Chemistry:Estradiol valerate
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌɛstrəˈdaɪoʊl ˈvæləreɪt/ ES-trə-DY-ohl VAL-ə-rayt[1] |
| Trade names | Delestrogen, Progynon Depot, Progynova, many others |
| Other names | EV; E2V; Oestradiol valerate; Estradiol pentanoate; Estradiol valerianate |
| Routes of administration | By mouth, sublingual, intramuscular injection,[2] subcutaneous injection |
| Drug class | Estrogen; Estrogen ester |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Oral: 3–5%[3][4] IM injection: 100%[5][3] |
| Metabolism | Cleavage via esterases in the liver, blood, and tissues[3] |
| Metabolites | Estradiol, valeric acid, and metabolites of estradiol[3] |
| Elimination half-life | Oral: 12–20 hours (as E2)[3][6] IM injection: 3.5 (1.2–7.2) days[7] |
| Duration of action | IM injection: • 5 mg: 7–8 days[8] • 10 mg: 10–14 days[9][10] • 40 mg: 2–3 weeks[9] • 100 mg: 3–4 weeks[9] |
| Excretion | Urine (80%)[3] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C23H32O3 |
| Molar mass | 356.506 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 144 to 145 °C (291 to 293 °F) |
| |
| |
Estradiol valerate (EV), sold for use by mouth under the brand name Progynova and for use by injection under the brand names Delestrogen and Progynon Depot among others, is an estrogen medication. It is used in hormone therapy for menopausal symptoms and low estrogen levels, hormone therapy for transgender people, and in hormonal birth control.[4][3][11][12] It is also used in the treatment of prostate cancer.[11] The medication is taken by mouth or by injection into muscle or fat once every 1 to 4 weeks.[11][12]

Side effects of estradiol valerate include breast tenderness, breast enlargement, nausea, headache, and fluid retention.[13][11][12] Estradiol valerate is an estrogen and hence is an agonist of the estrogen receptor, the biological target of estrogens like estradiol.[4][3][14] It is an estrogen ester and a prodrug of estradiol in the body.[14][4][3] Because of this, it is considered to be a natural and bioidentical form of estrogen.[14][15][3][16]
Estradiol valerate was first described in 1940 and was introduced for medical use in 1954.[17][18][19] Along with estradiol cypionate, it is one of the most widely used esters of estradiol.[20] Estradiol valerate is used in the United States , Canada , Europe, and throughout much of the rest of the world.[21][22] It is available as a generic medication.[23]
Medical uses
The medical uses of estradiol valerate are the same as those of estradiol and other estrogens. Examples of indications for the medication include hormone therapy and hormonal contraception. In regard to the latter, estradiol valerate is available in combination with a progestin as a combined estradiol-containing oral contraceptive (with dienogest)[24] and as a combined injectable contraceptive.[25][26] Along with estradiol cypionate, estradiol undecylate, and estradiol benzoate, estradiol valerate is used as a form of high-dose estrogen therapy in feminizing hormone therapy for transgender women.[27][28][29][30] It is also used as a form of high-dose estrogen therapy in the treatment of prostate cancer in men.[11] Low-dose oral estradiol valerate (2–6 mg/day) has been used in the treatment of breast cancer in women who were previously treated with and benefited from but acquired resistance to aromatase inhibitors as well.[31][32] Injectable estradiol valerate has been used to suppress sex drive in sex offenders.[33]
In the United States , the approved indications of estradiol valerate injections include the treatment of moderate to severe hot flashes and vaginal atrophy associated with menopause in women, the treatment of hypoestrogenism due to hypogonadism, castration, or primary ovarian failure in women, and the palliative treatment of advanced prostate cancer in men.[11] Elsewhere in the world, oral estradiol valerate is similarly approved for the treatment of symptoms associated with menopause or hypoestrogenism due to castration in women.[12] Such symptoms may include hot flashes, outbreaks of sweat, sleep disturbances, depressive moods, irritability, headaches, and dizziness.[12]
Estradiol valerate by intramuscular injection is usually used at a dosage of 10 to 20 mg every 4 weeks in the treatment of menopausal symptoms and hypoestrogenism due to hypogonadism, castration, or primary ovarian failure in women.[11] In the past, it was used at even higher doses of 10 to 40 every 1 to 4 weeks for estrogen replacement.[34] Estradiol valerate is usually used in the treatment of advanced prostate cancer in men at a dosage of 30 mg or more every 1 to 2 weeks by intramuscular injection.[11] In transgender women, estradiol valerate given by intramuscular injection is usually used at a dosage of 5 to 20 mg, but up to 30 to 40 mg, once every 2 weeks.[28][29][27] Estradiol valerate has also been used at a dose of 10 to 40 mg by intramuscular injection to limit bleeding in women with hemorrhage due to dysfunctional uterine bleeding.[35]: 318 [36]: 60
Available forms
Estradiol valerate is and has been available in the form of vials and ampoules of oil solution for intramuscular injection in concentrations of 4, 5, 10, 20, and 40 mg/mL and in the form of oral tablets at doses of 0.5, 1, 2, and 4 mg per tablet.[37][17][38][39] In the United States , it is specifically available in formulations of 10, 20, and 40 mg/mL in oil solution (as Delestrogen, as well as generics).[37] Aside from estradiol valerate, the only other injectable estrogen formulations that remain available in the United States are estradiol cypionate (5 mg/mL in oil solution) and conjugated estrogens (25 mg/vial in solution).[37] Some or all oral estradiol valerate tablets are micronized, similarly to oral estradiol tablets.[40]
In addition to single-drug formulations, oral estradiol valerate is available in combination with the progestin dienogest as a combined oral contraceptive and intramuscular estradiol valerate is marketed at a concentration of 5 mg/mL in combination with the progestin hydroxyprogesterone caproate and with the progestin norethisterone enantate as combined injectable contraceptives.[37][24][25][26][1] Intramuscular estradiol valerate is also marketed at a concentration of 4 mg/mL in combination with the weak androgen and neurosteroid prasterone enanthate (DHEA enanthate) and with the androgen testosterone enantate for use in menopausal hormone therapy, but the latter formulation has been discontinued.[41][37] The availability of estradiol valerate-containing products varies throughout the world.[1]
Contraindications
Contraindications of estrogens include coagulation problems, cardiovascular diseases, liver disease, and certain hormone-sensitive cancers such as breast cancer and endometrial cancer, among others.[42][43][44][45]
Side effects
The side effects of estradiol valerate are the same as those of estradiol. Examples of such side effects include breast tenderness and enlargement, nausea, bloating, edema, headache, and melasma.[13][46] High-dose estrogen therapy with estradiol valerate injections may also cause an increased risk of thromboembolism, changes in blood lipid profile, increased insulin resistance, and increased levels of prolactin.[46]
Overdose
Estradiol valerate has been used at very high doses of 40 to 100 mg once per week in women and men, without overt signs of acute toxicity observed.[47][48][49][50][51][52][53][54][55][56][57] Symptoms of estrogen overdosage may include nausea, vomiting, bloating, increased weight, water retention, breast tenderness, vaginal discharge, heavy legs, and leg cramps.[42] These side effects can be diminished by reducing the estrogen dosage.[42]
Interactions
Inhibitors and inducers of cytochrome P450 may influence the metabolism of estradiol and by extension circulating estradiol levels.[58]
Pharmacology
Pharmacodynamics
Estradiol valerate is an estradiol ester, or a prodrug of estradiol.[14][4] As such, it is an estrogen, or an agonist of the estrogen receptors.[4][14] The affinity of estradiol valerate for the estrogen receptor is approximately 50 times lower than that of estradiol.[3] In addition, estradiol valerate is rapidly cleaved into estradiol and is unable to reach target tissues in concentrations of significance, if at all.[3] As such, estradiol valerate is essentially inactive in terms of estrogenic effect itself, acting solely as a prodrug to estradiol.[3] The molecular weight of estradiol valerate is about 131% of that of estradiol due to the presence of its C17β valerate ester, and hence estradiol valerate contains about 76% of the amount of estradiol of an equal dose of estradiol.[21][22] Aside from dose adjustment to account for the difference in molecular weight, oral estradiol valerate is considered to be equivalent to oral estradiol.[3] Because estradiol valerate is a prodrug of estradiol, it is considered to be a natural and bioidentical form of estrogen.[14][15][16]
