Medicine:Systemic lupus erythematosus
| Systemic lupus erythematosus | |
|---|---|
| Other names | Lupus |
 | |
| Young woman with the typical "butterfly rash" found in lupus | |
| Pronunciation | |
| Specialty | Rheumatology |
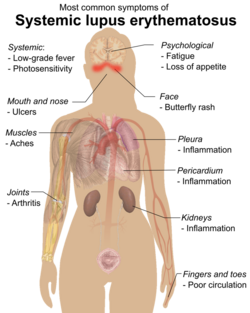
| Symptoms | Painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, red rash[1] |
| Usual onset | 15–45 years of age[1][2] |
| Duration | Long term[1] |
| Causes | Unclear[1] |
| Diagnostic method | Based on symptoms and blood tests[1] |
| Medication | NSAIDs, corticosteroids, immunosuppressants, hydroxychloroquine, methotrexate[1] |
| Prognosis | 15 year survival ~80%[3] |
| Frequency | 2–7 per 10,000[2] |
Systemic lupus erythematosus (SLE), also known simply as lupus, is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body.[1] Symptoms vary between people and may be mild to severe.[1] Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face.[1] Often there are periods of illness, called flares, and periods of remission during which there are few symptoms.[1]
The cause of SLE is not clear.[1] It is thought to involve genetics together with environmental factors.[4] Among identical twins, if one is affected there is a 24% chance the other one will be as well.[1] Female sex hormones, sunlight, smoking, vitamin D deficiency, and certain infections, are also believed to increase the risk.[4] The mechanism involves an immune response by autoantibodies against a person's own tissues.[1] These are most commonly anti-nuclear antibodies and they result in inflammation.[1] Diagnosis can be difficult and is based on a combination of symptoms and laboratory tests.[1] There are a number of other kinds of lupus erythematosus including discoid lupus erythematosus, neonatal lupus, and subacute cutaneous lupus erythematosus.[1]
There is no cure for SLE.[1] Treatments may include NSAIDs, corticosteroids, immunosuppressants, hydroxychloroquine, and methotrexate.[1] Although corticosteroids are rapidly effective, long term use results in side effects.[5] Alternative medicine has not been shown to affect the disease.[1] Life expectancy is lower among people with SLE.[6] SLE significantly increases the risk of cardiovascular disease with this being the most common cause of death.[4] With modern treatment about 80% of those affected survive more than 15 years.[3] Women with lupus have pregnancies that are higher risk but are mostly successful.[1]
Rate of SLE varies between countries from 20 to 70 per 100,000.[2] Women of childbearing age are affected about nine times more often than men.[4] While it most commonly begins between the ages of 15 and 45, a wide range of ages can be affected.[1][2] Those of African, Caribbean, and Chinese descent are at higher risk than white people.[4][2] Rates of disease in the developing world are unclear.[7] Lupus is Latin for "wolf": the disease was so-named in the 13th century as the rash was thought to appear like a wolf's bite.[8]
Signs and symptoms
SLE is one of several diseases known as "the great imitator" because it often mimics or is mistaken for other illnesses.[10] SLE is a classical item in differential diagnosis,[11] because SLE symptoms vary widely and come and go unpredictably. Diagnosis can thus be elusive, with some people having unexplained symptoms of SLE for years.
Common initial and chronic complaints include fever, malaise, joint pains, muscle pains, and fatigue. Because these symptoms are so often seen in association with other diseases, these signs and symptoms are not part of the diagnostic criteria for SLE. When occurring in conjunction with other signs and symptoms, however, they are considered suggestive.[12]
While SLE can occur in both males and females, it is found far more often in women, and the symptoms associated with each sex are different.[6] Females tend to have a greater number of relapses, a low white blood cell count, more arthritis, Raynaud's phenomenon, and psychiatric symptoms. Males tend to have more seizures, kidney disease, serositis (inflammation of tissues lining the lungs and heart), skin problems, and peripheral neuropathy.[13]
Skin
As many as 70% of people with lupus have some skin symptoms. The three main categories of lesions are chronic cutaneous (discoid) lupus, subacute cutaneous lupus, and acute cutaneous lupus. People with discoid lupus may exhibit thick, red scaly patches on the skin. Similarly, subacute cutaneous lupus manifests as red, scaly patches of skin but with distinct edges. Acute cutaneous lupus manifests as a rash. Some have the classic malar rash (or butterfly rash) associated with the disease.[14] This rash occurs in 30 to 60% of people with SLE.[15]
Hair loss, mouth and nasal ulcers, and lesions on the skin are other possible manifestations.[16]
Muscles and bones
The most commonly sought medical attention is for joint pain, with the small joints of the hand and wrist usually affected, although all joints are at risk. More than 90 percent of those affected will experience joint or muscle pain at some time during the course of their illness.[17] Unlike rheumatoid arthritis, lupus arthritis is less disabling and usually does not cause severe destruction of the joints. Fewer than ten percent of people with lupus arthritis will develop deformities of the hands and feet.[17] People with SLE are at particular risk of developing osteoarticular tuberculosis.[18]
A possible association between rheumatoid arthritis and SLE has been suggested,[19] and SLE may be associated with an increased risk of bone fractures in relatively young women.[20]
Blood
Anemia is common in children with SLE[21] and develops in about 50% of cases.[22] Low platelet count and white blood cell count may be due to the disease or a side effect of pharmacological treatment. People with SLE may have an association with antiphospholipid antibody syndrome[23] (a thrombotic disorder), wherein autoantibodies to phospholipids are present in their serum. Abnormalities associated with antiphospholipid antibody syndrome include a paradoxical prolonged partial thromboplastin time (which usually occurs in hemorrhagic disorders) and a positive test for antiphospholipid antibodies; the combination of such findings have earned the term "lupus anticoagulant-positive". Another autoantibody finding in SLE is the anti-cardiolipin antibody, which can cause a false positive test for syphilis.[citation needed]
Heart
SLE may cause pericarditis—inflammation of the outer lining surrounding the heart, myocarditis—inflammation of the heart muscle, or endocarditis—inflammation of the inner lining of the heart. The endocarditis of SLE is non-infectious, and is also called (Libman–Sacks endocarditis). It involves either the mitral valve or the tricuspid valve. Atherosclerosis also occurs more often and advances more rapidly than in the general population.[24][25]
Lungs
SLE can cause pleuritic pain as well as inflammation of the pleurae known as pleurisy, which can rarely give rise to shrinking lung syndrome involving a reduced lung volume.[26][27] Other associated lung conditions include pneumonitis, chronic diffuse interstitial lung disease, pulmonary hypertension, pulmonary emboli, and pulmonary hemorrhage.
Kidneys
Painless passage of blood or protein in the urine may often be the only presenting sign of kidney involvement. Acute or chronic renal impairment may develop with lupus nephritis, leading to acute or end-stage kidney failure. Because of early recognition and management of SLE, end-stage renal failure occurs in less than 5%[28][29] of cases; except in the black population, where the risk is many times higher.
The histological hallmark of SLE is membranous glomerulonephritis with "wire loop" abnormalities.[30] This finding is due to immune complex deposition along the glomerular basement membrane, leading to a typical granular appearance in immunofluorescence testing.
Neuropsychiatric
Neuropsychiatric syndromes can result when SLE affects the central or peripheral nervous system. The American College of Rheumatology defines 19 neuropsychiatric syndromes in systemic lupus erythematosus.[31] The diagnosis of neuropsychiatric syndromes concurrent with SLE (now termed as NPSLE),[32] is one of the most difficult challenges in medicine, because it can involve so many different patterns of symptoms, some of which may be mistaken for signs of infectious disease or stroke.[33]
A common neurological disorder people with SLE have is headache,[34] although the existence of a specific lupus headache and the optimal approach to headache in SLE cases remains controversial.[35] Other common neuropsychiatric manifestations of SLE include cognitive dysfunction, mood disorder, cerebrovascular disease,[34] seizures, polyneuropathy,[34] anxiety disorder, psychosis, depression, and in some extreme cases, personality disorders.[36] Steroid psychosis can also occur as a result of treating the disease.[32] It can rarely present with intracranial hypertension syndrome, characterized by an elevated intracranial pressure, papilledema, and headache with occasional abducens nerve paresis, absence of a space-occupying lesion or ventricular enlargement, and normal cerebrospinal fluid chemical and hematological constituents.[37]
More rare manifestations are acute confusional state, Guillain–Barré syndrome, aseptic meningitis, autonomic disorder, demyelinating syndrome, mononeuropathy (which might manifest as mononeuritis multiplex), movement disorder (more specifically, chorea), myasthenia gravis, myelopathy, cranial neuropathy and plexopathy.
