Chemistry:Hydralazine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Apresoline, BiDil, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682246 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 26–50% |
| Protein binding | 85–90% |
| Metabolism | Liver |
| Onset of action | 5 to 30 min[1] |
| Elimination half-life | 2–8 hours, 7–16 hours (renal impairment) |
| Duration of action | 2 to 6 hrs[1] |
| Excretion | Urine |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
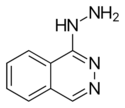
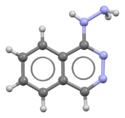
| Formula | C8H8N4 |
| Molar mass | 160.180 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Hydralazine, sold under the brand name Apresoline among others, is a medication used to treat high blood pressure and heart failure.[1] This includes high blood pressure in pregnancy and very high blood pressure resulting in symptoms.[2] It has been found to be particularly useful in heart failure, together with isosorbide dinitrate, for treatment of people of African descent.[1] It is given by mouth or by injection into a vein.[2] Effects usually begin around 15 minutes and last up to six hours.[1]
Common side effects include headache and fast heart rate.[1] It is not recommended in people with coronary artery disease or in those with rheumatic heart disease that affects the mitral valve.[1] In those with kidney disease a low dose is recommended.[2] Hydralazine is in the vasodilator family of medications, so it is believed to work by causing the dilation of blood vessels.[1]
Hydralazine was discovered while scientists at Ciba were looking for a treatment for malaria.[3] It was patented in 1949.[4] It is on the World Health Organization's List of Essential Medicines.[5] In 2020, it was the 103rd most commonly prescribed medication in the United States, with more than 6 million prescriptions.[6][7]
Medical use
Hydralazine is not used as a primary drug for treating hypertension because it elicits a reflex sympathetic stimulation of the heart (the baroreceptor reflex).[8] The sympathetic stimulation may increase heart rate and cardiac output, and in people with coronary artery disease may cause angina pectoris or myocardial infarction.[9] Hydralazine may also increase plasma renin concentration, resulting in fluid retention. To prevent these undesirable side effects, hydralazine is usually prescribed in combination with a beta blocker (e.g., propranolol) and a diuretic.[9] Beta-blockers licensed to treat heart failure in the UK include bisoprolol, carvedilol, and nebivolol.[10][11][12]
Hydralazine is used to treat severe hypertension, but is not a first-line therapy for essential hypertension. Hydralazine is often used to treat hypertension in pregnancy, though, with either labetalol and/or methyldopa.[13]
Hydralazine is commonly used in combination with isosorbide dinitrate for the treatment of congestive heart failure in black populations. This preparation, isosorbide dinitrate/hydralazine, was the first race-based prescription drug.[14]
It should not be used in people who have tachycardia, heart failure, constrictive pericarditis, lupus, a dissecting aortic aneurysm, or porphyria.[15]
Adverse effects
Prolonged treatment may cause a syndrome similar to lupus, which can become fatal if the symptoms are not noticed and drug treatment stopped.[15] Hydralazine is within the top three drugs that is known to induce systemic lupus and this adverse drug event is dose dependent yet significant.
Very common (>10% frequency) side effects include headache, tachycardia, and palpitations.[15]
Common (1–10% frequency) side effects include flushing, hypotension, anginal symptoms, aching or swelling joints, muscle aches, positive tests for atrial natriuretic peptide, stomach upset, diarrhea, nausea and vomiting, and swelling (sodium and water retention).[15]
Interactions
It may potentiate the antihypertensive effects of:[15]
Drugs subject to a strong first-pass effect such as beta blockers may increase the bioavailability of hydralazine.[15] The heart rate-accelerating effects of epinephrine (adrenaline) are increased by hydralazine, and coadministration may lead to toxicity.[15]
Mechanism of action
Hydralazine is a direct-acting smooth muscle relaxant and acts as a vasodilator primarily in resistance arterioles, also known as the smooth muscle of the arterial bed. The molecular mechanism involves inhibition of inositol trisphosphate-induced Ca2+ release from the sarcoplasmic reticulum in arterial smooth muscle cells.[16][17] By relaxing vascular smooth muscle, vasodilators act to decrease peripheral resistance, thereby lowering blood pressure and decreasing afterload.[9]
Metabolic products include the N-acetyl derivative, pyruvic acid hydrazone, and acetone hydrazone, each of which may also contribute to reducing blood pressure.[18]
Chemistry
Hydralazine belongs to the hydrazinophthalazine class of drugs.[19]
History
The antihypertensive activity of hydralazine was discovered by scientists at Ciba, who were trying to discover drugs to treat malaria; it was initially called C-5968 and 1-hydrazinophthalazine; Ciba's patent application was filed in 1945 and issued in 1949,[20][21][22] and the first scientific publications of its blood pressure-lowering activities appeared in 1950.[3][19][23] It was approved by the FDA in 1953.[24]
It was one of the first antihypertensive medications that could be taken by mouth.[8]
Research
Hydralazine has also been studied as a treatment for myelodysplastic syndrome in its capacity as a DNA methyltransferase inhibitor.[25]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 "Hydralazine Hydrochloride". The American Society of Health-System Pharmacists. https://www.drugs.com/monograph/hydralazine-hydrochloride.html.