| Estrogen | Form | Major brand names | EPD | CIC-D | Duration | |
|---|---|---|---|---|---|---|
| Estradiol | Oil solution | – | 40–60 mg | – | 1–2 mg ≈ 1–2 days | |
| Aqueous suspension | Aquadiol, Diogyn, Progynon, Mego-E | ? | 3.5 mg | 0.5–2 mg ≈ 2–7 days; 3.5 mg ≈ >5 days | ||
| Microspheres | Juvenum-E, Juvenum | ? | – | 1 mg ≈ 30 days | ||
| Estradiol benzoate | Oil solution | Progynon-B | 25–35 mg | – | 1.66 mg ≈ 2–3 days; 5 mg ≈ 3–6 days | |
| Aqueous suspension | Agofollin-Depot, Ovocyclin M | 20 mg | – | 10 mg ≈ 16–21 days | ||
| Emulsion | Menformon-Emulsion, Di-Pro-Emulsion | ? | – | 10 mg ≈ 14–21 days | ||
| Estradiol dipropionate | Oil solution | Agofollin, Di-Ovocylin, Progynon DP | 25–30 mg | – | 5 mg ≈ 5–8 days | |
| Estradiol valerate | Oil solution | Delestrogen, Progynon Depot, Mesigyna | 20–30 mg | 5 mg | 5 mg ≈ 7–8 days; 10 mg ≈ 10–14 days; 40 mg ≈ 14–21 days; 100 mg ≈ 21–28 days | |
| Estradiol benzoate butyrate | Oil solution | Redimen, Soluna, Unijab | ? | 10 mg | 10 mg ≈ 21 days | |
| Estradiol cypionate | Oil solution | Depo-Estradiol, Depofemin | 20–30 mg | – | 5 mg ≈ 11–14 days | |
| Aqueous suspension | Cyclofem, Lunelle | ? | 5 mg | 5 mg ≈ 14–24 days | ||
| Estradiol enanthate | Oil solution | Perlutal, Topasel, Yectames | ? | 5–10 mg | 10 mg ≈ 20–30 days | |
| Estradiol dienanthate | Oil solution | Climacteron, Lactimex, Lactostat | ? | – | 7.5 mg ≈ >40 days | |
| Estradiol undecylate | Oil solution | Delestrec, Progynon Depot 100 | ? | – | 10–20 mg ≈ 40–60 days; 25–50 mg ≈ 60–120 days | |
| Polyestradiol phosphate | Aqueous solution | Estradurin | 40–60 mg | – | 40 mg ≈ 30 days; 80 mg ≈ 60 days; 160 mg ≈ 120 days | |
| Estrone | Oil solution | Estrone, Kestrin, Theelin | ? | – | 1–2 mg ≈ 2–3 days | |
| Aqueous suspension | Estrone Aq. Susp., Kestrone, Theelin Aq. | ? | – | 0.1–2 mg ≈ 2–7 days | ||
| Estriol | Oil solution | – | ? | – | 1–2 mg ≈ 1–4 days | |
| Polyestriol phosphate | Aqueous solution | Gynäsan, Klimadurin, Triodurin | ? | – | 50 mg ≈ 30 days; 80 mg ≈ 60 days | |
| Notes: All aqueous suspensions are of microcrystalline particle size. Estradiol production during the menstrual cycle is 30–640 µg/day (6.4–8.6 mg total per month or cycle). The vaginal epithelium maturation dosage of estradiol benzoate or estradiol valerate has been reported as 5 to 7 mg/week. An effective ovulation-inhibiting dose of estradiol undecylate is 20–30 mg/month. Sources: See template. | ||||||
Effects on liver protein synthesis
The influence of 2 mg/day oral estradiol valerate on coagulation factors is less than that of 10 μg/day oral ethinylestradiol.[59][24][60][61][62] Oral ethinylestradiol at 10 μg/day has been found to have about 1.5- to 2.5-fold the impact of 2 mg/day oral estradiol valerate on HDL cholesterol and triglycerides.[63][64][65] The influence of 20 or 50 μg/day oral ethinylestradiol on coagulation factors and HDL cholesterol is markedly greater than that of 2 mg/day oral estradiol valerate.[63][66]
Estradiol-containing birth control pills, which contain 1 to 3 mg/day estradiol or estradiol valerate, have been found to increase sex hormone-binding globulin (SHBG) levels by 1.5-fold.[67][68] Oral estradiol valerate at 6 mg/day has been found to increase SHBG levels by 2.5- to 3-fold in transgender women.[69][70] For comparison, combined birth control pills containing ethinylestradiol and a progestin with minimal androgenic or antiandrogenic activity have been found to increase SHBG levels by about 3- to 4-fold.[71]
Pharmacokinetics
Regardless of the route of administration, estradiol valerate behaves as a prodrug of estradiol via cleavage by esterases into estradiol and the natural fatty acid valeric acid.[4][14][3][72] This cleavage occurs not only in the liver, but also in the blood and in tissues, and the hydrolysis of estradiol valerate into estradiol and valeric acid is complete regardless of whether the medication is administered orally or parenterally.[3] High levels of circulating estradiol are found after an intravenous injection of estradiol valerate, and this indicates very rapid cleavage of the medication upon entering circulation.[3]
Oral administration
Esterification of the C17β position of estradiol as in estradiol valerate reduces the metabolism of estradiol valerate by 17β-hydroxysteroid dehydrogenase (17β-HSD).[4] As approximately 80% of estradiol is metabolized into estrone (and estrone sulfate) by 17β-HSD during first-pass metabolism, this improves the metabolic stability and hence bioavailability of estradiol valerate.[14] However, estradiol valerate is hydrolyzed into estradiol and valeric acid in the intestines, and hence, is still subject to extensive first-pass metabolism.[4] As such, the oral bioavailability of estradiol valerate is only around 3 to 5%, and is similar to that of oral estradiol.[3][4][73] All oral tablets in the cases of both estradiol and estradiol valerate seem to be micronized.[40] Due to its nature as a rapidly converted prodrug of estradiol, the pharmacokinetics of oral estradiol valerate are similar to those of oral estradiol.[3][4] Moreover, the pharmacodynamics and potency (after differences in molecular weight are taken into account) of oral estradiol valerate are considered to be equivalent to those of oral estradiol.[3] This is also notably true for effects on hepatic protein synthesis (e.g., of SHBG), again after differences in molecular weight between the two compounds are considered.[3]
A dosage of 1 mg/day oral estradiol valerate has been found to produce approximate circulating concentrations of 50 pg/mL estradiol and 160 pg/mL estrone, while a dosage of 2 mg/day results in circulating levels of 60 pg/mL estradiol and 300 pg/mL estrone.[74] These concentrations of estradiol and estrone are comparable to those observed with 1 and 2 mg/day oral estradiol.[74] A review of selected studies reported a range of mean peak estradiol levels of 24 to 140 pg/mL occurring 1 to 12 hours after administration of 2 mg oral estradiol valerate.[3] A study found that, in accordance with their differences in molecular weights, oral estradiol produced higher levels of estradiol than oral estradiol valerate.[75] Likewise, other studies found that levels of estradiol and estrone are very similar after oral administration of roughly equimolar doses of estradiol (1.5 mg) and estradiol valerate (2 mg).[76][77][78] A study of high-dose oral estradiol valerate found levels of estradiol of about 250 pg/mL after a single 10-mg dose in three women.[73]
Sublingual administration
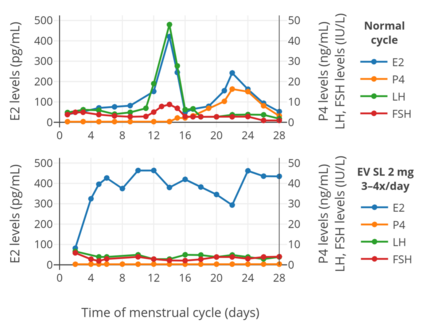
Estradiol valerate has been studied by sublingual administration in premenopausal women for the purpose of cycle control and ovulation suppression in egg donation and surrogacy.[80][81] It has been investigated for this indication, along with vaginal and transdermal estradiol, because oral estradiol valerate is sometimes unable to achieve adequate estradiol levels and hence proper cycle control in this situation.[80][81] Sublingual administration of estradiol valerate bypasses the first pass that occurs with the oral route and results in higher levels of estradiol and improved cycle control.[80][81] Sublingual estradiol valerate is also used in hormone therapy for transgender women.[82]
The administration of 2 mg oral micronized estradiol valerate tablets (Progynova, Schering) sublingually 3 or 4 times per day has been found to result in circulating estradiol levels of about 290 pg/mL to 460 pg/mL in premenopausal women (time of measurements not given).[80][81] Steady-state levels of estradiol were achieved within about 2 or 3 days.[80][81] Levels of progesterone, luteinizing hormone, and follicle-stimulating hormone were all considerably suppressed, and ovulation, as well as the associated mid-cycle hormonal surges, were prevented.[80][81] Similarly to oral administration of estradiol, but in contrast to the vaginal and transdermal routes, the ratio of estradiol to estrone is decreased with sublingual administration of either estradiol valerate or estradiol.[80][81][83]
Intramuscular injection
