Allergy and Clinical Immunology 15 (3): 204–12. June 2015. doi:10.1097/ACI.0000000000000166. PMID 25899692.
- ↑ "Up-date on neuro-immune mechanisms involved in allergic and non-allergic rhinitis". Rhinology 50 (3): 227–35. September 2012. doi:10.4193/Rhino11.152. PMID 22888478.
- ↑ Wheeler, P. W.; Wheeler, S. F. (Sep 2005). "Vasomotor rhinitis". Am Fam Physician 72 (6): 1057–62. PMID 16190503. http://www.aafp.org/afp/2005/0915/p1057.html.
- ↑ "Vasomotor rhinitis Medline Plus". Nlm.nih.gov. https://www.nlm.nih.gov/medlineplus/ency/article/001648.htm.
- ↑ "Exercise-induced rhinitis: a common disorder that adversely affects allergic and nonallergic athletes". Annals of Allergy, Asthma & Immunology 96 (2): 334–40. February 2006. doi:10.1016/s1081-1206(10)61244-6. PMID 16498856.
- ↑ Adelman, Daniel (2002). Manual of Allergy and Immunology: Diagnosis and Therapy. Lippincott Williams & Wilkins. p. 66. ISBN 9780781730525.
- ↑ (Middleton's Allergy Principles and Practice, seventh edition.)
- ↑ "[Ultrastructural changes in allergic rhinitis vs. idiopathic rhinitis]". Hno 56 (8): 799–807. August 2008. doi:10.1007/s00106-008-1764-4. PMID 18651116.
- ↑ 26.0 26.1 26.2 26.3 "Neural Abnormalities in Nonallergic Rhinitis". Current Allergy and Asthma Reports 15 (4): 18. April 2015. doi:10.1007/s11882-015-0511-7. PMID 26130469.
- ↑ "What causes non-allergic rhinitis?". Gov.uk. 2018-09-07. https://www.nhs.uk/conditions/non-allergic-rhinitis/.
- ↑ "Non-allergic rhinitis: Position paper of the European Academy of Allergy and Clinical Immunology". Allergy 72 (11): 1657–1665. November 2017. doi:10.1111/all.13200. PMID 28474799.
- ↑ 29.0 29.1 "Adverse reactions to alcohol and alcoholic beverages". Annals of Allergy, Asthma & Immunology 111 (6): 439–45. December 2013. doi:10.1016/j.anai.2013.09.016. PMID 24267355.
- ↑ "Associations of ADH and ALDH2 gene variation with self report alcohol reactions, consumption and dependence: an integrated analysis". Human Molecular Genetics 18 (3): 580–93. February 2009. doi:10.1093/hmg/ddn372. PMID 18996923.
- ↑ "Alcohol-induced respiratory symptoms are common in patients with aspirin exacerbated respiratory disease". The Journal of Allergy and Clinical Immunology. In Practice 2 (2): 208–13. 2014. doi:10.1016/j.jaip.2013.12.003. PMID 24607050.
- ↑ "Prevalence of aspirin-exacerbated respiratory disease among asthmatic patients: A meta-analysis of the literature". The Journal of Allergy and Clinical Immunology 135 (3): 676–81.e1. March 2015. doi:10.1016/j.jaci.2014.08.020. PMID 25282015.
- ↑ "An update on the pathogenesis of the upper airways in aspirin-exacerbated respiratory disease". Current Opinion in Allergy and Clinical Immunology 14 (1): 1–6. February 2014. doi:10.1097/aci.0000000000000021. PMID 24300420.
- ↑ "Azelastine hydrochloride: a review of pharmacology, pharmacokinetics, clinical efficacy and tolerability". Current Medical Research and Opinion 23 (10): 2441–52. October 2007. doi:10.1185/030079907X226302. PMID 17723160.
- ↑ "Capsaicin for non-allergic rhinitis". The Cochrane Database of Systematic Reviews 2015 (7): CD010591. July 2015. doi:10.1002/14651858.CD010591.pub2. PMID 26171907.