- ↑ 2.0 2.1 2.2 WHO Model Formulary 2008. World Health Organization. 2009. p. 280. ISBN 9789241547659.
- ↑ 3.0 3.1 (in en) The Practice of Medicinal Chemistry. Academic Press. 2 May 2011. p. 12. ISBN 9780080568775. https://books.google.com/books?id=Qmt1_DQkCpEC&pg=PA12.
- ↑ (in en) Progress in Drug Research/Fortschritte der Arzneimittelforschung/Progrés des recherches pharmaceutiques. Birkhäuser. 2013. p. 206. ISBN 9783034870948. https://books.google.com/books?id=i8LzBwAAQBAJ&pg=PA206.
- ↑ World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. 2019. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ "The Top 300 of 2020". https://clincalc.com/DrugStats/Top300Drugs.aspx.
- ↑ "Hydralazine - Drug Usage Statistics". https://clincalc.com/DrugStats/Drugs/Hydralazine.
- ↑ 8.0 8.1 "Hydralazine for essential hypertension". The Cochrane Database of Systematic Reviews (11): CD004934. November 2011. doi:10.1002/14651858.CD004934.pub4. PMID 22071816.
- ↑ 9.0 9.1 9.2 Lippincott's Illustrated Reviews: Pharmacology. (2nd ed.). Philadelphia: Lippincott Williams & Wilkins. 2000. p. 190.
- ↑ Joint Formulary Committee. "Bisoprolol fumarate". BMJ Group and Pharmaceutical Press. https://bnf.nice.org.uk/drugs/bisoprolol-fumarate/.
- ↑ Joint Formulary Committee. "Carvedilol". BMJ Group and Pharmaceutical Press. https://bnf.nice.org.uk/drugs/carvedilol/.
- ↑ Joint Formulary Committee. "Nebivolol". BMJ Group and Pharmaceutical Press. https://bnf.nice.org.uk/drugs/nebivolol/.
- ↑ First Aid for the USMLE Step 1.. New York: McGraw-Hill Medical. 2007. p. 251.
- ↑ "Use of isosorbide dinitrate and hydralazine in African-Americans with heart failure 9 years after the African-American Heart Failure Trial". The American Journal of Cardiology 114 (1): 151–9. July 2014. doi:10.1016/j.amjcard.2014.04.018. PMID 24846808. http://www.ajconline.org/article/S0002-9149(14)00975-8/pdf.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 "Hydralazine Tablets 50mg" (in en). UK Electronic Medicines Compendium. 7 September 2016. https://www.medicines.org.uk/emc/medicine/24412.
- ↑ "Inhibition of calcium release from the sarcoplasmic reticulum of rabbit aorta by hydralazine". British Journal of Pharmacology 114 (1): 238–244. January 1995. doi:10.1111/j.1476-5381.1995.tb14931.x. PMID 7712024.
- ↑ "Mechanisms of hydralazine induced vasodilation in rabbit aorta and pulmonary artery". British Journal of Pharmacology 134 (3): 621–631. October 2001. doi:10.1038/sj.bjp.0704302. PMID 11588117.
- ↑ "Direct-acting vasodilators". Journal of Clinical Hypertension 13 (9): 690–692. 2011. doi:10.1111/j.1751-7176.2011.00507.x. PMID 21896152.
- ↑ 19.0 19.1 "The effect of 1-hydrasinophthalasine in hypertension". Circulation 5 (1): 28–37. January 1952. doi:10.1161/01.cir.5.1.28. PMID 14896450.
- ↑ "Hydralazine". Drugbank. https://www.drugbank.ca/drugs/DB01275.
- ↑ "hydralazine" (in en). PubChem. https://pubchem.ncbi.nlm.nih.gov/compound/hydralazine#section=Physical-Description.
- ↑ US2484029; see Example 1
- ↑ "Renal hyperemia induced in man by a new phthalazine derivative". Proceedings of the Society for Experimental Biology and Medicine 73 (1): 102–103. January 1950. doi:10.3181/00379727-73-17591. PMID 15402536.
- ↑ "New Drug Application (NDA) 008303 Company: NOVARTIS Drug Name(s): Apresoline". FDA. http://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=008303.
- ↑ "DNA methyltransferase-1 inhibitors as epigenetic therapy for cancer". Current Cancer Drug Targets 13 (4): 379–99. May 2013. doi:10.2174/15680096113139990077. PMID 23517596.
External links
- "Hydralazine". Drug Information Portal. U.S. National Library of Medicine. https://druginfo.nlm.nih.gov/drugportal/name/hydralazine.
 |