Neurological disorders contribute to a significant percentage of morbidity and mortality in people with lupus.[38] As a result, the neural side of lupus is being studied in hopes of reducing morbidity and mortality rates.[31] One aspect of this disease is severe damage to the epithelial cells of the blood–brain barrier. In certain regions, depression affects up to 60% of women with SLE.[39]
Eyes
Eye involvement is seen in up to one-third of people. The most common diseases are dry eye syndrome and secondary Sjögren's syndrome, but episcleritis, scleritis, retinopathy (more often affecting both eyes than one), ischemic optic neuropathy, retinal detachment, and secondary angle-closure glaucoma may occur. In addition, the medications used to treat SLE can cause eye disease: long-term glucocorticoid use can cause cataracts and secondary open-angle glaucoma, and long-term hydroxychloroquine treatment can cause vortex keratopathy and maculopathy.[40]
Reproductive
While most pregnancies have positive outcomes there is a greater risk of adverse events occurring during pregnancy.[41] SLE causes an increased rate of fetal death in utero and spontaneous abortion (miscarriage). The overall live-birth rate in people with SLE has been estimated to be 72%.[42] Pregnancy outcome appears to be worse in people with SLE whose disease flares up during pregnancy.[43]
Neonatal lupus is the occurrence of SLE symptoms in an infant born from a mother with SLE, most commonly presenting with a rash resembling discoid lupus erythematosus, and sometimes with systemic abnormalities such as heart block or enlargement of the liver and spleen.[44] Neonatal lupus is usually benign and self-limited.[44]
Systemic
Fatigue in SLE is probably multifactorial and has been related to not only disease activity or complications such as anemia or hypothyroidism, but also to pain, depression, poor sleep quality, poor physical fitness and lack of social support.[45][46]
Causes
SLE is presumably caused by a genetic susceptibility coupled with an environmental trigger which results in defects in the immune system. One of the factors associated with SLE is vitamin D deficiency.[47]
Genetics
SLE does run in families, but no single causal gene has been identified. Instead, multiple genes appear to influence a person's chance of developing lupus when triggered by environmental factors. HLA class I, class II, and class III genes are associated with SLE, but only classes I and II contribute independently to increased risk of SLE.[48] Other genes which contain risk variants for SLE are IRF5, PTPN22, STAT4,[49] CDKN1A,[50] ITGAM, BLK,[49] TNFSF4 and BANK1.[51] Some of the susceptibility genes may be population specific.[49] Genetic studies of the rates of disease in families supports the genetic basis of this disease with a heritability of >66%.[52] Identical (monozygotic) twins were found to share susceptibility to the disease at >35% rate compared to fraternal (dizygotic) twins and other full siblings who only showed a 2–5% concordance in shared inheritance.[52]
Since SLE is associated with many genetic regions, it is likely an oligogenic trait, meaning that there are several genes that control susceptibility to the disease.[53]
SLE is regarded as a prototype disease due to the significant overlap in its symptoms with other autoimmune diseases.[54]
Drug reactions
Drug-induced lupus erythematosus is a (generally) reversible condition that usually occurs in people being treated for a long-term illness. Drug-induced lupus mimics SLE. However, symptoms of drug-induced lupus generally disappear once the medication that triggered the episode is stopped. More than 38 medications can cause this condition, the most common of which are procainamide, isoniazid, hydralazine, quinidine, and phenytoin.[55][11]
Non-systemic forms of lupus
Discoid (cutaneous) lupus is limited to skin symptoms and is diagnosed by biopsy of rash on the face, neck, scalp or arms. Approximately 5% of people with DLE progress to SLE.[56]
Pathophysiology
SLE is triggered by environmental factors that are unknown. In SLE, the body's immune system produces antibodies against itself, particularly against proteins in the cell nucleus. These antibody attacks are the immediate cause of SLE.[11][57][58]
SLE is a chronic inflammatory disease believed to be a type III hypersensitivity response with potential type II involvement.[59] Reticulate and stellate acral pigmentation should be considered a possible manifestation of SLE and high titers of anti-cardiolipin antibodies, or a consequence of therapy.[60]
People with SLE have intense polyclonal B-cell activation, with a population shift towards immature B cells. Memory B cells with increased CD27+/IgD—are less susceptible to immunosuppression. CD27-/IgD- memory B cells are associated with increased disease activity and renal lupus. T cells, which regulate B-cell responses and infiltrate target tissues, have defects in signaling, adhesion, co-stimulation, gene transcription, and alternative splicing. The cytokines B-lymphocyte stimulator (BLys), interleukin 6, interleukin 17, interleukin 18, type I interferons, and tumor necrosis factor α (TNFα) are involved in the inflammatory process and are potential therapeutic targets.[4][61][62]
In the complement system low C3 levels are associated with systemic lupus erythematosus[63]
Cell death signaling
- Apoptosis is increased in monocytes and keratinocytes
- Expression of Fas by B cells and T cells is increased
- There are correlations between the apoptotic rates of lymphocytes and disease activity.
- Necrosis is increased in T lymphocytes.
Tingible body macrophages (TBMs) – large phagocytic cells in the germinal centers of secondary lymph nodes – express CD68 protein. These cells normally engulf B cells that have undergone apoptosis after somatic hypermutation. In some people with SLE, significantly fewer TBMs can be found, and these cells rarely contain material from apoptotic B cells. Also, uningested apoptotic nuclei can be found outside of TBMs. This material may present a threat to the tolerization of B cells and T cells. Dendritic cells in the germinal center may endocytose such antigenic material and present it to T cells, activating them. Also, apoptotic chromatin and nuclei may attach to the surfaces of follicular dendritic cells and make this material available for activating other B cells that may have randomly acquired self-specificity through somatic hypermutation.[64] Necrosis, a pro-inflammatory form of cell death, is increased in T lymphocytes, due to mitochondrial dysfunction, oxidative stress, and depletion of ATP.[65]
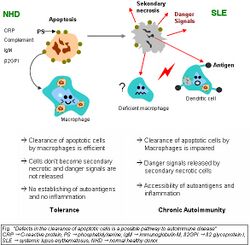
Clearance deficiency
Impaired clearance of dying cells is a potential pathway for the development of this systemic autoimmune disease. This includes deficient phagocytic activity and scant serum components in addition to increased apoptosis.
SLE is associated with defects in apoptotic clearance, and the damaging effects caused by apoptotic debris. Early apoptotic cells express “eat-me” signals, of cell-surface proteins such as phosphatidylserine, that prompt immune cells to engulf them. Apoptotic cells also express “find-me” signals, to attract macrophages and dendritic cells. When apoptotic material is not removed correctly by phagocytes, they are captured instead by antigen-presenting cells, which leads to development of antinuclear antibodies.[4]
Monocytes isolated from whole blood of people with SLE show reduced expression of CD44 surface molecules involved in the uptake of apoptotic cells. Most of the monocytes and tingible body macrophages (TBMs), which are found in the germinal centres of lymph nodes, even show a definitely different morphology; they are smaller or scarce and die earlier. Serum components like complement factors, CRP, and some glycoproteins are, furthermore, decisively important for an efficiently operating phagocytosis. With SLE, these components are often missing, diminished, or inefficient.
Recent research has found an association between certain people with lupus (especially those with lupus nephritis) and an impairment in degrading neutrophil extracellular traps (NETs). These were due to DNAse1 inhibiting factors, or NET protecting factors in people's serum, rather than abnormalities in the DNAse1 itself.[66] DNAse1 mutations in lupus have so far only been found in some Japanese cohorts.[67]
The clearance of early apoptotic cells is an important function in multicellular organisms. It leads to a progression of the apoptosis process and finally to secondary necrosis of the cells if this ability is disturbed. Necrotic cells release nuclear fragments as potential autoantigens, as well as internal danger signals, inducing maturation of dendritic cells (DCs), since they have lost their membranes' integrity. Increased appearance of apoptotic cells also stimulates inefficient clearance. That leads to maturation of DCs and also to the presentation of intracellular antigens of late apoptotic or secondary necrotic cells, via MHC molecules. Autoimmunity possibly results by the extended exposure to nuclear and intracellular autoantigens derived from late apoptotic and secondary necrotic cells. B and T cell tolerance for apoptotic cells is abrogated, and the lymphocytes get activated by these autoantigens; inflammation and the production of autoantibodies by plasma cells is initiated. A clearance deficiency in the skin for apoptotic cells has also been observed in people with cutaneous lupus erythematosus (CLE).[68]
Germinal centers

In healthy conditions, apoptotic lymphocytes are removed in germinal centers (GC) by specialized phagocytes, the tingible body macrophages (TBM), which is why no free apoptotic and potential autoantigenic material can be seen. In some people with SLE, buildup of apoptotic debris can be observed in GC because of an ineffective clearance of apoptotic cells. In close proximity to TBM, follicular dendritic cells (FDC) are localised in GC, which attach antigen material to their surface and, in contrast to bone marrow-derived DC, neither take it up nor present it via MHC molecules.
Autoreactive B cells can accidentally emerge during somatic hypermutation and migrate into the germinal center light zone. Autoreactive B cells, maturated coincidentally, normally do not receive survival signals by antigen planted on follicular dendritic cells and perish by apoptosis. In the case of clearance deficiency, apoptotic nuclear debris accumulates in the light zone of GC and gets attached to FDC. This serves as a germinal centre survival signal for autoreactive B-cells. After migration into the mantle zone, autoreactive B cells require further survival signals from autoreactive helper T cells, which promote the maturation of autoantibody-producing plasma cells and B memory cells. In the presence of autoreactive T cells, a chronic autoimmune disease may be the consequence.
Anti-nRNP autoimmunity
Anti-nRNP autoantibodies to nRNP A and nRNP C initially targeted restricted, proline-rich motifs. Antibody binding subsequently spread to other epitopes. The similarity and cross-reactivity between the initial targets of nRNP and Sm autoantibodies identifies a likely commonality in cause and a focal point for intermolecular epitope spreading.[69]
Others
Elevated expression of HMGB1 was found in the sera of people and mice with systemic lupus erythematosus, high mobility group box 1 (HMGB1) is a nuclear protein participating in chromatin architecture and transcriptional regulation. Recently, there is increasing evidence HMGB1 contributes to the pathogenesis of chronic inflammatory and autoimmune diseases due to its inflammatory and immune stimulating properties.[70]
Diagnosis


Laboratory tests
Antinuclear antibody (ANA) testing and anti-extractable nuclear antigen (anti-ENA) form the mainstay of serologic testing for SLE. If ANA is negative the disease can be ruled out.[71]
Several techniques are used to detect ANAs. The most widely used is indirect immunofluorescence (IF). The pattern of fluorescence suggests the type of antibody present in the people's serum. Direct immunofluorescence can detect deposits of immunoglobulins and complement proteins in the people's skin. When skin not exposed to the sun is tested, a positive direct IF (the so-called lupus band test) is an evidence of systemic lupus erythematosus.[72]
ANA screening yields positive results in many connective tissue disorders and other autoimmune diseases, and may occur in normal individuals. Subtypes of antinuclear antibodies include anti-Smith and anti-double stranded DNA (dsDNA) antibodies (which are linked to SLE) and anti-histone antibodies (which are linked to drug-induced lupus). Anti-dsDNA antibodies are highly specific for SLE; they are present in 70% of cases, whereas they appear in only 0.5% of people without SLE.[11] The anti-dsDNA antibody titers also tend to reflect disease activity, although not in all cases.[11] Other ANA that may occur in people with SLE are anti-U1 RNP (which also appears in systemic sclerosis and mixed connective tissue disease), SS-A (or anti-Ro) and SS-B (or anti-La; both of which are more common in Sjögren's syndrome). SS-A and SS-B confer a specific risk for heart conduction block in neonatal lupus.[73]
Other tests routinely performed in suspected SLE are complement system levels (low levels suggest consumption by the immune system), electrolytes and kidney function (disturbed if the kidney is involved), liver enzymes, and complete blood count.