- ↑ Brooks, Pamela (2012-10-25). The Daily Telegraph: Complete Guide to Allergies. Little, Brown Book. ISBN 9781472103949. https://books.google.com/books?id=eReGG6UtxbcC&q=%22balsam+of+peru%22+allergy&pg=PT413. Retrieved 2014-04-23.[yes|permanent dead link|dead link}}]
- ↑ "Allergic rhinitis: update on diagnosis". Consultant 49: 610–613. 2009. http://www.consultantlive.com/display/article/10162/1465701. Retrieved 2010-02-22.
- ↑ "Local allergic rhinitis: a new entity, characterization and further studies". Current Opinion in Allergy and Clinical Immunology 10 (1): 1–7. February 2010. doi:10.1097/ACI.0b013e328334f5fb. PMID 20010094.
- ↑ "Local allergic rhinitis: concept, clinical manifestations, and diagnostic approach". Journal of Investigational Allergology & Clinical Immunology 20 (5): 364–71; quiz 2 p following 371. 2010. PMID 20945601.
- ↑ "Rhinitis medicamentosa". Journal of Investigational Allergology & Clinical Immunology 16 (3): 148–55. 2006. PMID 16784007. http://www.jiaci.org/issues/vol16issue03/1.pdf.
- ↑ "TRP channels and temperature in airway disease-clinical significance". Temperature 2 (2): 172–7. April 2015. doi:10.1080/23328940.2015.1012979. PMID 27227021.
- ↑ "Rhinitis phenotypes correlate with different symptom presentation and risk factor patterns of asthma". Respiratory Medicine 105 (11): 1611–21. November 2011. doi:10.1016/j.rmed.2011.06.004. PMID 21764573.
- ↑ "[Occupational rhinitis and asthma]". Therapeutische Umschau 69 (4): 261–7. April 2012. doi:10.1024/0040-5930/a000283. PMID 22477666.
- ↑ "Nonallergic Rhinitis - Ear, Nose, and Throat Disorders" (in en-PT). https://www.msdmanuals.com/en-pt/professional/ear,-nose,-and-throat-disorders/nose-and-paranasal-sinus-disorders/nonallergic-rhinitis?query=rhinitis.
- ↑ Sousa-Pinto, Bernardo; Anto, Aram; Berger, Markus; Dramburg, Stephanie; Pfaar, Oliver et al. (2022). "Real-world data using mHealth apps in rhinitis, rhinosinusitis and their multimorbidities". Clinical and Translational Allergy (Wiley) 12 (11): e12208. doi:10.1002/clt2.12208. ISSN 2045-7022. PMID 36434742.
- ↑ May, Brandon (6 December 2022). "Study Finds 7 Apps for Rhinitis and Rhinosinusitis With Evidence". https://www.medscape.com/viewarticle/985131.
- ↑ 47.0 47.1 "Pharmacologic Treatment of Seasonal Allergic Rhinitis: Synopsis of Guidance From the 2017 Joint Task Force on Practice Parameters". Annals of Internal Medicine 167 (12): 876–881. December 2017. doi:10.7326/M17-2203. PMID 29181536.
- ↑ "rhinitis | Definition, meaning & more | Collins Dictionary". www.collinsdictionary.com. https://www.collinsdictionary.com/dictionary/english/rhinitis.
- ↑ "coryza | Definition, meaning & more | Collins Dictionary". www.collinsdictionary.com. https://www.collinsdictionary.com/dictionary/english/coryza.
- ↑ Etymological Dictionary of Greek. Brill. 2009. p. 756.
- ↑ "Rhinology and laryngology in literature and Folk-Lore.". The Journal of Laryngology & Otology 42 (2): 81–87. 1927. doi:10.1017/S0022215100029959.
| Classification | |
|---|---|
| External resources |
 |