In contrast to oral administration, the bioavailability of estradiol valerate is complete (i.e., 100%) via intramuscular injection.[5][3][4] Due to the far greater bioavailability of intramuscular estradiol valerate relative to oral, the former is substantially stronger (in terms of potency) than the latter.[3] As an example, a single 4 mg intramuscular injection is said to be approximately equivalent to 2 mg/day of the medication administered orally over the course of 3 weeks.[3] Estradiol valerate, when given intramuscularly in oil, has a relatively long duration due to the formation of an intramuscular depot from which the medication is slowly released and absorbed.[3][84] Upon intramuscular injection of estradiol valerate in an oil solution, the solvent (i.e., oil) is absorbed, and a primary microcrystalline depot is formed within the muscle at the site of injection.[4] In addition, a secondary depot may also be formed in adipose tissue.[4] The slow release of estradiol valerate is caused by the increased lipophilicity of the medication, which in turn is due to its long fatty acid valeric acid ester moiety.[3] The elimination half-life of estradiol valerate in oil by intramuscular injection (brand names Estradiol-Depot 10 mg, Progynon Depot-10) is about 3.5 days, with a range of 1.2 days to 7.2 days in different individuals.[7] Α couple of older studies from the 1980s with sample sizes of only 2 or 3 individuals reported an elimination half-life of 4 to 5 days.[3][85][86]
A single intramuscular injection of 4 mg estradiol valerate has been found to result in maximal circulating levels of estradiol of about 390 pg/mL within 3 days of administration, with levels declining to 100 pg/mL (baseline, in the study) by 12 to 13 days.[41] Studies in general have found that a single intramuscular injection of 4 mg estradiol valerate results in peak levels of estradiol of 240 to 540 pg/mL after 1 to 5 days following administration.[86] A study found that a single intramuscular injection of 5 mg estradiol valerate resulted in peak circulating levels of 667 pg/mL estradiol and 324 pg/mL estrone within approximately 2 and 3 days, respectively.[8] The duration of estradiol valerate at this dose and in this study was considered to be 7 to 8 days.[8] Other studies have found that larger doses of intramuscular estradiol valerate exceeding 20 mg have a duration of more than 15 days.[8] A third study, in contrast to the preceding study, found that a single 10 mg intramuscular injection of estradiol valerate resulted in maximal estradiol levels of 506 to 544 pg/mL and maximal estrone levels of 205 to 219 pg/mL in postmenopausal women.[7]
With intramuscular injections of estradiol valerate, it has been reported that a dose of 5 mg has a duration of 7 to 8 days, 10 mg a duration of 10 to 14 days, 40 mg a duration of 2 to 3 weeks (14 to 21 days), and 100 mg a duration of 3 to 4 weeks (21 to 28 days).[9][10][8]
A study of pseudopregnancy with intramuscular injections of 40 mg/week estradiol valerate and 250 mg/week hydroxyprogesterone caproate in women with estrogen deficiency observed estradiol levels of about 3,100 pg/mL at 3 months of therapy and 2,500 pg/mL at 6 months of therapy.[48]
-
Estrogen levels after a single intramuscular injection of 10 mg estradiol valerate in oil in 24 postmenopausal women.[7] Determinations were made for both Progynon Depot 10 and Estradiol Depot 10, for a total of 48 measurements per point.[7] Assays were performed using GC/MS-NCI/SIM.[7] Source was Schug et al. (2012).[7]
-
Hormone levels after a single intramuscular injection of 5 mg estradiol valerate in oil in 17 postmenopausal women.[87] Assays were performed using EIA.[87] Estrone levels were likely overestimated, possibly due to cross reactivity of the assay with estrogen conjugates.[7] Source was Göretzlehner et al. (2002).[87]
-
Estradiol levels after a single intramuscular injection of 10 mg estradiol valerate or 100 mg estradiol undecylate in oil both in 4 individuals each.[89] Subject characteristics and assay method were not described.[89] Source was Vermeulen (1975).[89]
-
Estradiol and DHEA levels after a single intramuscular injection of Gynodian Depot (4 mg estradiol valerate, 200 mg prasterone enanthate in oil) or Primogyn Depot (10 mg estradiol valerate in oil) in women.[90][85][91] Assays were performed using RIA.[85][91] Sources were Düsterberg & Wendt (1983) and Rauramo et al. (1980).[90][85][91]
-
Estradiol levels after an intramuscular injection of 10 mg estradiol valerate in oil, Climacteron (150 mg testosterone enanthate, 1 mg estradiol benzoate, 7.5 mg estradiol dienanthate in oil), and control group in 20, 11, and 11 ovariectomized women, respectively.[94] Assays were performed using RIA.[94] Source was Sherwin et al. (1987).[94]
Subcutaneous injection
Estradiol esters like estradiol valerate and estradiol cypionate can be given by subcutaneous injection instead of intramuscular injection.[96][97]
Intravenous injection
The administration of estradiol valerate by intravenous injection has been studied.[3][86] It has been found to be very rapidly cleaved into estradiol.[3][86] The bioavailability and metabolism of estradiol valerate does not differ with intravenous versus intramuscular injection.[86] Conversely, intravenous injection of estradiol valerate has a very short duration, whereas intramuscular injection has a long duration and elimination half-life.[86]
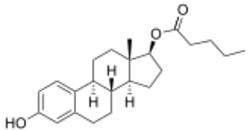
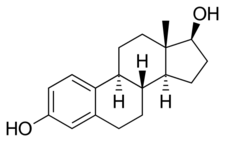
Chemistry
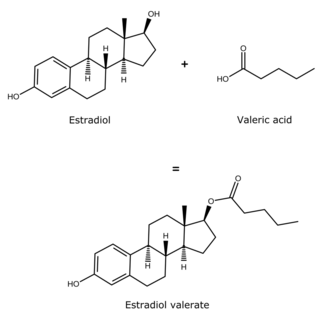
Estradiol valerate is a synthetic estrane steroid and the C17β valerate (pentanoate) fatty acid ester of estradiol.[21][22] It is also known as estradiol 17β-valerate or as estra-1,3,5(10)-triene-3,17β-diol 17β-pentanoate.[21][22] Other common esters of estradiol in use include estradiol cypionate, estradiol enantate, and estradiol acetate, the former two of which are C17β esters of estradiol similarly to estradiol valerate and the latter of which is the C3 acetate ester of estradiol.[21][22]
The experimental log octanol/water partition coefficient (log P) of estradiol valerate is 5.6.[98]
History
Estradiol valerate was patented by Ciba in 1940 and 1941, with a priority date of 1936.[17][99] It was synthesized and studied, along with a variety of other estradiol esters, by Karl Junkmann of Schering AG in 1953.[100][101] The medication was first introduced for medical use via intramuscular injection in 1954 by Schering in Europe under the brand name Progynon Depot and by Squibb in the United States under the brand name Delestrogen.[18][19][102] In 1966, oral estradiol valerate was introduced by Schering for medical use in Europe under the brand name Progynova.[103][104][105][106][107] A report of its metabolism was published in 1967.[108] Esterification of estradiol, as in estradiol valerate, has been claimed to improve its metabolic stability with oral administration.[4][3][109] In 1968, micronized preparations of oral estradiol valerate were first introduced under the brand names Progynova 21 and Progynova 21 mite.[103] Along with estradiol benzoate (1933)[110][111][112] and estradiol cypionate (1952),[113] estradiol valerate is one of the most widely used esters of estradiol.[20]
Society and culture
Generic names
Estradiol valerate is the generic name of the drug and its INN, USAN, BANM, and JAN, while oestradiol valerate was formerly its BANM.[21][22][114]
Brand names
Estradiol valerate has been marketed under the brand names Altadiol, Androtardyl-Oestradiol, Ardefem, Climaval, Cyclabil, Cyclocur, Deladiol, Delahormone Unimatic, Delestrogen, Delestrogen 4X, Depogen, Diol-20, Dioval, Ditate, Dura-Estate, Dura-Estradiol, Duratrad, Duragen, Estate, Estra-L, Estradiol Depot, Estraval, Estraval Depot, Estraval PA, Estravel, Femogen, Femogex, Gynogen L.A., Gynokadin, Lastrogen, Menaval, Merimono, Neofollin, Nuvelle, Oestrogynal, Ostrin Depo, Pelanin, Pharlon, Postoval, Primogyna, Primogyn, Primogyn Depot, Progynon, Progynon Depot, Progynova, Repestrogen, Repo-Estra, Reposo-E, Retestrin, Ronfase, Span-Est, Testaval, and Valergen, among others.[21][22][18][115][114] Neofollin is an oil solution of estradiol valerate.[116][117]
Availability
Oral estradiol valerate is used primarily in Europe, under the brand name Progynova.[118] Although oral estradiol valerate was previously available in the United States ,[22] it is no longer available in this country except in combination with dienogest as a combined oral contraceptive (under the brand name Natazia).[37] Estradiol valerate by intramuscular injection is available under the brand name Delestrogen in the United States and Canada and under the brand name Progynon Depot in Europe and elsewhere in the world.[37][22]
Research
SH-834 was a combination of 90 mg estradiol valerate and 300 mg gestonorone caproate for weekly intramuscular injection that was developed by Schering in the 1970s.[52][119][120] It was investigated clinically as a treatment for breast cancer and was found to be effective, but was never marketed.[52][50]
See also
- Estradiol valerate/hydroxyprogesterone caproate
- Estradiol valerate/norethisterone enantate
- Estradiol valerate/prasterone enanthate
- Estradiol valerate/testosterone enanthate
References
- ↑ 1.0 1.1 1.2 "Estradiol and dienogest Advanced Patient Information". https://www.drugs.com/cons/estradiol-and-dienogest.html.