The lupus erythematosus (LE) cell test was commonly used for diagnosis, but it is no longer used because the LE cells are only found in 50–75% of SLE cases, and they are also found in some people with rheumatoid arthritis, scleroderma, and drug sensitivities. Because of this, the LE cell test is now performed only rarely and is mostly of historical significance.[74]
Diagnostic criteria
Some physicians make a diagnosis on the basis of the American College of Rheumatology (ACR) classification criteria. The criteria, however, were established mainly for use in scientific research including use in randomized controlled trials which require higher confidence levels, so many people with SLE may not pass the full criteria.
Criteria
The American College of Rheumatology (ACR) established eleven criteria in 1982,[75] which were revised in 1997[76] as a classificatory instrument to operationalise the definition of SLE in clinical trials. They were not intended to be used to diagnose individuals and do not do well in that capacity. For the purpose of identifying people for clinical studies, a person has SLE if any 4 out of 11 symptoms are present simultaneously or serially on two separate occasions.
- Malar rash (rash on cheeks); sensitivity = 57%; specificity = 96%.[77]
- Discoid rash (red, scaly patches on skin that cause scarring); sensitivity = 18%; specificity = 99%.[77]
- Serositis: Pleurisy (inflammation of the membrane around the lungs) or pericarditis (inflammation of the membrane around the heart); sensitivity = 56%; specificity = 86% (pleural is more sensitive; cardiac is more specific).[77]
- Oral ulcers (includes oral or nasopharyngeal ulcers); sensitivity = 27%; specificity = 96%.[77]
- Arthritis: nonerosive arthritis of two or more peripheral joints, with tenderness, swelling, or effusion; sensitivity = 86%; specificity = 37%.[77]
- Photosensitivity (exposure to ultraviolet light causes rash, or other symptoms of SLE flareups); sensitivity = 43%; specificity = 96%.[77]
- Blood—hematologic disorder—hemolytic anemia (low red blood cell count), leukopenia (white blood cell count<4000/µl), lymphopenia (<1500/µl), or low platelet count (<100000/µl) in the absence of offending drug; sensitivity = 59%; specificity = 89%.[77] Hypocomplementemia is also seen, due to either consumption of C3[78] and C4 by immune complex-induced inflammation or to congenitally complement deficiency, which may predispose to SLE.
- Renal disorder: More than 0.5 g per day protein in urine or cellular casts seen in urine under a microscope; sensitivity = 51%; specificity = 94%.[77]
- Antinuclear antibody test positive; sensitivity = 99%; specificity = 49%.[77]
- Immunologic disorder: Positive anti-Smith, anti-ds DNA, antiphospholipid antibody, or false positive serological test for syphilis; sensitivity = 85%; specificity = 93%.[77] Presence of anti-ss DNA in 70% of cases (though also positive with rheumatic disease and healthy persons).[79]
- Neurologic disorder: Seizures or psychosis; sensitivity = 20%; specificity = 98%.[77]
Other than the ACR criteria, people with lupus may also have:[80]
- fever (over 100 °F/ 37.7 °C)
- extreme fatigue
- hair loss
- fingers turning white or blue when cold (Raynaud's phenomenon)
Criteria for individual diagnosis
Some people, especially those with antiphospholipid syndrome, may have SLE without four of the above criteria, and also SLE may present with features other than those listed in the criteria.[81][82][83]
Recursive partitioning has been used to identify more parsimonious criteria.[77] This analysis presented two diagnostic classification trees:
- Simplest classification tree: SLE is diagnosed if a person has an immunologic disorder (anti-DNA antibody, anti-Smith antibody, false positive syphilis test, or LE cells) or malar rash. It has sensitivity = 92% and specificity = 92%.
- Full classification tree: Uses 6 criteria. It has sensitivity = 97% and specificity = 95%.
Other alternative criteria have been suggested, e.g. the St. Thomas' Hospital "alternative" criteria in 1998.[84]
Treatment
The treatment of SLE involves preventing flares and reducing their severity and duration when they occur.
Treatment can include corticosteroids and anti-malarial drugs. Certain types of lupus nephritis such as diffuse proliferative glomerulonephritis require intermittent cytotoxic drugs. These drugs include cyclophosphamide and mycophenolate. Cyclophosphamide increases the risk of developing infections, pancreas problems, high blood sugar, and high blood pressure.[85]
Hydroxychloroquine was approved by the FDA for lupus in 1955.[86] Some drugs approved for other diseases are used for SLE 'off-label'. In November 2010, an FDA advisory panel recommended approving belimumab (Benlysta) as a treatment for the pain and flare-ups common in lupus. The drug was approved by the FDA in March 2011.[87][88]
Medications
Due to the variety of symptoms and organ system involvement with SLE, its severity in an individual must be assessed in order to successfully treat SLE. Mild or remittent disease may, sometimes, be safely left untreated. If required, nonsteroidal anti-inflammatory drugs and antimalarials may be used. Medications such as prednisone, mycophenolic acid and tacrolimus have been used in the past.
Disease-modifying antirheumatic drugs
Disease-modifying antirheumatic drugs (DMARDs) are used preventively to reduce the incidence of flares, the progress of the disease, and the need for steroid use; when flares occur, they are treated with corticosteroids. DMARDs commonly in use are antimalarials such as hydroxychloroquine and immunosuppressants (e.g. methotrexate and azathioprine). Hydroxychloroquine is an FDA-approved antimalarial used for constitutional, cutaneous, and articular manifestations. Hydroxychloroquine has relatively few side effects, and there is evidence that it improves survival among people who have SLE.[86] Cyclophosphamide is used for severe glomerulonephritis or other organ-damaging complications. Mycophenolic acid is also used for treatment of lupus nephritis, but it is not FDA-approved for this indication, and FDA is investigating reports that it may be associated with birth defects when used by pregnant women.[89]
Immunosuppressive drugs
In more severe cases, medications that modulate the immune system (primarily corticosteroids and immunosuppressants) are used to control the disease and prevent recurrence of symptoms (known as flares). Depending on the dosage, people who require steroids may develop Cushing's syndrome, symptoms of which may include obesity, puffy round face, diabetes mellitus, increased appetite, difficulty sleeping and osteoporosis. These may subside if and when the large initial dosage is reduced, but long-term use of even low doses can cause elevated blood pressure and cataracts.
Numerous new immunosuppressive drugs are being actively tested for SLE. Rather than suppressing the immune system nonspecifically, as corticosteroids do, they target the responses of individual [types of] immune cells. Some of these drugs are already FDA-approved for treatment of rheumatoid arthritis, however due to high-toxicity, its use is limited.[86][90]
Analgesia
Since a large percentage of people with SLE have varying amounts of chronic pain, stronger prescription analgesics (painkillers) may be used if over-the-counter drugs (mainly nonsteroidal anti-inflammatory drugs) do not provide effective relief. Potent NSAIDs such as indomethacin and diclofenac are relatively contraindicated for people with SLE because they increase the risk of kidney failure and heart failure.[86]
Pain is typically treated with opioids, varying in potency based on the severity of symptoms. When opioids are used for prolonged periods, drug tolerance, chemical dependency, and addiction may occur. Opiate addiction is not typically a concern since the condition is not likely to ever completely disappear. Thus, lifelong treatment with opioids is fairly common for chronic pain symptoms, accompanied by periodic titration that is typical of any long-term opioid regimen.
Intravenous immunoglobulins (IVIGs)
Intravenous immunoglobulins may be used to control SLE with organ involvement, or vasculitis. It is believed that they reduce antibody production or promote the clearance of immune complexes from the body, even though their mechanism of action is not well understood.[91] Unlike immunosuppressives and corticosteroids, IVIGs do not suppress the immune system, so there is less risk of serious infections with these drugs.[92]
Lifestyle changes
Avoiding sunlight in SLE is critical, since sunlight is known to exacerbate skin manifestations of the disease. Avoiding activities which induce fatigue is also important, since those with SLE fatigue easily and it can be debilitating. These two problems can lead to people becoming housebound for long periods of time. Drugs unrelated to SLE should be prescribed only when known not to exacerbate the disease. Occupational exposure to silica, pesticides, and mercury can also worsen the disease.[61]
Kidney transplantation
Kidney transplants are the treatment of choice for end-stage kidney disease, which is one of the complications of lupus nephritis, but the recurrence of the full disease is common in up to 30% of people.[93]
Antiphospholipid syndrome
Approximately 20% of people with SLE have clinically significant levels of antiphospholipid antibodies, which are associated with antiphospholipid syndrome.[94] Antiphospholipid syndrome is also related to the onset of neural lupus symptoms in the brain. In this form of the disease the cause is very different from lupus: thromboses (blood clots or "sticky blood") form in blood vessels, which prove to be fatal if they move within the blood stream.[81] If the thromboses migrate to the brain, they can potentially cause a stroke by blocking the blood supply to the brain.
