Chemistry:Nalidixic acid
 | |
| Clinical data | |
|---|---|
| Trade names | NegGram, Wintomylon, others |
| AHFS/Drugs.com | Consumer Drug Information |
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | 90% |
| Metabolism | Partially Hepatic |
| Elimination half-life | 6-7 hours, significantly longer in renal impairment |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
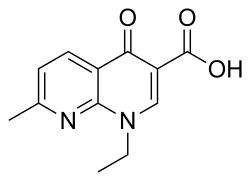
| Formula | C12H12N2O3 |
| Molar mass | 232.239 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Nalidixic acid (tradenames Nevigramon, NegGram, Wintomylon and WIN 18,320) is the first of the synthetic quinolone antibiotics.
In a technical sense, it is a naphthyridone, not a quinolone: its ring structure is a 1,8-naphthyridine nucleus that contains two nitrogen atoms, unlike quinoline, which has a single nitrogen atom.[1]
Synthetic quinolone antibiotics were discovered by George Lesher and coworkers as a byproduct of chloroquine manufacture in the 1960s;[2] nalidixic acid itself was used clinically, starting in 1967.
Nalidixic acid is effective primarily against Gram-negative bacteria, with minor anti-Gram-positive activity. In lower concentrations, it acts in a bacteriostatic manner; that is, it inhibits growth and reproduction. In higher concentrations, it is bactericidal, meaning that it kills bacteria instead of merely inhibiting their growth.
It has historically been used for treating urinary tract infections, caused, for example, by Escherichia coli, Proteus, Shigella, Enterobacter, and Klebsiella. It is no longer clinically used for this indication in the US as less toxic and more effective agents are available. The marketing authorization for nalidixic acid has been suspended throughout the EU.[3]
It is also a tool in studies as a regulation of bacterial division. It selectively and reversibly blocks DNA replication in susceptible bacteria. Nalidixic acid and related antibiotics inhibit a subunit of DNA gyrase and topoisomerase IV and induce formation of cleavage complexes.[4] It also inhibits the nicking-closing activity on the subunit of DNA gyrase that releases the positive binding stress on the supercoiled DNA.
Adverse effects
Hives, rash, intense itching, or fainting soon after a dose may be a sign of anaphylaxis. Common adverse effects include rash, itchy skin, blurred or double vision, halos around lights, changes in color vision, nausea, vomiting, and diarrhea. Nalidixic acid may also cause convulsions and hyperglycemia,[5] photosensitivity reactions,[6] and sometimes haemolytic anaemia,[7][8] thrombocytopenia[9] or leukopenia. Particularly in infants and young children, has been reported occasionally increased intracranial pressure.[10][11][12]
Overdose
In case of overdose the patient experiences headache, visual disturbances, balance disorders, mental confusion, metabolic acidosis and seizures.[13]
Spectrum of bacterial susceptibility and resistance
Aeromonas hydrophila, Clostridium and Haemophilus are generally susceptible to nalidixic acid, while other bacteria such as Bifidobacteria, Lactobacillus, Pseudomonas and Staphylococcus are resistant.[14] Salmonella enterica serovar Typhimurium strain ATCC14028 acquires nalidixic acid resistance when gyrB gene is mutated (strain IR715).[15]
See also
References
- ↑ "The quinolones: decades of development and use". The Journal of Antimicrobial Chemotherapy 51 (Suppl 1): 13–20. May 2003. doi:10.1093/jac/dkg208. PMID 12702699.
- ↑ "1,8-Naphthyridine Derivatives. A New Class of Chemotherapeutic Agents". Journal of Medicinal and Pharmaceutical Chemistry 5 (5): 1063–1065. September 1962. doi:10.1021/jm01240a021. PMID 14056431.
- ↑ "Disabling and potentially permanent side effects lead to suspension or restrictions of quinolone and fluoroquinolone antibiotics". 11 March 2019. https://www.ema.europa.eu/en/medicines/human/referrals/quinolone-fluoroquinolone-containing-medicinal-products.
- ↑ "DNA topoisomerases and their poisoning by anticancer and antibacterial drugs". Chemistry & Biology 17 (5): 421–433. May 2010. doi:10.1016/j.chembiol.2010.04.012. PMID 20534341.
- ↑ "Convulsions and hyperglycaemia associated with nalidixic acid". British Medical Journal 2 (6101): 1518. December 1977. doi:10.1136/bmj.2.6101.1518. PMID 589309.
- ↑ "Photosensitivity from nalidixic acid". Proceedings of the Royal Society of Medicine 66 (8): 747. August 1973. doi:10.1177/003591577306600805. PMID 4733958.
- ↑ "Haemolytic anaemia with nalidixic acid". British Medical Journal 4 (5838): 493. November 1972. doi:10.1136/bmj.4.5838.493-a. PMID 4653901.
- ↑ "Fatal acute immune haemolytic anaemia caused by nalidixic acid". British Medical Journal 285 (6346): 936–937. October 1982. doi:10.1136/bmj.285.6346.936-a. PMID 6811074.
- ↑ "Thrombocytopenia induced by nalidixic acid". British Medical Journal 289 (6450): 962. October 1984. doi:10.1136/bmj.289.6450.962. PMID 6435742.
- ↑ "Intracranial hypertension in a child during treatment with nalidixic acid". British Medical Journal 2 (5554): 744–745. June 1967. doi:10.1136/bmj.2.5554.744. PMID 6025983.
- ↑ "Nalidixic acid and intracranial hypertension". British Medical Journal 4 (5577): 488. November 1967. doi:10.1136/bmj.4.5577.488-a. PMID 6055749.
- ↑ "Acute intracranial hypertension after nalidixic acid administration". Archives of Disease in Childhood 49 (9): 743. September 1974. doi:10.1136/adc.49.9.743. PMID 4419059.
- ↑ "Nalidixic acid overdose and metabolic acidosis". CJEM 8 (2): 78. March 2006. doi:10.1017/s148180350001349x. PMID 17175866.
- ↑ "Nalidixic acid spectrum of bacterial susceptibility and Resistance". Toku-E. 2011-09-14. http://www.toku-e.com/Upload/Products/PDS/20120522005430.pdf.
- ↑ "Ethanolamine utilization in Salmonella typhimurium: nucleotide sequence, protein expression, and mutational analysis of the cchA cchB eutE eutJ eutG eutH gene cluster". Journal of Bacteriology 177 (5): 1357–66. March 1995. doi:10.1128/jb.177.5.1357-1366.1995. PMID 7868611.
External links
- "Nalidixic acid". HealthDigest.org. http://www.healthdigest.org/topics/category/1464-nalidixic-acid-dosage-interactions-side-effects-how-to-use.
 |