- ↑ Dictionary of Obstetrics and Gynecology. Walter de Gruyter. 1 January 1988. p. 86. ISBN 978-3-11-085727-6. https://books.google.com/books?id=EQlvzV9V7xIC&pg=PA86. Retrieved 20 May 2012.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 3.23 3.24 3.25 3.26 3.27 3.28 3.29 3.30 "Pharmacokinetic and pharmacological features of oestradiol valerate". Maturitas 4 (4): 315–324. December 1982. doi:10.1016/0378-5122(82)90064-0. PMID 7169965.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 "Pharmacology of estrogens and progestogens: influence of different routes of administration". Climacteric 8 (Suppl 1): 3–63. August 2005. doi:10.1080/13697130500148875. PMID 16112947.
- ↑ 5.0 5.1 "Animal toxicity studies performed for risk assessment of the once-a-month injectable contraceptive Mesigyna". Contraception 49 (4): 303–333. April 1994. doi:10.1016/0010-7824(94)90030-2. PMID 8013217.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedpmid23375353 - ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 "Bioavailability and pharmacodynamics of two 10-mg estradiol valerate depot formulations following IM single dose administration in healthy postmenopausal volunteers". International Journal of Clinical Pharmacology and Therapeutics 50 (2): 100–117. February 2012. doi:10.5414/CP201589. PMID 22257576.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 "A comparison of the pharmacokinetic properties of three estradiol esters". Contraception 21 (4): 415–424. April 1980. doi:10.1016/S0010-7824(80)80018-7. PMID 7389356.
- ↑ 9.0 9.1 9.2 9.3 "Natürliche und Synthetische Sexualhormone – Biologische Grundlagen und Behandlungsprinzipien" (in de). Grundlagen und Klinik der Menschlichen Fortpflanzung. Walter de Gruyter. 1988. pp. 229–306. ISBN 978-3110109689. OCLC 35483492. https://books.google.com/books?id=v4HvAQAACAAJ.
- ↑ 10.0 10.1 Clinical Endocrinology: Theory and Practice. Springer Science & Business Media. 6 December 2012. pp. 551–. ISBN 978-3-642-96158-8. https://books.google.com/books?id=DAgJCAAAQBAJ&pg=PA551.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 11.7 "DELESTROGEN (estradiol valerate injection, USP)". Par Pharmaceutical, Inc.. U.S. Food and Drug Administration. November 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/009402s052lbl.pdf.
- ↑ 12.0 12.1 12.2 12.3 12.4 "PROGYNOVA Product Information". Bayer group, Germany. 20 October 2016. http://www.bayerresources.com.au/resources/uploads/pi/file9418.pdf.
- ↑ 13.0 13.1 Mayo Clinic Internal Medicine Board Review. OUP USA. 23 September 2010. pp. 222–. ISBN 978-0-19-975569-1. https://books.google.com/books?id=LS65jBzoD40C&pg=PA222.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 14.6 14.7 Estrogens and Antiestrogens II: Pharmacology and Clinical Application of Estrogens and Antiestrogen. Springer Science & Business Media. 6 December 2012. p. 261. ISBN 978-3-642-60107-1. https://books.google.com/books?id=wBvyCAAAQBAJ&pg=PA261. "Natural estrogens considered here include: [...] Esters of 17β-estradiol, such as estradiol valerate, estradiol benzoate and estradiol cypionate. Esterification aims at either better absorption after oral administration or a sustained release from the depot after intramuscular administration. During absorption, the esters are cleaved by endogenous esterases and the pharmacologically active 17β-estradiol is released; therefore, the esters are considered as natural estrogens."
- ↑ 15.0 15.1 "Bioidentical hormone therapy: a review of the evidence". Journal of Women's Health 16 (5): 600–631. June 2007. doi:10.1089/jwh.2006.0311. PMID 17627398.
- ↑ 16.0 16.1 "Injectable Contraceptives Till Date". Progress in Obstetrics and Gynecology--3. Jaypee Brothers Medical Publishers Pvt. Ltd.. 15 December 2012. pp. 419–. ISBN 978-93-5090-575-3. https://books.google.com/books?id=AS3UBAAAQBAJ&pg=PA419.
- ↑ 17.0 17.1 17.2 Pharmaceutical Substances, 5th Edition, 2009: Syntheses, Patents and Applications of the most relevant APIs. Thieme. 14 May 2014. pp. 1167–1174. ISBN 978-3-13-179525-0. https://books.google.com/books?id=fO2IAwAAQBAJ&pg=PA1167.
- ↑ 18.0 18.1 18.2 William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia, 3rd Edition. Elsevier. pp. 1477–1478. ISBN 978-0-8155-1856-3. https://books.google.com/books?id=_J2ti4EkYpkC&pg=PA1477.
- ↑ 19.0 19.1 Research and development, market power, and patent policy in ethical drugs. University of Wisconsin--Madison. 1969. p. 95. https://books.google.com/books?id=4vdsAAAAMAAJ&q=Delestrogen. "1954. Delestrogen. Estradiol valerate."
- ↑ 20.0 20.1 Reproductive endocrinology: physiology, pathophysiology, and clinical management. Saunders. 1991. ISBN 978-0-7216-3206-3. https://books.google.com/books?id=RN1qAAAAMAAJ. Retrieved 20 May 2012.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. 14 November 2014. pp. 898–. ISBN 978-1-4757-2085-3. https://books.google.com/books?id=0vXTBwAAQBAJ&pg=PA898.
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 22.6 22.7 22.8 Index Nominum 2000: International Drug Directory. Taylor & Francis US. 2000. p. 405. ISBN 978-3-88763-075-1. https://books.google.com/books?id=5GpcTQD_L2oC&pg=PA405. Retrieved 20 May 2012.
- ↑ "Generic Delestrogen Availability". https://www.drugs.com/availability/generic-delestrogen.html.
- ↑ 24.0 24.1 24.2 "Review of the safety, efficacy and patient acceptability of the combined dienogest/estradiol valerate contraceptive pill". International Journal of Women's Health 2: 279–290. August 2010. doi:10.2147/IJWH.S6954. PMID 21151673.
- ↑ 25.0 25.1 "A review of "once-a-month" combined injectable contraceptives". Journal of Obstetrics and Gynaecology 4 (Suppl 1): S1-34. 1994. doi:10.3109/01443619409027641. PMID 12290848.
- ↑ 26.0 26.1 "New technologies in contraception". BJOG 116 (2): 230–239. January 2009. doi:10.1111/j.1471-0528.2008.01985.x. PMID 19076955. http://wrap.warwick.ac.uk/28852/1/WRAP_Rowlands_NewtechnologiesincontraceptionBJOG2008_Uni_repos_version.pdf.
- ↑ 27.0 27.1 "Hormonal and Surgical Treatment Options for Transgender Women and Transfeminine Spectrum Persons". The Psychiatric Clinics of North America 40 (1): 99–111. March 2017. doi:10.1016/j.psc.2016.10.006. PMID 28159148.
- ↑ 28.0 28.1 "Gonadal suppressive and cross-sex hormone therapy for gender dysphoria in adolescents and adults". Pharmacotherapy 34 (12): 1282–1297. December 2014. doi:10.1002/phar.1487. PMID 25220381.
- ↑ 29.0 29.1 Principles of Transgender Medicine and Surgery. Routledge. 20 May 2016. pp. 216–. ISBN 978-1-317-51460-2. https://books.google.com/books?id=LwszDAAAQBAJ&pg=PA216.