If this disorder is suspected in people, brain scans are usually required for early detection. These scans can show localized areas of the brain where blood supply has not been adequate. The treatment plan for these people requires anticoagulation. Often, low-dose aspirin is prescribed for this purpose, although for cases involving thrombosis anticoagulants such as warfarin are used.[95]
Management of pregnancy
While most infants born to mothers who have SLE are healthy, pregnant mothers with SLE should remain under medical care until delivery. Neonatal lupus is rare, but identification of mothers at highest risk for complications allows for prompt treatment before or after birth. In addition, SLE can flare up during pregnancy, and proper treatment can maintain the health of the mother longer. Women pregnant and known to have anti-Ro (SSA) or anti-La antibodies (SSB) often have echocardiograms during the 16th and 30th weeks of pregnancy to monitor the health of the heart and surrounding vasculature.[96]
Contraception and other reliable forms of pregnancy prevention is routinely advised for women with SLE, since getting pregnant during active disease was found to be harmful. Lupus nephritis was the most common manifestation.
Prognosis
No cure is available for SLE but there are many treatments for the disease.[1]
In the 1950s, most people diagnosed with SLE lived fewer than five years. Today, over 90% now survive for more than ten years, and many live relatively symptom-free. 80–90% can expect to live a normal lifespan.[97] Mortality rates are however elevated compared to people without SLE.[98]
Prognosis is typically worse for men and children than for women; however, if symptoms are present after age 60, the disease tends to run a more benign course. Early mortality, within 5 years, is due to organ failure or overwhelming infections, both of which can be altered by early diagnosis and treatment. The mortality risk is fivefold when compared to the normal population in the late stages, which can be attributed to cardiovascular disease from accelerated atherosclerosis, the leading cause of death for people with SLE.[86] To reduce the potential for cardiovascular issues, high blood pressure and high cholesterol should be prevented or treated aggressively. Steroids should be used at the lowest dose for the shortest possible period, and other drugs that can reduce symptoms should be used whenever possible.[86]
Epidemiology
The global rates of SLE are approximately 20–70 per 100,000 people. In females, the rate is highest between 45 and 64 years of age. The lowest overall rate exists in Iceland and Japan. The highest rates exist in the US and France. However, there is not sufficient evidence to conclude why SLE is less common in some countries compared to others; it could be the environmental variability in these countries. For example, different countries receive different levels of sunlight, and exposure to UV rays affects dermatological symptoms of SLE. Certain studies hypothesize that a genetic connection exists between race and lupus which affects disease prevalence. If this is true, the racial composition of countries affects disease, and will cause the incidence in a country to change as the racial makeup changes. In order to understand if this is true, countries with largely homogenous and racially stable populations should be studied to better understand incidence.[2] Rates of disease in the developing world are unclear.[7]
The rate of SLE varies between countries, ethnicity, and sex, and changes over time.[99] In the United States, one estimate of the rate of SLE is 53 per 100,000;[99] another estimate places the total affected population at 322,000 to over 1 million (98 to over 305 per 100,000).[100] In Northern Europe the rate is about 40 per 100,000 people.[101] SLE occurs more frequently and with greater severity among those of non-European descent.[100] That rate has been found to be as high as 159 per 100,000 among those of Afro-Caribbean descent.[99] Childhood-onset systemic lupus erythematosus generally presents between the ages of 3 and 15 and is four times more common in girls.[102]
While the onset and persistence of SLE can show disparities between genders, socioeconomic status also plays a major role. Women with SLE and of lower socioeconomic status have been shown to have higher depression scores, higher body mass index, and more restricted access to medical care than women of higher socioeconomic statuses with the illness. People with SLE had more self-reported anxiety and depression scores if they were from a lower socioeconomic status.[103]
Ethnicity
There are assertions that race affects the rate of SLE. However, a 2010 review of studies which correlate race and SLE identified several sources of systematic and methodological error, indicating that the connection between race and SLE may be spurious.[104] For example, studies show that social support is a modulating factor which buffers against SLE-related damage and maintains physiological functionality.[104] Studies have not been conducted to determine whether people of different racial backgrounds receive differing levels of social support.[104] If there is a difference, this could act as a confounding variable in studies correlating race and SLE. Another caveat to note when examining studies about SLE is that symptoms are often self-reported. This process introduces additional sources of methodological error. Studies have shown that self-reported data is affected by more than just the patients experience with the disease- social support, the level of helplessness, and abnormal illness-related behaviors also factor into a self-assessment. Additionally, other factors like the degree of social support that a person receives, socioeconomic status, health insurance, and access to care can contribute to an individual's disease progression.[104][105] Racial differences in lupus progression have not been found in studies that control for the socioeconomic status [SES] of participants.[104][106] Studies that control for the SES of its participants have found that non-white people have more abrupt disease onset compared to white people and that their disease progresses more quickly. Non-white patients often report more hematological, serosal, neurological, and renal symptoms. However, the severity of symptoms and mortality are both similar in white and non-white patients. Studies that report different rates of disease progression in late-stage SLE are most likely reflecting differences in socioeconomic status and the corresponding access to care.[104] The people who receive medical care have often accrued less disease-related damage and are less likely to be below the poverty line.[106] Additional studies have found that education, marital status, occupation, and income create a social context which contributes to disease progression.[104]
Sex
SLE, like many autoimmune diseases, affects females more frequently than males, at a rate of about 9 to 1.[6][99] The X chromosome carries immunological related genes, which can mutate and contribute to the onset of SLE. The Y chromosome has no identified mutations associated with autoimmune disease.[107]
Hormonal mechanisms could explain the increased incidence of SLE in females. The onset of SLE could be attributed to the elevated hydroxylation of estrogen and the abnormally decreased levels of androgens in females. In addition, differences in GnRH signalling have also shown to contribute to the onset of SLE. While females are more likely to relapse than males, the intensity of these relapses is the same for both sexes.[13]
In addition to hormonal mechanisms, specific genetic influences found on the X chromosome may also contribute to the development of SLE. Studies indicate that the X chromosome can determine the levels of sex hormones. A study has shown an association between Klinefelter syndrome and SLE. XXY males with SLE have an abnormal X–Y translocation resulting in the partial triplication of the PAR1 gene region.[108]
Changing rate of disease
The rate of SLE in the United States increased from 1.0 in 1955 to 7.6 in 1974. Whether the increase is due to better diagnosis or to increasing frequency of the disease is unknown.[99]
History

The history of SLE can be divided into three periods: classical, neoclassical, and modern. In each period, research and documentation advanced the understanding and diagnosis of SLE, leading to its classification as an autoimmune disease in 1851, and to the various diagnostic options and treatments now available to people with SLE. The advances made by medical science in the diagnosis and treatment of SLE have dramatically improved the life expectancy of a person diagnosed with SLE.[110]
Etymology
There are several explanations ventured for the term lupus erythematosus. Lupus is Latin for "wolf",[111][8] and "erythro" is derived from ερυθρός, Greek for "red." All explanations originate with the reddish, butterfly-shaped malar rash that the disease classically exhibits across the nose and cheeks.
- In various accounts, some doctors thought the rash resembled the pattern of fur on a wolf's face. More likely is that it is derived from the similarity in distribution to lupus vulgaris or chronic facial tuberculosis where the lesions are ragged and punched out and are said to resemble the bite of a wolf.
- Another account claims that the term "lupus" did not come from Latin directly, but from the term for a French style of mask that women reportedly wore to conceal the rash on their faces. The mask is called a "loup," French for "wolf."[citation needed]
Classical period
The classical period began when the disease was first recognized in the Middle Ages. The term lupus is attributed to 12th-century Italian physician Rogerius Frugard, who used it to describe ulcerating sores on the legs of people.[112] No formal treatment for the disease existed and the resources available to physicians to help people were limited.[113]
Neoclassical period
The neoclassical period began in 1851 when the skin disease which is now known as discoid lupus was documented by the French physician, Pierre Cazenave. Cazenave termed the illness lupus and added the word erythematosus to distinguish this disease from other illnesses that affected the skin except they were infectious.[114] Cazenave observed the disease in several people and made very detailed notes to assist others in its diagnosis. He was one of the first to document that lupus affected adults from adolescence into the early thirties and that the facial rash is its most distinguishing feature.[115]
Research and documentation of the disease continued in the neoclassical period with the work of Ferdinand von Hebra and his son-in-law, Moritz Kaposi. They documented the physical effects of lupus as well as some insights into the possibility that the disease caused internal trauma. Von Hebra observed that lupus symptoms could last many years and that the disease could go "dormant" after years of aggressive activity and then re-appear with symptoms following the same general pattern. These observations led Hebra to term lupus a chronic disease in 1872.[116]
Kaposi observed that lupus assumed two forms: the skin lesions (now known as discoid lupus) and a more aggravated form that affected not only the skin but also caused fever, arthritis, and other systemic disorders in people.[117] The latter also presented a rash confined to the face, appearing on the cheeks and across the bridge of the nose; he called this the "butterfly rash". Kaposi also observed those patients who developed the "butterfly rash" (or malar rash) often were afflicted with another disease such as tuberculosis, anemia, or chlorisis which often caused death.[115] Kaposi was one of the first people to recognize what is now termed systemic lupus erythematosus in his documentation of the remitting and relapsing nature of the disease and the relationship of skin and systemic manifestations during disease activity.[118]
The 19th century's research into lupus continued with the work of Sir William Osler who, in 1895, published the first of his three papers about the internal complications of erythema exudativum multiforme. Not all the patient cases in his paper had SLE but Osler's work expanded the knowledge of systemic diseases and documented extensive and critical visceral complications for several diseases including lupus.[115] Noting that many people with lupus had a disease that not only affected the skin but many other organs in the body as well, Osler added the word "systemic" to the term lupus erythematosus to distinguish this type of disease from discoid lupus erythematosus.[119] Osler's second paper noted that reoccurrence is a special feature of the disease and that attacks can be sustained for months or even years. Further study of the disease led to a third paper, published in 1903, documenting afflictions such as arthritis, pneumonia, the inability to form coherent ideas, delirium, and central nervous system damage as all affecting patients diagnosed with SLE.[115]
Modern period
The modern period, beginning in 1920, saw major developments in research into the cause and treatment of discoid and systemic lupus. Research conducted in the 1920s and 1930s led to the first detailed pathologic descriptions of lupus and demonstrated how the disease affected the kidney, heart, and lung tissue.[120] A major breakthrough was made in 1948 with the discovery of the LE cell (the lupus erythematosus cell—a misnomer, as it occurs with other diseases as well). Discovered by a team of researchers at the Mayo Clinic, they discovered that the white blood cells contained the nucleus of another cell that was pushing against the white's cell proper nucleus.[121] Noting that the invading nucleus was coated with antibody that allowed it to be ingested by a phagocytic or scavenger cell, they named the antibody that causes one cell to ingest another the LE factor and the two nuclei cell result in the LE cell.[122] The LE cell, it was determined, was a part of an anti-nuclear antibody (ANA) reaction; the body produces antibodies against its own tissue. This discovery led to one of the first definitive tests for lupus since LE cells are found in approximately 60% of all people diagnosed with lupus.[123] The LE cell test is rarely performed as a definitive lupus test today as LE cells do not always occur in people with SLE and can occur in individuals with other autoimmune diseases. Their presence can be helpful in establishing a diagnosis but no longer indicates a definitive SLE diagnosis.
The discovery of the LE cell led to further research and this resulted in more definitive tests for lupus. Building on the knowledge that those with SLE had auto-antibodies that would attach themselves to the nuclei of normal cells, causing the immune system to send white blood cells to fight off these "invaders", a test was developed to look for the anti-nuclear antibody (ANA) rather than the LE cell specifically. This ANA test was easier to perform and led not only to a definitive diagnosis of lupus but also many other related diseases. This discovery led to the understanding of what are now known as autoimmune diseases.[124]
To ensure that the person has lupus and not another autoimmune disease, the American College of Rheumatology (ACR) established a list of clinical and immunologic criteria that, in any combination, point to SLE. The criteria include symptoms that the person can identify (e.g. pain) and things that a physician can detect in a physical examination and through laboratory test results. The list was originally compiled in 1971, initially revised in 1982, and further revised and improved in 2009.[125]
Medical historians have theorized that people with porphyria (a disease that shares many symptoms with SLE) generated folklore stories of vampires and werewolves, due to the photosensitivity, scarring, hair growth, and porphyrin brownish-red stained teeth in severe recessive forms of porphyria (or combinations of the disorder, known as dual, homozygous, or compound heterozygous porphyrias).[126]
Useful medication for the disease was first found in 1894, when quinine was first reported as an effective therapy. Four years later, the use of salicylates in conjunction with quinine was noted to be of still greater benefit. This was the best available treatment until the middle of the twentieth century, when Hench discovered the efficacy of corticosteroids in the treatment of SLE.[126]
Research
A study called BLISS-76 tested the drug belimumab, a fully human monoclonal anti-BAFF (or anti-BLyS) antibody.[88] BAFF stimulates and extends the life of B lymphocytes, which produce antibodies against foreign and self cells.[127] It was approved by the FDA in March 2011.[87] Genetically engineered immune cells are also being studied in animal models of the disease as of 2019.[128]
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 "Handout on Health: Systemic Lupus Erythematosus". February 2015. Archived from the original on 17 June 2016. https://web.archive.org/web/20160617162703/http://www.niams.nih.gov/Health_Info/Lupus/default.asp. Retrieved 12 June 2016.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Danchenko, N.; Satia, J.A.; Anthony, M.S. (2006). "Epidemiology of systemic lupus erythematosus: a comparison of worldwide disease burden". Lupus 15 (5): 308–318. doi:10.1191/0961203306lu2305xx. PMID 16761508.
- ↑ 3.0 3.1 The Cleveland Clinic Intensive Review of Internal Medicine (5 ed.). Lippincott Williams & Wilkins. 2012. p. 969. ISBN 9781451153309. https://books.google.com/books?id=4LeX_5Vwy-4C&pg=PA969. Retrieved 13 June 2016.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Lisnevskaia, L; Murphy, G; Isenberg, D (22 November 2014). "Systemic lupus erythematosus.". Lancet 384 (9957): 1878–88. doi:10.1016/s0140-6736(14)60128-8. PMID 24881804.
- ↑ Davis, Laurie S.; Reimold, Andreas M. (April 2017). "Research and therapeutics—traditional and emerging therapies in systemic lupus erythematosus". Rheumatology 56 (suppl_1): i100–i113. doi:10.1093/rheumatology/kew417. PMID 28375452.
- ↑ 6.0 6.1 6.2 Murphy, G; Isenberg, D (December 2013). "Effect of gender on clinical presentation in systemic lupus erythematosus.". Rheumatology (Oxford, England) 52 (12): 2108–15. doi:10.1093/rheumatology/ket160. PMID 23641038.
- ↑ 7.0 7.1 Tiffin, N; Adeyemo, A; Okpechi, I (7 January 2013). "A diverse array of genetic factors contribute to the pathogenesis of systemic lupus erythematosus.". Orphanet Journal of Rare Diseases 8: 2. doi:10.1186/1750-1172-8-2. PMID 23289717.
- ↑ 8.0 8.1 Chabner, Davi-Ellen (2013). The Language of Medicine. Elsevier Health Sciences. p. 610. ISBN 978-1455728466. https://books.google.com/books?id=OUAD3KKPRwIC&pg=PA610.
- ↑ MedicineNet: Systemic Lupus (cont.) Last Editorial Review: 2009-01-30
- ↑ "Lupus, "The Great Imitator"". University Health Care. Archived from the original on January 15, 2009. https://web.archive.org/web/20090115100021/http://healthcare.utah.edu/healthtools/articles/lupus.html. Retrieved 2009-02-03.
- ↑ 11.0 11.1 11.2 11.3 11.4 Anisur Rahman; David A. Isenberg (February 28, 2008). "Review Article: Systemic Lupus Erythematosus". N Engl J Med 358 (9): 929–939. doi:10.1056/NEJMra071297. PMID 18305268.
- ↑ "Lupus: Symptoms — MayoClinic.com". Archived from the original on 2008-07-14. https://web.archive.org/web/20080714123532/http://www.mayoclinic.com/health/lupus/DS00115/DSECTION%3Dsymptoms. Retrieved 2008-07-14.
- ↑ 13.0 13.1 Yacoub Wasef, Sherif Z. (2004). "Gender differences in systemic lupus erythematosus". Gender Medicine 1 (1): 12–17. doi:10.1016/S1550-8579(04)80006-8. PMID 16115579.
- ↑ Tebbe, B; Orfanos, CE (1997). "Epidemiology and socioeconomic impact of skin disease in lupus erythematosus". Lupus 6 (2): 96–104. doi:10.1177/096120339700600204. PMID 9061657.
- ↑ Harris, Jeffrey P.; Weisman, Michael H., eds (2007). Head and neck manifestations of systemic disease. New York: Informa Healthcare. p. 6. ISBN 9781420017564. https://books.google.com/books?id=31yUl-V90XoC&pg=PA6.
- ↑ Gladman, Dafna (10 September 2015). "Overview of the clinical manifestations of systemic lupus erythematosus in adults". Archived from the original on 19 April 2017. https://web.archive.org/web/20170419003102/https://www.uptodate.com/contents/overview-of-the-clinical-manifestations-of-systemic-lupus-erythematosus-in-adults. Retrieved 18 April 2017.
- ↑ 17.0 17.1 Joint and Muscle Pain Lupus Foundation of America
- ↑ "Osteoarticular tuberculosis in patients with systemic lupus erythematosus". QJM 102 (5): 321–8. February 2009. doi:10.1093/qjmed/hcp015. PMID 19246552.
- ↑ "Familial associations of rheumatoid arthritis with autoimmune diseases and related conditions". Arthritis Rheum. 60 (3): 661–8. February 2009. doi:10.1002/art.24328. PMID 19248111.
- ↑ "Risk factors of vertebral fractures in women with systemic lupus erythematosus". Clin. Rheumatol. 28 (5): 579–85. February 2009. doi:10.1007/s10067-009-1105-3. PMID 19224131.
- ↑ Lam, SK; Quah, TC (1990). "Anemia in systemic lupus erythematosus.". The Journal of the Singapore Paediatric Society 32 (3–4): 132–6. PMID 2133750.
- ↑ Giannouli, S (1 February 2006). "Anaemia in systemic lupus erythematosus: from pathophysiology to clinical assessment". Annals of the Rheumatic Diseases 65 (2): 144–148. doi:10.1136/ard.2005.041673. PMID 16079164.
- ↑ "Association of antiphosphatidylserine/prothrombin antibodies with neuropsychiatric systemic lupus erythematosus". Clin. Rheumatol. 28 (7): 841–5. February 2009. doi:10.1007/s10067-009-1123-1. PMID 19224124.
- ↑ Bevra Hannahs Hahn, M.D. (December 2003). "Systemic lupus erythematosus and accelerated atherosclerosis". N Engl J Med 349 (25): 2379–80. doi:10.1056/NEJMp038168. PMID 14681501.