- ↑ Transgender Care: Recommended Guidelines, Practical Information, and Personal Accounts. Temple University Press. 1 March 2001. pp. 64–. ISBN 978-1-56639-852-7. https://books.google.com/books?id=IlPX6E5glDEC&pg=PA64.
- ↑ "The use of high-dose estrogens for the treatment of breast cancer". Maturitas 95: 11–23. January 2017. doi:10.1016/j.maturitas.2016.10.010. PMID 27889048.
- ↑ "Breast cancer: current and future endocrine therapies". Molecular and Cellular Endocrinology 382 (1): 695–723. January 2014. doi:10.1016/j.mce.2013.08.001. PMID 23933149.
- ↑ "Recognizing and Treating Dangerous Sex Offenders". International Journal of Offender Therapy and Comparative Criminology 16 (2): 109–115. June 1972. doi:10.1177/0306624X7201600202. ISSN 0306-624X.
- ↑ American Medical Association. Dept. of Drugs; Council on Drugs (American Medical Association); American Society for Clinical Pharmacology and Therapeutics (1 February 1977). "Estrogens, Progestagens, Oral Contraceptives, and Ovulatory Agents". AMA drug evaluations. Publishing Sciences Group. pp. 540–572. ISBN 978-0-88416-175-2. https://books.google.com/books?id=0h7s_rfEZgkC. "Intramuscular: For replacement therapy, (Estradiol, Estradiol Benzoate) 0.5 to 1.5 mg two or three times weekly; (Estradiol Cypionate) 1 to 5 mg weekly for two or three weeks; (Estradiol Dipropionate) 1 to 5 mg every one to two weeks; (Estradiol Valerate) 10 to 40 mg every one to four weeks."
- ↑ "Hormonal Treatment of Disorders of the Menstrual Cycle". Ovarian Function and its Disorders. Springer Science & Business Media. 1981. pp. 309–332. doi:10.1007/978-94-009-8195-9_11. ISBN 978-94-009-8195-9. https://books.google.com/books?id=7IrpCAAAQBAJ&pg=PA310.
- ↑ The Cyclopedia of Medicine, Surgery, Specialties. F. A. Davis Company. 1975. https://books.google.com/books?id=RiE9K5bgKcsC.
- ↑ 37.0 37.1 37.2 37.3 37.4 37.5 37.6 "Drugs@FDA: FDA Approved Drug Products". United States Food and Drug Administration. http://www.accessdata.fda.gov/scripts/cder/daf/.
- ↑ European Drug Index: European Drug Registrations (Fourth ed.). CRC Press. 19 June 1998. pp. 276, 313, 379, 561, 566. ISBN 978-3-7692-2114-5. https://books.google.com/books?id=2HBPHmclMWIC&pg=PA276.
- ↑ Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. 2001. pp. 2153–. ISBN 978-0-7817-1750-2. https://books.google.com/books?id=FVfzRvaucq8C&pg=PA2153.
- ↑ 40.0 40.1 "Preparation of endometrium for egg donation". Human Reproduction Update 4 (6): 856–861. 1998. doi:10.1093/humupd/4.6.856. PMID 10098476. "Oestradiol valerate and oestradiol in a micronized form are the most widely used oestrogen per os for steroid substitution therapy. Our regimen, as of most other groups [...] is oestradiol valerate (Progynova; Schering, Berlin, Germany) given in various concentrations throughout the cycle [...]. According to Norfolk's protocol, 2 mg of micronized oestradiol valerate are given on cycle days 1–5. [...] In tablet form, micronized oestradiol valerate is also efficiently absorbed [...]".
- ↑ 41.0 41.1 The Climacteric in Perspective: Proceedings of the Fourth International Congress on the Menopause, held at Lake Buena Vista, Florida, October 28–November 2, 1984. Springer Science & Business Media. 6 December 2012. pp. 397, 399. ISBN 978-94-009-4145-8. https://books.google.com/books?id=VM0hBQAAQBAJ&pg=PA397.
- ↑ 42.0 42.1 42.2 "Clinical use of oestrogens and progestogens". Maturitas 12 (3): 199–214. September 1990. doi:10.1016/0378-5122(90)90004-P. PMID 2215269.
- ↑ Current Management of the Menopause. CRC Press. 22 June 2005. pp. 95–98,488. ISBN 978-0-203-48612-2. https://books.google.com/books?id=WD7S7677xUUC&pg=PA95.
- ↑ "Hormone Substitution Before, During and After Menopause". Menopause – Andropause: Hormone Replacement Therapy Through the Ages. Krause & Pachernegg: Gablitz. 2001. pp. 67–88. ISBN 978-3-901299-34-6. https://www.kup.at/kup/pdf/4978.pdf.
- ↑ "Contraindications to estrogen therapy and management of the menopausal syndrome in these cases". The Management of the Menopause & Post-Menopausal Years: The Proceedings of the International Symposium held in London 24–26 November 1975 Arranged by the Institute of Obstetrics and Gynaecology, The University of London. MTP Press Limited. 1976. pp. 377–382. doi:10.1007/978-94-011-6165-7_33. ISBN 978-94-011-6167-1.
- ↑ 46.0 46.1 "Pharmacotherapy Considerations in the Management of Transgender Patients: A Brief Review". Pharmacotherapy 35 (12): 1130–1139. December 2015. doi:10.1002/phar.1668. PMID 26684553.
- ↑ "Hormontherapie bei gynäkologischen Erkrankungen". Praktische Hormontherapie in der Gynäkologie. Walter de Gruyter. 10 December 2008. pp. 245–314. ISBN 978-3-11-020864-1. https://books.google.com/books?id=E3SuivmVMnQC&pg=PA245. "Dosierungsbeispiele bei Mammahypoplasie und Infantilismus [...] Parenteral 1. 40 mg Estradiolvalerat (Estradiol-Depot 10 mg JENAPHARM) und 250 mg Hydroxyprogesteroncaproat (Progesteron-Depot JENAPHARM, Proluton Depot) i. m. einmal wöchentlich über 15–20 Wochen lang. 2. 20–40 mg Estradiolvalerat (Estradiol-Depot 10 mg JENAPHARM) i. m. in der ersten und zweiten Woche. 40 mg Estradiolvalerat (Estradiol-Depot 10 mg JENAPHARM) und 250 mg Hydroxyprogesteroncaproat (Progesteron-Depot JENAPHARM, Proluton Depot) i. m. in der dritten und vierten Woche. Therapiedauer 4–5 Monate. Evtl. Abstand zwischen 2 Injektionen auf 2 Wochen erweitern (Abb. 6.2)."
- ↑ 48.0 48.1 "Rapid increase in lumbar spine bone density in osteopenic women by high-dose intramuscular estrogen-progestogen injections. A preliminary report". Hormone and Metabolic Research = Hormon- und Stoffwechselforschung = Hormones et Metabolisme 26 (9): 428–431. September 1994. doi:10.1055/s-2007-1001723. PMID 7835827.
- ↑ "[The treatment of inoperable and metastasizing breast carcinoma with gestational and estrogenci hormones]" (in de). Munchener Medizinische Wochenschrift 108 (39): 1920–1923. September 1966. PMID 6014870.
- ↑ 50.0 50.1 "[The combined estrogen-gestagen treatment of metastasizing mammary carcinoma using with SH 834]" (in de). Deutsche Medizinische Wochenschrift 95 (48): 2399+. November 1970. doi:10.1055/s-0028-1108843. PMID 5529652.
- ↑ "Die Wirkung einer Ostrogen-Gestagen-Kombinationstherapie beim fortgeschrittenen Mammakarzinom mit besonderer Berucksichtigung der Lungenmetastasen" (in de). Strahlentherapie 141 (5): 540–548. ISSN 0039-2073. https://www.popline.org/node/485956.
- ↑ 52.0 52.1 52.2 "Hormonal treatment of mammary carcinoma with Progynon-Depot and Depostat". Acta Radiologica 14 (5): 433–442. October 1975. doi:10.3109/02841867509132684. PMID 1202923.
- ↑ "[Additive treatment of metastasizing breast cancer with special reference to postmenopausal age (results of a randomized study)]" (in de). Strahlentherapie 152 (3): 235–247. September 1976. PMID 968923.
- ↑ "[Comparison of histological and cytological studies of the prostate with special reference to oestrogene induced changes (author's transl)"] (in de). Verhandlungen der Deutschen Gesellschaft für Pathologie 57: 315–318. 1973. PMID 4142204. https://www.popline.org/node/508573.
- ↑ "Morphological criteria for the control of carcinoma of the prostate with estrogen therapy". International Urology and Nephrology 6 (3–4): 195–200. 1974. doi:10.1007/BF02089265. PMID 4142482.
- ↑ The Transsexual Phenomenon. Ace Publishing Company. 1966. p. 107. https://books.google.com/books?id=hArbAAAAMAAJ. "In my own practice, Squibb's Delestrogen for intramuscular injections was employed with much satisfaction and positive results. This is a slowly absorbing, well-tolerated, potent preparation (chemically, Estradiol Valerate), and was applied in doses of 20 to 60 mg. (½ to 1 ½ cc.). Usually 30 to 60 mg. of Delalutin (Squibb) was added, an equally potent progesterone. This combination was given once a week or once in two to three weeks, according to the response as measured by the patient's emotional balance and physical feminization symptoms. Generally I found that dosage seems less important than length and regularity of administration."
- ↑ "Transvestism and Transsexualism in the male and female1". Journal of Sex Research 3 (2): 107–127. 1967. doi:10.1080/00224496709550519. ISSN 0022-4499. "Estrogen treatment—as already indicated—helps greatly but does not cure. I have employed either Squibb's Delestrogen, a slowly absorbing, highly potent preparation which is, chemically, estradiol valerate (40 mg. to 1 cc); or the still more potent Delestrec, which is estradiol undecylate (100 mg. to 1 cc). This preparation, however, is not yet on the market in this country, though it is widely used in Europe. In the majority of cases, I used from 30 to 100 mg. weekly, or every two to three weeks, by intramuscular injection.".
- ↑ "Role of cytochrome P450 in estradiol metabolism in vitro". Acta Pharmacologica Sinica 22 (2): 148–154. February 2001. PMID 11741520.
- ↑ "Treatment of heavy menstrual bleeding with the estradiol valerate and dienogest oral contraceptive pill". Advances in Therapy 30 (1): 1–13. January 2013. doi:10.1007/s12325-012-0071-3. PMID 23239397.
- ↑ "Hormonal contraceptive regimens in the perimenopause". Maturitas 63 (3): 204–212. July 2009. doi:10.1016/j.maturitas.2009.05.001. PMID 19524378.
- ↑ "A comparison between effects of estradiol valerate and low dose ethinyl estradiol on haemostasis parameters". Thrombosis and Haemostasis 61 (1): 65–69. February 1989. doi:10.1055/s-0038-1646528. PMID 2526387.
- ↑ "Effect of four oral contraceptives on hemostatic parameters". Contraception 70 (2): 97–106. August 2004. doi:10.1016/j.contraception.2004.03.004. PMID 15288212.
- ↑ 63.0 63.1 "[Oral combined contraception: is there any difference between ethinyl-estradiol and estradiol?]" (in fr). Gynecologie, Obstetrique & Fertilite 40 (2): 109–115. February 2012. doi:10.1016/j.gyobfe.2011.10.009. PMID 22244780.
- ↑ "Risks of estrogens and progestogens". Maturitas 12 (3): 215–246. September 1990. doi:10.1016/0378-5122(90)90005-q. PMID 2170823. https://dipot.ulb.ac.be/dspace/bitstream/2013/352796/3/MATURITAS1990MLHEPRISKS.pdf.
- ↑ "Estrogen induction of liver proteins and high-density lipoprotein cholesterol: comparison between estradiol valerate and ethinyl estradiol". Gynecologic and Obstetric Investigation 22 (4): 198–205. 1986. doi:10.1159/000298914. PMID 3817605.
- ↑ "The effects of estradiol on blood lipids and lipoproteins in postmenopausal women". Obstetrics and Gynecology 72 (5): 18S–22S. November 1988. PMID 3173937.
- ↑ "Metabolic effects of contraceptive steroids". Reviews in Endocrine & Metabolic Disorders 12 (2): 63–75. June 2011. doi:10.1007/s11154-011-9182-4. PMID 21538049.
- ↑ "An overview of the development of combined oral contraceptives containing estradiol: focus on estradiol valerate/dienogest". Gynecological Endocrinology 28 (5): 400–408. May 2012. doi:10.3109/09513590.2012.662547. PMID 22468839.
- ↑ "High dose estrogen treatment increases bone mineral density in male-to-female transsexuals receiving gonadotropin-releasing hormone agonist in the absence of testosterone". European Journal of Endocrinology 153 (1): 107–113. July 2005. doi:10.1530/eje.1.01943. PMID 15994752.
- ↑ "Effects on the male endocrine system of long-term treatment with gonadotropin-releasing hormone agonists and estrogens in male-to-female transsexuals". Hormone and Metabolic Research = Hormon- und Stoffwechselforschung = Hormones et Metabolisme 38 (3): 183–187. March 2006. doi:10.1055/s-2006-925198. PMID 16673210.
- ↑ "Can changes in sex hormone binding globulin predict the risk of venous thromboembolism with combined oral contraceptive pills?". Acta Obstetricia et Gynecologica Scandinavica 81 (6): 482–490. June 2002. doi:10.1034/j.1600-0412.2002.810603.x. PMID 12047300.
- ↑ "Progynova 1mg (SPC) | Drugs.com". https://www.drugs.com/uk/progynova-1mg-spc-3430.html.
- ↑ 73.0 73.1 73.2 "Pharmacology of estrogens". The Climacteric in Perspective. 1986. pp. 393–410. doi:10.1007/978-94-009-4145-8_36. ISBN 978-94-010-8339-3. https://books.google.com/books?id=VM0hBQAAQBAJ&pg=PA401.
- ↑ 74.0 74.1 "Pharmacokinetic and pharmacologic variation between different estrogen products". Journal of Clinical Pharmacology 35 (9S): 18S–24S. September 1995. doi:10.1002/j.1552-4604.1995.tb04143.x. PMID 8530713.
- ↑ 75.0 75.1 75.2 "[Cross-over comparison of the pharmacokinetics of estradiol during hormone replacement therapy with estradiol valerate or micronized estradiol]" (in de). Zentralblatt für Gynäkologie 123 (9): 505–512. September 2001. doi:10.1055/s-2001-18223. PMID 11709743.
- ↑ "Review of clinical experience with estradiol in combined oral contraceptives". Contraception 81 (1): 8–15. January 2010. doi:10.1016/j.contraception.2009.08.010. PMID 20004267.
- ↑ "Enterohepatic cycling and pharmacokinetics of oestradiol in postmenopausal women". The Journal of Pharmacy and Pharmacology 50 (8): 857–864. August 1998. doi:10.1111/j.2042-7158.1998.tb04000.x. PMID 9751449.
- ↑ 78.0 78.1 78.2 "Bioequivalence assessment of three different estradiol formulations in postmenopausal women in an open, randomized, single-dose, 3-way cross-over study". European Journal of Drug Metabolism and Pharmacokinetics 24 (1): 47–53. 1999. doi:10.1007/BF03190010. PMID 10412891.
- ↑ "Comparison of the pharmacologic and clinical profiles of new combined oral contraceptives containing estradiol". Open Access Journal of Contraception: 39. 2013. doi:10.2147/OAJC.S50693. ISSN 1179-1527.
- ↑ 80.0 80.1 80.2 80.3 80.4 80.5 80.6 80.7 "Oocyte donation in 61 patients". Lancet 1 (8648): 1185–1187. May 1989. doi:10.1016/S0140-6736(89)92762-1. PMID 2566746.
- ↑ 81.0 81.1 81.2 81.3 81.4 81.5 81.6 81.7 "Oocyte donation and surrogacy". British Medical Bulletin 46 (3): 796–812. July 1990. doi:10.1093/oxfordjournals.bmb.a072432. PMID 2207608.
- ↑ "Gender affirmative care of transgender people: a single center's experience in Korea". Obstetrics & Gynecology Science 62 (1): 46–55. January 2019. doi:10.5468/ogs.2019.62.1.46. PMID 30671393. "When we prescribed estradiol, we preferred sublingual estradiol valerate instead of the oral form for feminizing HT since prior researchers have reported the effectiveness of sublingual administration in maintaining high blood estradiol concentration and low E1/E2 ratio [13].".
- ↑ "The acute effects of sublingual 17beta-estradiol on the cardiovascular system". Maturitas 33 (1): 81–85. September 1999. doi:10.1016/S0378-5122(99)00036-5. PMID 10585176.
- ↑ "Steroids". Medicinal Chemistry. Pearson Education India. 2007. p. 427. ISBN 978-81-317-0031-0. https://books.google.com/books?id=9HSoZrcBRl0C&pg=PA427. Retrieved 20 May 2012.