- ↑ Frieri, M; Stampfl, H (January 2016). "Systemic lupus erythematosus and atherosclerosis: Review of the literature.". Autoimmunity Reviews 15 (1): 16–21. doi:10.1016/j.autrev.2015.08.007. PMID 26299985.
- ↑ Henderson, LA; Loring, SH; Gill, RR; Liao, KP; Ishizawar, R; Kim, S; Perlmutter-Goldenson, R; Rothman, D et al. (March 2013). "Shrinking lung syndrome as a manifestation of pleuritis: a new model based on pulmonary physiological studies.". The Journal of Rheumatology 40 (3): 273–81. doi:10.3899/jrheum.121048. PMID 23378468.
- ↑ Calderaro, DC; Ferreira, GA (May 2012). "Presentation and prognosis of shrinking lung syndrome in systemic lupus erythematosus: report of four cases.". Rheumatology International 32 (5): 1391–6. doi:10.1007/s00296-011-1863-5. PMID 21431288.
- ↑ "Population-based incidence and prevalence of systemic lupus erythematosus: the Michigan Lupus Epidemiology and Surveillance program.". Arthritis Rheumatol 66 (2): 369–78. 2014. doi:10.1002/art.38238. PMID 24504809. PMC 4198147. https://deepblue.lib.umich.edu/bitstream/2027.42/106579/1/Somers_AandR%202014_MILES%20SLE%20inc%20prev.pdf.
- ↑ Ward MM (2000). "Changes in the incidence of end-stage renal disease due to lupus nephritis, 1982–1995.". Arch Intern Med 160 (20): 3136–40. doi:10.1001/archinte.160.20.3136. PMID 11074743.
- ↑ "General Pathology Images for Immunopathology". Archived from the original on 2007-05-10. https://web.archive.org/web/20070510100001/http://erl.pathology.iupui.edu/C603/GENE607.HTM. Retrieved 2007-07-24.
- ↑ 31.0 31.1 "The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes". Arthritis Rheum. 42 (4): 599–608. April 1999. doi:10.1002/1529-0131(199904)42:4<599::AID-ANR2>3.0.CO;2-F. PMID 10211873.
- ↑ 32.0 32.1 Kasama, T; Maeoka, A; Oguro, N (2016). "Clinical Features of Neuropsychiatric Syndromes in Systemic Lupus Erythematosus and Other Connective Tissue Diseases.". Clinical Medicine Insights. Arthritis and Musculoskeletal Disorders 9: 1–8. doi:10.4137/CMAMD.S37477. PMID 26819561.
- ↑ "Managing neuropsychiatric lupus: Top 10 clinical pearls". The Journal of Musculoskeletal Medicine 26 (4). April 2, 2009. Archived from the original on April 27, 2009. https://web.archive.org/web/20090427042535/http://jmm.consultantlive.com/display/article/1145622/1396901.
- ↑ 34.0 34.1 34.2 "Neurological syndromes in systemic lupus erythematosus and their association with antiphospholipid syndrome". Neurol. Neurochir. Pol. 42 (6): 513–7. 2008. PMID 19235104. http://www.neurology.termedia.pl/showarticle.php?id=11794.
- ↑ Omdal R (2002). "Some controversies of neuropsychiatric systemic lupus erythematosus". Scand. J. Rheumatol. 31 (4): 192–7. doi:10.1080/030097402320318369. PMID 12369649.
- ↑ "Lupus site (SLE)". Archived from the original on 2010-03-29. https://web.archive.org/web/20100329044737/http://www.uklupus.co.uk/fact5.html. Retrieved 2009-11-06.
- ↑ "Intracranial hypertension syndrome in systemic lupus erythematosus: Clinical analysis and review of the literature". J. Huazhong Univ. Sci. Technol. Med. Sci. 29 (1): 107–11. February 2009. doi:10.1007/s11596-009-0123-3. PMID 19224175.
- ↑ West SG (September 1996). "Lupus and the central nervous system". Curr Opin Rheumatol 8 (5): 408–14. doi:10.1097/00002281-199609000-00004. PMID 8941443.
- ↑ "Prevalence of depression and depressive symptoms in patients with systemic lupus erythematosus: Iranian experience". Rheumatol Int 32 (5): 1179–87. January 2011. doi:10.1007/s00296-010-1791-9. PMID 21253731.
- ↑ Dammacco, Rosanna (May 2018). "Systemic lupus erythematosus and ocular involvement: an overview". Clinical and Experimental Medicine 18 (2): 135–149. doi:10.1007/s10238-017-0479-9. ISSN 1591-9528. PMID 29243035.
- ↑ Clowse, ME (May 2007). "Lupus activity in pregnancy.". Rheumatic Diseases Clinics of North America 33 (2): 237–52, v. doi:10.1016/j.rdc.2007.01.002. PMID 17499705.
- ↑ Smyth, Andrew; Guilherme H.M. Oliveira; Brian D. Lahr; Kent R. Bailey; Suzanne M. Norby; Vesna D. Garovic (November 2010). "A Systematic Review and Meta-Analysis of Pregnancy Outcomes in Patients with Systemic Lupus Erythematosus and Lupus Nephritis". Clinical Journal of the American Society of Nephrology 5 (11): 2060–2068. doi:10.2215/CJN.00240110. PMID 20688887. PMC 3001786. Archived from the original on 2016-01-26. https://web.archive.org/web/20160126141220/http://cjasn.asnjournals.org/content/5/11/2060.abstract.
- ↑ Cortés‐Hernández, J.; Ordi‐Ros, J.; Paredes, F.; Casellas, M.; Castillo, F.; Vilardell‐Tarres, M. (December 2001). "Clinical predictors of fetal and maternal outcome in systemic lupus erythematosus: a prospective study of 103 pregnancies". Rheumatology 41 (6): 643–650. doi:10.1093/rheumatology/41.6.643. PMID 12048290.
- ↑ 44.0 44.1 thefreedictionary.com > neonatal lupus Citing: Dorland's Medical Dictionary for Health Consumers. Copyright 2007
- ↑ D'Cruz DP (April 2006). "Systemic lupus erythematosus". BMJ 332 (7546): 890–4. doi:10.1136/bmj.332.7546.890. PMID 16613963.
- ↑ "Fatigue in systemic lupus erythematosus: contributions of disease activity, pain, depression, and perceived social support". J. Rheumatol. 32 (9): 1699–705. September 2005. PMID 16142863. Archived from the original on 2007-08-16. https://web.archive.org/web/20070816055540/http://www.jrheum.com/subscribers/05/09/1699.html.
- ↑ Schneider, L; Dos Santos, AS; Santos, M; da Silva Chakr, RM; Monticielo, OA (August 2014). "Vitamin D and systemic lupus erythematosus: state of the art.". Clinical Rheumatology 33 (8): 1033–8. doi:10.1007/s10067-014-2530-5. PMID 24573738.
- ↑ "An extensive screen of the HLA region reveals an independent association of HLA class I and class II with susceptibility for systemic lupus erythematosus". Scand. J. Rheumatol. 38 (4): 256–62. March 2009. doi:10.1080/03009740802552469. PMID 19255932. https://semanticscholar.org/paper/252fe8c772d252d5e1d0d6c0c8d2b0f345d59124.
- ↑ 49.0 49.1 49.2 "Population differences in SLE susceptibility genes: STAT4 and BLK, but not PXK, are associated with systemic lupus erythematosus in Hong Kong Chinese". Genes Immun. 10 (3): 219–26. February 2009. doi:10.1038/gene.2009.1. PMID 19225526.
- ↑ "A regulatory SNP at position -899 in CDKN1A is associated with systemic lupus erythematosus and lupus nephritis". Genes Immun. 10 (5): 482–6. March 2009. doi:10.1038/gene.2009.5. PMID 19262578.
- ↑ "The genetics of SLE: an update in the light of genome-wide association studies". Rheumatology (Oxford) 47 (11): 1603–11. November 2008. doi:10.1093/rheumatology/ken247. PMID 18611920.
- ↑ 52.0 52.1 Moser, K. L.; Kelly, J. A.; Lessard, C. J.; Harley, J. B. (2009-07-01). "Recent insights into the genetic basis of systemic lupus erythematosus". Genes and Immunity 10 (5): 373–379. doi:10.1038/gene.2009.39. ISSN 1476-5470. PMID 19440199.
- ↑ Kelly, J. A.; Moser, K. L.; Harley, J. B. (2002-10-01). "The genetics of systemic lupus erythematosus: putting the pieces together". Genes and Immunity 3 Suppl 1: S71–85. doi:10.1038/sj.gene.6363885. ISSN 1466-4879. PMID 12215907.
- ↑ Prokunina, Ludmila; Alarcon-Riquelme, Marta (2004-04-01). "The genetic basis of systemic lupus erythematosus—knowledge of today and thoughts for tomorrow". Human Molecular Genetics 13 Spec No 1 (90001): R143–148. doi:10.1093/hmg/ddh076. ISSN 0964-6906. PMID 14764622.
- ↑ "Drug-Induced Lupus Erythematosus". (non-archive version no longer available): Lupus Foundation of America. Archived on 2006-10-13. Error: If you specify
|archivedate=, you must also specify|archiveurl=. http://www.lupus.org/education/brochures/drug.html. Retrieved 20 June 2018. - ↑ Millard LG (1979). "Abnormal Laboratory Test Results and Their Relationship to Prognosis in Discoid Lupus Erythematosus. A Long-term Follow-up Study of 92 Patients". Archives of Dermatology 115 (9): 1055–058. doi:10.1001/archderm.1979.04010090005011.
- ↑ Mary K. Crow (February 28, 2008). "Collaboration, Genetic Associations, and Lupus Erythematosus". N Engl J Med 358 (9): 956–961. doi:10.1056/NEJMe0800096. PMID 18204099.