- ↑ 85.0 85.1 85.2 85.3 "Plasma levels of dehydroepiandrosterone and 17 beta-estradiol after intramuscular administration of Gynodian-Depot in 3 women". Hormone Research 17 (2): 84–89. 1983. doi:10.1159/000179680. PMID 6220949.
- ↑ 86.0 86.1 86.2 86.3 86.4 86.5 "Pharmacokinetics and biotransformation of estradiol valerate in ovariectomized women". Hormone Research 21 (3): 145–154. 1985. doi:10.1159/000180039. PMID 2987096.
- ↑ 87.0 87.1 87.2 "Pharmakokinetik von Estron, Estradiol, FSH, LH und Prolaktin nach intramuskulärer Applikation von 5 mg Estradiolvalerat". Journal für Menopause 9 (2): 51–55. 2002. https://www.kup.at/journals/summary/1071.html.
- ↑ 88.0 88.1 88.2 del Cisne Valle Alvarez D (11 May 2011). Efecto de una Dosis de 50 mg de Enantato de Noretisterona y 5 mg de Valerato de Estradiol en los Niveles de Testosterona Total en Hombres Mexicanos Sanos [Effect of a Dose of 50 mg of Norethisterone Enanthate and 5 mg of Estradiol Valerate on Total Testosterone Levels in Healthy Mexican Men] (MSc). National Polytechnic Institute of Mexico.
- ↑ 89.0 89.1 89.2 "Longacting steroid preparations". Acta Clinica Belgica 30 (1): 48–55. 1975. doi:10.1080/17843286.1975.11716973. PMID 1231448.
- ↑ 90.0 90.1 (in de) Das Klimakterium – Pathophysiologie, Klinik, Therapie. Stuttgart, Germany: Thieme Verlag. 1987. p. 122. ISBN 978-3137008019.
- ↑ 91.0 91.1 91.2 "Serum oestrone, oestradiol and oestriol concentrations in castrated women during intramuscular oestradiol valerate and oestradiolbenzoate-oestradiolphenylpropionate therapy". Maturitas 2 (1): 53–58. January 1980. doi:10.1016/0378-5122(80)90060-2. PMID 7402086.
- ↑ 92.0 92.1 92.2 Untersuchungen zur Pharmakokinetik von Östradiol-17β, Östradiol-Benzoat, Östradiol-Valerianat und Östradiol-Undezylat bei der Frau: der Verlauf der Konzentrationen von Östradiol-17β, Östron, LH und FSH im Serum. 1975. pp. 1–34. OCLC 632312599. https://books.google.com/books?id=cJ82vwEACAAJ.
- ↑ 93.0 93.1 93.2 "[Estradiol-17beta, estrone, LH and FSH in serum after administration of estradiol-17beta, estradiolbenzoate, estradiol-valeriate and estradiol-undecylate in the female (author's transl)]" (in de). Geburtshilfe und Frauenheilkunde 35 (5): 370–374. May 1975. PMID 1150068.
- ↑ 94.0 94.1 94.2 "Postmenopausal estrogen and androgen replacement and lipoprotein lipid concentrations". American Journal of Obstetrics and Gynecology 156 (2): 414–419. February 1987. doi:10.1016/0002-9378(87)90295-x. PMID 3826177.
- ↑ 95.0 95.1 "Pharmacokinetics of once-a-month injectable contraceptives". Contraception 49 (4): 347–359. April 1994. doi:10.1016/0010-7824(94)90032-9. PMID 8013219.
- ↑ "Hormone therapy for transgender patients". Translational Andrology and Urology 5 (6): 877–884. December 2016. doi:10.21037/tau.2016.09.04. PMID 28078219.
- ↑ "Comparative pharmacokinetics and pharmacodynamics after subcutaneous and intramuscular administration of medroxyprogesterone acetate (25 mg) and estradiol cypionate (5 mg)". Contraception 84 (6): 565–570. December 2011. doi:10.1016/j.contraception.2011.03.014. PMID 22078184.
- ↑ "Estradiol valerate | C23H32O3 | ChemSpider". http://www.chemspider.com/Chemical-Structure.13194.html.
- ↑ "Esters of unsaturated polyhydroxy estrane". https://patents.google.com/patent/US2205627A/en.
- ↑ "Tools for making correct decisions regarding hormone therapy. part I: background and drugs". Fertility and Sterility 81 (6): 1447–1457. June 2004. doi:10.1016/j.fertnstert.2003.10.052. PMID 15193460.
- ↑ "Über protrahiert wirksame Östrogene". Naunyn-Schmiedebergs Archiv für Experimentelle Pathologie und Pharmakologie 220 (5). 1953. doi:10.1007/BF00246561. ISSN 0028-1298.
- ↑ "Über ovarielle Agenesie". Zeitschrift für Kinderheilkunde 75 (3): 224–234. 1954. doi:10.1007/BF00439822. ISSN 0340-6199. "Um die "Menarche" sollte eine verstärkte Substitutionstherapie (20 Tage lang tgl. 0,1 mg Follikelhormon per os oder einmalig Progynon-Depot (10 mg i.m.), [...]".
- ↑ 103.0 103.1 (in de) Klimakterium, Postmenopause und Hormonsubstitution (4 ed.). UNI-MED-Verlag. 1 January 2008. p. 18. ISBN 978-3-83742-043-2. "With Progynon Depot-10, an oily solution of 10 mg estradiol valerate, an injection preparation had been available since 1953 and since 1966 coated tablets with estradiol valerate for oral therapy. The first Schering preparation containing micronized estradiol was marketed in 1968 as Progynova 21 (2 mg) and Progynova 21 mite (1 mg)."
- ↑ "Neue Spezialitäten". Klinische Wochenschrift 44 (23): 1381. 1966. doi:10.1007/BF01747900. ISSN 0023-2173. "NEUE SPEZIALITATEN [...] Progynova. 1 Dragee enthält 2 mg Oestradiolvalerinat (Klimakterium). Hersteller: Schering AG, Berlin 65.".
- ↑ "[The management of climacteric disorders using estradiol valerate (Progynova)]" (in de). Medizinische Klinik 62 (35): 1356–61 passim. September 1967. PMID 5593020.
- ↑ "[The peroral treatment of the climacteric syndrome with estradiol valerate]" (in de). Wiener Klinische Wochenschrift 80 (12): 229–233. March 1968. PMID 5728263.
- ↑ "[Therapy of climacteric deficiency symptoms using progynova]" (in de). Die Medizinische Welt 23 (22): 834–836. May 1972. PMID 5045321.
- ↑ "The metabolism of oestradiol valerate". Medizinische Mitteilungen (Schering) 28: 16–. 1967. ISSN 0301-2492. https://scholar.google.com/scholar?cluster=14998892125998427533.
- ↑ "Drugs@FDA: FDA-Approved Drugs". https://www.accessdata.fda.gov/scripts/cder/daf/.
- ↑ "Die Behandlung der Amenorrhöe mit Hohen Dosen der Ovarialhormone". Klinische Wochenschrift 12 (40): 1557–1562. 1933. doi:10.1007/BF01765673. ISSN 0023-2173.
- ↑ "Neue Wege der Hormontherapie in der Gynäkologie". Deutsche Medizinische Wochenschrift 60 (11): 389–393. 2009. doi:10.1055/s-0028-1129842. ISSN 0012-0472.
- ↑ "Commercial Glandular Products". Journal of the American Medical Association 105 (9): 667. 1935. doi:10.1001/jama.1935.92760350007009a. ISSN 0002-9955. "Progynon-B, Schering Corporation: This is crystalline hydroxyestrin benzoate obtained by hydrogenation of theelin and subsequent conversion to the benzoate. [...] Progynon-B is marketed in ampules containing 1 cc. of a sesame oil solution of hydroxyestrin benzoate of either 2,500, 5,000, 10,000 or 50,000 international units.".
- ↑ Pharmaceutical Manufacturing Encyclopedia. William Andrew. 1 January 1988. pp. 575–576. ISBN 978-0-8155-1144-1. https://books.google.com/books?id=X2EyLsG4bcUC&pg=PA576. Retrieved 20 May 2012.
- ↑ 114.0 114.1 "Estradiol". https://www.drugs.com/international/estradiol.html.
- ↑ Hazardous Chemicals Desk Reference. John Wiley & Sons. 13 June 2008. pp. 594–. ISBN 978-0-470-18024-2. https://books.google.com/books?id=WZeBDwAAQBAJ&pg=PA594.
- ↑ "Menopauzální symptomy a hormonální substituční terapie" (in cs). Praktické Lékárenství 10 (2): 68–73. 2014. ISSN 1801-2434. http://www.medvik.cz/link/bmc14059249.
- ↑ "NEOFOLLIN Injekční roztok (Estradioli valeras)". http://www.sukl.cz/download/pil/PI16359.pdf.
- ↑ Primary Care in Obstetrics and Gynecology: A Handbook for Clinicians. Springer Science & Business Media. January 1998. pp. 227–. ISBN 978-0-387-94739-6. https://books.google.com/books?id=jfmB3aNSGfoC&pg=PA227.
- ↑ "Progestogen therapy for ovarian carcinoma". The Journal of Obstetrics and Gynaecology of the British Commonwealth 79 (6): 555–559. June 1972. doi:10.1111/j.1471-0528.1972.tb14200.x. PMID 4555897.
- ↑ "[Effect of estrogen-gestagen combination therapy in advanced breast carcinoma with special reference to pulmonary metastases"] (in de). Strahlentherapie 141 (5): 540–548. May 1971. PMID 5088730. https://www.popline.org/node/485956.
Further reading
- "Longacting steroid preparations". Acta Clinica Belgica 30 (1): 48–55. 1975. doi:10.1080/17843286.1975.11716973. PMID 1231448.
- "Pharmacokinetic and pharmacological features of oestradiol valerate". Maturitas 4 (4): 315–324. December 1982. doi:10.1016/0378-5122(82)90064-0. PMID 7169965.
- "Pharmacodynamic effects of once-a-month combined injectable contraceptives". Contraception 49 (4): 361–385. April 1994. doi:10.1016/0010-7824(94)90033-7. PMID 8013220.
- "Pharmacokinetic and pharmacologic variation between different estrogen products". Journal of Clinical Pharmacology 35 (9S): 18S–24S. September 1995. doi:10.1002/j.1552-4604.1995.tb04143.x. PMID 8530713.
- "Pharmacology of estrogens and progestogens: influence of different routes of administration". Climacteric 8 (Suppl 1): 3–63. August 2005. doi:10.1080/13697130500148875. PMID 16112947.
- "Ethinyl estradiol and 17β-estradiol in combined oral contraceptives: pharmacokinetics, pharmacodynamics and risk assessment". Contraception 87 (6): 706–727. June 2013. doi:10.1016/j.contraception.2012.12.011. PMID 23375353.
 |
![Baseline-adjusted estradiol levels after a single oral dose of 1.5 mg micronized estradiol or 2.0 mg estradiol valerate in postmenopausal women.[79][78] Source was Timmer & Geurts (1999).[78]](/wiki/images/thumb/0/0d/Estradiol_levels_with_oral_micronized_estradiol_and_oral_estradiol_valerate_in_postmenopausal_women.png/400px-Estradiol_levels_with_oral_micronized_estradiol_and_oral_estradiol_valerate_in_postmenopausal_women.png)
![Estradiol levels after a single oral dose of 2 mg micronized estradiol or 2 mg estradiol valerate and with continuous oral administration of 2 mg/day micronized estradiol or 2 mg/day estradiol valerate (at steady state) in postmenopausal women.[75] Source was Wiegratz et al. (2001).[75]](/wiki/images/thumb/2/2c/Estradiol_levels_after_a_single_dose_and_with_continuous_administration_of_oral_estradiol_or_oral_estradiol_valerate_in_women.png/377px-Estradiol_levels_after_a_single_dose_and_with_continuous_administration_of_oral_estradiol_or_oral_estradiol_valerate_in_women.png)
![Estrogen levels after a single intramuscular injection of 10 mg estradiol valerate in oil in 24 postmenopausal women.[7] Determinations were made for both Progynon Depot 10 and Estradiol Depot 10, for a total of 48 measurements per point.[7] Assays were performed using GC/MS-NCI/SIM.[7] Source was Schug et al. (2012).[7]](/wiki/images/thumb/d/d0/Estrogen_levels_after_a_single_intramuscular_injection_of_10_mg_estradiol_valerate_in_postmenopausal_women.png/300px-Estrogen_levels_after_a_single_intramuscular_injection_of_10_mg_estradiol_valerate_in_postmenopausal_women.png)
![Hormone levels after a single intramuscular injection of 5 mg estradiol valerate in oil in 17 postmenopausal women.[87] Assays were performed using EIA.[87] Estrone levels were likely overestimated, possibly due to cross reactivity of the assay with estrogen conjugates.[7] Source was Göretzlehner et al. (2002).[87]](/wiki/images/thumb/0/0c/Hormone_levels_after_a_single_intramuscular_injection_of_5_mg_estradiol_valerate_in_postmenopausal_women.png/300px-Hormone_levels_after_a_single_intramuscular_injection_of_5_mg_estradiol_valerate_in_postmenopausal_women.png)
![Hormone levels after a single intramuscular injection of estradiol valerate/norethisterone enanthate (5 mg/50 mg) (Mesigyna) in healthy young men.[88] Testosterone decreased from ~503 ng/dL to ~30 ng/dL (–94%).[88] Source was Valle Alvarez (2011).[88]](/wiki/images/thumb/4/4a/Hormone_levels_in_men_with_a_single_intramuscular_injection_of_5_mg_estradiol_valerate_and_50_mg_norethisterone_enanthate_in_oil.png/300px-Hormone_levels_in_men_with_a_single_intramuscular_injection_of_5_mg_estradiol_valerate_and_50_mg_norethisterone_enanthate_in_oil.png)
![Estradiol levels after single intramuscular injections of 5 mg of different estradiol esters in oil in about 10 premenopausal women each.[8] Assays were performed using RIA with CS.[8] Source was Oriowo et al. (1980).[8]](/wiki/images/thumb/3/33/Estradiol_levels_after_a_single_5_mg_intramuscular_injection_of_estradiol_esters.png/300px-Estradiol_levels_after_a_single_5_mg_intramuscular_injection_of_estradiol_esters.png)
![Estradiol levels after a single intramuscular injection of 10 mg estradiol valerate or 100 mg estradiol undecylate in oil both in 4 individuals each.[89] Subject characteristics and assay method were not described.[89] Source was Vermeulen (1975).[89]](/wiki/images/thumb/6/65/Estradiol_levels_after_a_single_intramuscular_injection_of_10_mg_estradiol_valerate_and_100_mg_estradiol_undecylate.png/300px-Estradiol_levels_after_a_single_intramuscular_injection_of_10_mg_estradiol_valerate_and_100_mg_estradiol_undecylate.png)
![Estradiol and DHEA levels after a single intramuscular injection of Gynodian Depot (4 mg estradiol valerate, 200 mg prasterone enanthate in oil) or Primogyn Depot (10 mg estradiol valerate in oil) in women.[90][85][91] Assays were performed using RIA.[85][91] Sources were Düsterberg & Wendt (1983) and Rauramo et al. (1980).[90][85][91]](/wiki/images/thumb/d/dd/Estradiol_and_dehydroepiandrosterone_levels_after_a_single_intramuscular_injection_of_Gynodian_Depot_in_women.png/300px-Estradiol_and_dehydroepiandrosterone_levels_after_a_single_intramuscular_injection_of_Gynodian_Depot_in_women.png)
![Estradiol levels after a short intravenous infusion of 20 mg estradiol in aqueous solution or an intramuscular injection of equimolar doses of estradiol esters in oil solution in postmenopausal women.[92][93] Assays were performed using RIA with CS.[92][93] Source was Geppert (1975).[92][93]](/wiki/images/thumb/b/b1/Estradiol_levels_after_injections_of_estradiol%2C_estradiol_benzoate%2C_estradiol_valerate%2C_and_estradiol_undecylate_in_women.png/300px-Estradiol_levels_after_injections_of_estradiol%2C_estradiol_benzoate%2C_estradiol_valerate%2C_and_estradiol_undecylate_in_women.png)
![Estradiol levels after an intramuscular injection of 10 mg estradiol valerate in oil, Climacteron (150 mg testosterone enanthate, 1 mg estradiol benzoate, 7.5 mg estradiol dienanthate in oil), and control group in 20, 11, and 11 ovariectomized women, respectively.[94] Assays were performed using RIA.[94] Source was Sherwin et al. (1987).[94]](/wiki/images/thumb/e/e5/Estradiol_levels_after_an_intramuscular_injection_of_Climacteron_or_estradiol_valerate_in_ovariectomized_women.png/300px-Estradiol_levels_after_an_intramuscular_injection_of_Climacteron_or_estradiol_valerate_in_ovariectomized_women.png)
![Simplified curves of estradiol levels after injection of different estradiol esters in women.[95] Source was Garza-Flores (1994).[95]](/wiki/images/thumb/8/8c/Idealized_curves_of_estradiol_levels_after_injection_of_different_estradiol_esters_in_women.png/293px-Idealized_curves_of_estradiol_levels_after_injection_of_different_estradiol_esters_in_women.png)