- ↑ Geoffrey Hom et al. (February 28, 2008). "Association of Systemic Lupus Erythematosus with C8orf13–BLK and ITGAM–ITGAX". N Engl J Med 358 (9): 900–9. doi:10.1056/NEJMoa0707865. PMID 18204098. https://semanticscholar.org/paper/4decf9b11b26aeedf87ad0206f6d63a632e9002c.
- ↑ "University of South Carolina School of Medicine lecture notes, Immunology, Hypersensitivity reactions. General discussion of hypersensitivity, not specific to SLE". Pathmicro.med.sc.edu. 2010-07-07. Archived from the original on 2011-08-03. https://web.archive.org/web/20110803082424/http://pathmicro.med.sc.edu/ghaffar/hyper00.htm. Retrieved 2011-08-06.
- ↑ "Reticulate and stellate acral pigmentation associated with systemic lupus erythematosus and high titers of circulating anticardiolipin antibodies: a possible association with acral microlivedo". Journal of Drugs in Dermatology 2 (6): 674–6. December 2003. PMID 14711150.
- ↑ 61.0 61.1 "Systemic lupus erythematosus". Lancet 369 (9561): 587–96. February 2007. doi:10.1016/S0140-6736(07)60279-7. PMID 17307106.
- ↑ "Three checkpoints in lupus development: central tolerance in adaptive immunity, peripheral amplification by innate immunity and end-organ inflammation". Genes Immun. 10 (5): 390–6. March 2009. doi:10.1038/gene.2009.6. PMID 19262576.
- ↑ "Complement C3 (Blood)—Health Encyclopedia—University of Rochester Medical Center". Archived from the original on 2016-09-24. https://web.archive.org/web/20160924171124/https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=167&contentid=complement_c3_blood.
- ↑ Clearance of apoptotic cells in human SLE. Current Directions in Autoimmunity. 9. 2006. 173–87. doi:10.1159/000090781. ISBN 978-3-8055-8036-6.
- ↑ Gergely P Jr; Grossman C; Niland B; Puskas F; Neupane H; Allam F; Banki K; Phillips PE et al. (January 2002). "Mitochondrial hyperpolarization and ATP depletion in patients with systemic lupus erythematosus.". Arthritis Rheum. 46 (1): 175–90. doi:10.1002/1529-0131(200201)46:1<175::AID-ART10015>3.0.CO;2-H. PMID 11817589.
- ↑ "Impairment of neutrophil extracellular trap degradation is associated with lupus nephritis". Proc. Natl. Acad. Sci. U.S.A. 107 (21): 9813–8. May 2010. doi:10.1073/pnas.0909927107. PMID 20439745. Bibcode: 2010PNAS..107.9813H.
- ↑ "Mutation of DNASE1 in people with systemic lupus erythematosus". Nat. Genet. 28 (4): 313–4. 2001. doi:10.1038/91070. PMID 11479590.
- ↑ "Clearance deficiency and systemic lupus erythematosus (SLE)". J. Autoimmun. 28 (2–3): 114–21. 2007. doi:10.1016/j.jaut.2007.02.005. PMID 17368845.
- ↑ "Early targets of nuclear RNP humoral autoimmunity in human systemic lupus erythematosus". Arthritis Rheum. 60 (3): 848–859. February 2009. doi:10.1002/art.24306. PMID 19248110.
- ↑ "High Mobility Group Box 1: a potential therapeutic target for systemic lupus erythematosus". Mol. Biol. Rep. 37 (3): 1191–5. February 2009. doi:10.1007/s11033-009-9485-7. PMID 19247800.
- ↑ Aringer, M; Costenbader, K; Daikh, D; Brinks, R; Mosca, M; Ramsey-Goldman, R; Smolen, JS; Wofsy, D et al. (September 2019). "2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus.". Arthritis & Rheumatology 71 (9): 1400–1412. doi:10.1002/art.40930. PMID 31385462.
- ↑ Ther Clin Risk Manag. 2011; 7: 27–32. The lupus band test in systemic lupus erythematosus patients. Adam Reich, Katarzyna Marcinow, and Rafal Bialynicki-Birula
- ↑ "Maternal autoantibodies and congenital heart block: mediators, markers, and therapeutic approach". Semin. Arthritis Rheum. 33 (3): 140–54. December 2003. doi:10.1016/j.semarthrit.2003.09.002. PMID 14671725.
- ↑ NIM encyclopedic article on the LE cell test
- ↑ "Article on the classification of rheumatic diseases". Rheumatology.org. 2011-06-08. Archived from the original on 2011-07-18. https://web.archive.org/web/20110718192030/http://www.rheumatology.org/publications/classification/index.asp?aud=mem. Retrieved 2011-08-06.
- ↑ "Revision of Rheumatology.org's diagnostic criteria". Rheumatology.org. 2011-06-08. Archived from the original on 2011-07-18. https://web.archive.org/web/20110718192053/http://www.rheumatology.org/publications/classification/SLE/1982SLEupdate.asp?aud=mem. Retrieved 2011-08-06.
- ↑ 77.00 77.01 77.02 77.03 77.04 77.05 77.06 77.07 77.08 77.09 77.10 77.11 "Analysis of the 1982 ARA lupus criteria data set by recursive partitioning methodology: new insights into the relative merit of individual criteria". J. Rheumatol. 15 (10): 1493–8. 1988. PMID 3060613.
- ↑ Weinstein, A; Bordwell, B; Stone, B; Tibbetts, C; Rothfield, NF (February 1983). "Antibodies to native DNA and serum complement (C3) levels. Application to diagnosis and classification of systemic lupus erythematosus.". The American Journal of Medicine 74 (2): 206–16. doi:10.1016/0002-9343(83)90613-7. PMID 6600582.
- ↑ "UpToDate Patient information article on DNA antibodies". Patients.uptodate.com. Archived from the original on 2007-10-11. https://web.archive.org/web/20071011145146/http://patients.uptodate.com/topic.asp?file=dx_rheum%2F18305. Retrieved 2011-08-06.
- ↑ "Common Symptoms of Lupus". Lupus Foundation of America. Archived from the original on 2013-04-19. https://web.archive.org/web/20130419103517/http://www.lupus.org/webmodules/webarticlesnet/templates/new_learndiagnosing.aspx?articleid=2241&zoneid=524. Retrieved 7 June 2013.
- ↑ 81.0 81.1 "Catastrophic antiphospholipid syndrome: international consensus statement on classification criteria and treatment guidelines". Lupus 12 (7): 530–4. 2003. doi:10.1191/0961203303lu394oa. PMID 12892393. http://openurl.ingenta.com/content/nlm?genre=article&issn=0961-2033&volume=12&issue=7&spage=530&aulast=Asherson.
- ↑ "Livedo reticularis and pregnancy morbidity in patients negative for antiphospholipid antibodies". Ann. Rheum. Dis. 64 (1): 147–8. 2005. doi:10.1136/ard.2004.020743. PMID 15608315.
- ↑ "Seronegative antiphospholipid syndrome". Ann. Rheum. Dis. 62 (12): 1127. 2003. doi:10.1136/ard.2003.006163. PMID 14644846.
- ↑ Hughes GR (1998). "Is it lupus? The St. Thomas' Hospital "alternative" criteria". Clin. Exp. Rheumatol. 16 (3): 250–2. PMID 9631744.
- ↑ Fernandes Moça Trevisani, Virginia; Castro, Aldemar A; Ferreira Neves Neto, João; Atallah, Álvaro N (2013-02-28). "Cyclophosphamide versus methylprednisolone for treating neuropsychiatric involvement in systemic lupus erythematosus". Cochrane Database of Systematic Reviews (2): CD002265. doi:10.1002/14651858.cd002265.pub3. ISSN 1465-1858. PMID 23450535.
- ↑ 86.0 86.1 86.2 86.3 86.4 86.5 "Established and novel treatments for lupus". The Journal of Musculoskeletal Medicine 26 (8). August 4, 2009. http://www.musculoskeletalnetwork.com/lupus/article/1145622/1434518.[no|permanent dead link|dead link}}]
- ↑ 87.0 87.1 "FDA approves first new lupus drug in 56 years". Archived from the original on 3 May 2011. https://web.archive.org/web/20110503191041/https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm246489.htm. Retrieved 6 May 2011.
- ↑ 88.0 88.1 "BAFF and innate immunity: new therapeutic targets for systemic lupus erythematosus". Immunology and Cell Biology 90 (3): 293–303. 2012. doi:10.1038/icb.2011.111. PMID 22231653. http://www.nature.com/icb/journal/vaop/ncurrent/abs/icb2011111a.html. Retrieved 10 January 2012.
- ↑ FDA Alert: Mycophenolate Mofetil (marketed as CellCept) and Mycophenolic Acid (marketed as Myfortic). May 16, 2008. Archived from the original on August 3, 2010. https://web.archive.org/web/20100803153442/https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm124776.htm.
- ↑ Suarez-Almazor, Maria E; Belseck, Elaine; Shea, Beverley; Tugwell, Peter; Wells, George A (2000-10-23). "Cyclophosphamide for treating rheumatoid arthritis". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.cd001157. ISSN 1465-1858.
- ↑ "Handout on Health: Systemic Lupus Erythematosus, National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health, U.S. Department of Health and Human Services". Archived from the original on 2010-12-04. https://web.archive.org/web/20101204095742/http://www.niams.nih.gov/Health_Info/Lupus/default.asp. Retrieved 2010-10-13.
- ↑ "Intravenous Immunoglobulins (IVIGs) in Lupus Central Station, sourced from the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health, U.S. Department of Health and Human Services". Archived from the original on 2011-10-20. https://web.archive.org/web/20111020213817/http://theodora.com/lupus_central_station/intravenous_immunoglobulins_ivigs.html. Retrieved 2010-10-13.
- ↑ "Disease recurrence in paediatric renal transplantation". Pediatr. Nephrol. 24 (11): 2097–108. February 2009. doi:10.1007/s00467-009-1137-6. PMID 19247694.
- ↑ Ünlü, O; Zuily, S; Erkan, D (2016). "The clinical significance of antiphospholipid antibodies in systemic lupus erythematosus". European Journal of Rheumatology 3 (2): 75–84. doi:10.5152/eurjrheum.2015.0085. PMID 27708976.
- ↑ "Epidemiology of systemic lupus erythematosus: a comparison of worldwide disease burden". Lupus 15 (5): 308–18. 2006. doi:10.1191/0961203306lu2305xx. PMID 16761508. http://openurl.ingenta.com/content/nlm?genre=article&issn=0961-2033&volume=15&issue=5&spage=308&aulast=Danchenko.
- ↑ "Handout on Health: Systemic Lupus Erythematosus". The National Institute of Arthritis and Musculoskeletal and Skin Diseases. National Institutes of Health. August 2003. Archived from the original on 2007-10-18. https://web.archive.org/web/20071018040714/http://www.niams.nih.gov/Health_Info/Lupus/default.asp. Retrieved 2007-11-23.
- ↑ "Prognosis and a Hopeful Future". Lupus Foundation of America website. Archived from the original on 20 March 2011. https://web.archive.org/web/20110320042014/http://www.lupus.org/webmodules/webarticlesnet/templates/new_learnunderstanding.aspx?articleid=2238&zoneid=523. Retrieved 14 December 2010.
- ↑ Singh, RR; Yen, EY (September 2018). "SLE mortality remains disproportionately high, despite improvements over the last decade.". Lupus 27 (10): 1577–1581. doi:10.1177/0961203318786436. PMID 30016928.
- ↑ 99.0 99.1 99.2 99.3 99.4 "Epidemiology of systemic lupus erythematosus: a comparison of worldwide disease burden". Lupus 15 (5): 308–18. 2006. doi:10.1191/0961203306lu2305xx. PMID 16761508. http://openurl.ingenta.com/content/nlm?genre=article&issn=0961-2033&volume=15&issue=5&spage=308&aulast=Danchenko.
- ↑ 100.0 100.1 "OMHD|AMH|Factsheets|Lupus". Archived from the original on 2009-01-11. https://web.archive.org/web/20090111033453/http://www.cdc.gov/omhd/AMH/factsheets/lupus.htm.
- ↑ "Systemic lupus erythematosus". N. Engl. J. Med. 358 (9): 929–39. February 2008. doi:10.1056/NEJMra071297. PMID 18305268.
- ↑ Borgia, RE; Silverman, ED (September 2015). "Childhood-onset systemic lupus erythematosus: an update.". Current Opinion in Rheumatology 27 (5): 483–92. doi:10.1097/bor.0000000000000208. PMID 26200474.
- ↑ Sule S, Petri M (2006). "Socioeconomic Status in Systemic Lupus Erythematosus". Lupus 15 (11): 720–23. doi:10.1177/0961203306070008. PMID 17153841.
- ↑ 104.0 104.1 104.2 104.3 104.4 104.5 104.6 Pons-Estel, Guillermo J; Alarcon, Graciela S; Scofield, Lacie; Cooper, Glinda S (February 2010). "Understanding the Epidemiology and Progression of Systemic Lupus Erythematosus". Seminars in Arthritis and Rheumatism 39 (4): 257–68. doi:10.1016/j.semarthrit.2008.10.007. PMID 19136143.
- ↑ Ow, M.Y.; Ho, P.C.; Thumboo, J.; Wee, H.L. (Nov–Dec 2010). "Factors associated with health services utilization in patients with systemic lupus erythematosus: a systematic review". Clinical and Experimental Rheumatology 28 (6): 892–904. PMID 21122271.
- ↑ 106.0 106.1 Yelin, Edward; Yazdany, Jinoos; Tonner, Chris; Criswell, Lindsey A; Katz, Patricia; Schamjuk, Gabriela (2014). "Interactions between patients, providers, and health systems and technical quality of care". Arthritis Care & Research 67 (3): 417–424. doi:10.1002/acr.22427. PMID 25132660.
- ↑ Tsokos GC (December 2011). "Systemic lupus erythematosus". N. Engl. J. Med. 365 (22): 2110–21. doi:10.1056/NEJMra1100359. PMID 22129255.
- ↑ "Gender and Autoimmunity". Autoimmunity Reviews 6 (6): 366–72. 2007. doi:10.1016/j.autrev.2006.10.001. PMID 17537382.
- ↑ Justiz Vaillant, AA; Varacallo, M (2019), "article-24526", Lupus Erythematosus, Treasure Island (FL): StatPearls Publishing, PMID 30571026, http://www.ncbi.nlm.nih.gov/books/NBK535405/, retrieved 2019-12-21
- ↑ Lupus Foundation of America. "What is the history of lupus?". Archived from the original on 4 November 2014. https://web.archive.org/web/20141104073119/http://www.lupus.org/answers/entry/what-is-the-history-of-lupus. Retrieved 11 October 2014.
- ↑ "Definition in Dictionary.com". Dictionary.reference.com. Archived from the original on 2012-10-26. https://web.archive.org/web/20121026063456/http://dictionary.reference.com/browse/lupus. Retrieved 2012-10-24.
- ↑ Thomas, Jr., Donald E. (2014). The Lupus Encyclopedia: A Comprehensive Guide for Patients and Families. Baltimore, Maryland: Johns Hopkins University Press. p. 4. ISBN 978-1-4214-0984-9.
- ↑ Thomas, Jr., Donald E. (2014). The Lupus Encyclopedia: A Comprehensive Guide for Patients and Families. Baltimore, Maryland: Johns Hopkins University Press. p. 463. ISBN 978-1-4214-0984-9.
- ↑ Phillips, Robert H. (2012). Coping with Lupus: A Practical Guide to Alleviating the Challenges of Systemic Lupus Erythematosus (4th ed.). New York, NY: The Penguin Group. pp. 11–12. ISBN 978-1-58333-445-4. https://archive.org/details/isbn_9781583334454/page/11.
- ↑ 115.0 115.1 115.2 115.3 Talbott, John H. (1966). "Historical Background of Discoid and Systemic Lupus Erythematosus". in Dubois, Edmund L.. Lupus Erythematosus: A review of the current status of Discoid and Systemic Lupus Erythematosus. New York: McGraw Hill. pp. 1–9.
- ↑ Hebra, Ferdinand (1866). Fagge, C. Hilton. ed. Diseases of the skin including the Exanthemata (Vol. 1 ed.). London, England: The New Sydenham Society. pp. 114–116. https://archive.org/details/in.ernet.dli.2015.63788.
- ↑ Blau, Sheldon Paul; Schultz, Dodi (1984). Lupus:The body against itself (2nd ed.). New York: Doubleday & Company Inc.. p. 6.
- ↑ Rostein, J. (1974). Kargar, S.. ed. "Immunosuppresion Systemic Lupus Erythematosus". Rheumatology: An Annual Review 5 (5 volumes 1967–1974): 52–53.
- ↑ Carr, Ronald I. (1986). Lupus Erythematosus: A Handbook for Physicians, Patients, and their Families (2nd ed.). Lupus Foundation of America Inc.. p. 3.
- ↑ Wallace, Daniel J. (1995). The Lupus Book. New York: Oxford University Press. p. 8. https://archive.org/details/lupusbook00wall.
- ↑ Carr, Robert I. (1986). Lupus Erythematosus: A Handbook for Physicians, Patients and Their Families (2nd ed.). Lupus Foundation of America Inc.. p. 15.
- ↑ Lahita, Robert G.; Phillips, Robert H. (2004). Lupus Q&A: Everything you need to know (2nd ed.). New York, NY: Penguin Group (USA). pp. 65–66. ISBN 978-1-58333-196-5. https://archive.org/details/lupusqaeverythin00lah_l84/page/65.
- ↑ Phillips, Robert H. (2012). Coping with Lupus: A Practical Guide to Alleviating the Challenges of Systemic Lupus Erythematosus (4th ed.). New York, NY: The Penguin Group. p. 24. ISBN 978-1-58333-445-4. https://archive.org/details/isbn_9781583334454/page/24.
- ↑ Thomas, Jr., Donald E. (2014). The Lupus Encyclopedia: A Comprehensive Guide for Patients and Families. Baltimore, USA: Johns Hopkins University Press. p. 26. ISBN 978-1-4214-0984-9.
- ↑ Thomas, Jr., Donald E. (2014). The Lupus Encyclopedia: A Comprehensive Guide for Patients and Families. Baltimore, USA: Johns Hopkins University Press. pp. 17–21. ISBN 978-1-4214-0984-9.
- ↑ 126.0 126.1 Hochberg MC (October 1991). "The history of lupus erythematosus". Md Med J 40 (10): 871–3. PMID 1943516.
- ↑ Jordan, Natasha; D’Cruz, David P (29 December 2014). "Belimumab for the treatment of systemic lupus erythematosus". Expert Review of Clinical Immunology 11 (2): 195–204. doi:10.1586/1744666X.2015.996550. PMID 25543845.
- ↑ Couzin-FrankelMar. 6, Jennifer (6 March 2019). "Genetically engineered immune cells wipe out lupus in mice" (in en). https://www.sciencemag.org/news/2019/03/genetically-engineered-immune-cells-wipe-out-lupus-mice. Retrieved 8 May 2019.
External links
| Classification | |
|---|---|
| External resources |
- Systemic lupus erythematosus at Curlie
- Systemic Lupus Erythematosus at National Institute of Arthritis and Musculoskeletal and Skin Diseases