Medicine:Mollaret's meningitis
| Mollaret's meningitis | |
|---|---|
| Other names | Benign recurrent lymphocytic meningitis |
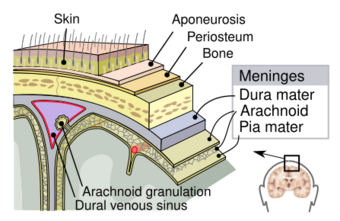 | |
| Meninges of the central nervous system: dura mater, arachnoid, and pia mater. | |
| Specialty | Neurology |
Mollaret's meningitis is a recurrent or chronic inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. Since Mollaret's meningitis is a recurrent, benign (non-cancerous), aseptic meningitis, it is also referred to as benign recurrent lymphocytic meningitis.[1][2] It was named for Pierre Mollaret, the French neurologist who first described it in 1944.[3][4][5]
Although chronic meningitis has been defined as "irritation and inflammation of the meninges persisting for more than 4 weeks being associated with pleocytosis in the cerebrospinal fluid",[2] cerebrospinal fluid abnormalities may not be detectable for the entire time.[6] Diagnosis can be elusive, as Helbok et al. note: "in reality, many more weeks, even months pass by until the diagnosis is established. In many cases the signs and symptoms of chronic meningitis not only persist for periods longer than 4 weeks, they even progress with continuing deterioration, i. e. headache, neck stiffness and even low grade fever. Impairment of consciousness, epileptic seizures, neurological signs and symptoms may evolve over time."[2]
Signs and symptoms
Mollaret's meningitis is characterized by chronic, recurrent episodes of headache, stiff neck, meningismus, and fever; cerebrospinal fluid (CSF) pleocytosis with large "endothelial" cells, neutrophil granulocytes, and lymphocytes; and attacks separated by symptom-free periods of weeks to years; and spontaneous remission of symptoms and signs. Many people have side effects between bouts that vary from chronic daily headaches to after-effects from meningitis such as hearing loss and visual impairment, nerve pain and twitches. Symptoms may be mild or severe.[2] Some cases may be short, lasting only 3–7 days, while others last for weeks to months.[citation needed]
While herpes simplex and varicella can cause rash, Mollaret's patients may or may not have a rash.[7] Herpes simplex virus is likely the most common cause of Mollaret's meningitis.[8]
Cause
Although for a long time, the cause of Mollaret's meningitis was not known, recent work has associated this problem with herpes simplex viruses, particularly HSV-2.[6][9]
Cases of Mollaret's resulting from varicella zoster virus infection, diagnosed by polymerase chain reaction (PCR), have been documented. In these cases, PCR for herpes simplex was negative.[10][11] Some patients also report frequent shingles outbreaks.[citation needed] Varicella zoster virus, which causes chickenpox and shingles is part of the herpes family, and is sometimes called "herpes zoster virus".[12] CNS epidermoid cysts (a type of cholesteatoma) can give rise to Mollaret's meningitis especially with surgical manipulation of cyst contents.[citation needed]
A familial association, where more than one family member had Mollaret's, has been documented.[13]
Diagnosis
Diagnosis starts by examining the patient's symptoms. Symptoms can vary. Symptoms can include headache, sensitivity to light, neck stiffness, nausea, and vomiting. In some patients, fever is absent. Neurological examination and MRI can be normal.[6]
Mollaret's meningitis is suspected based on symptoms, and can be confirmed by HSV 1 or HSV 2 on PCR of Cerebrospinal fluid (CSF), although not all cases test positive on PCR. PCR is performed on spinal fluid or blood, however, the viruses do not need to enter the spinal fluid or blood to spread within the body: they can spread by moving through the axons and dendrites of the nerves.[14]
During the first 24 h of the disease the spinal fluid will show predominant polymorphonuclear neutrophils and large cells that have been called endothelial (Mollaret's) cells.[15]
A study performed on patients who had diffuse symptoms, such as persistent or intermittent headaches, concluded that although PCR is a highly sensitive method for detection, it may not always be sensitive enough for identification of viral DNA in CSF, due to the fact that viral shedding from latent infection may be very low. The concentration of viruses in CSF during subclinical infection might be very low.[16]
Investigations include blood tests (electrolytes, liver and kidney function, inflammatory markers and a complete blood count) and usually X-ray examination of the chest. The most important test in identifying or ruling out meningitis is analysis of the cerebrospinal fluid (fluid that envelops the brain and the spinal cord) through lumbar puncture (LP). However, if the patient is at risk for a cerebral mass lesion or elevated intracranial pressure (recent head injury, a known immune system problem, localizing neurological signs, or evidence on examination of a raised ICP), a lumbar puncture may be contraindicated because of the possibility of fatal brain herniation. In such cases, a CT or MRI scan is generally performed prior to the lumbar puncture to exclude this possibility. Otherwise, the CT or MRI should be performed after the LP, with MRI preferred over CT due to its superiority in demonstrating areas of cerebral edema, ischemia, and meningeal inflammation.[citation needed]
During the lumbar puncture procedure, the opening pressure is measured. A pressure of over 180 mm H2O is suggestive of bacterial meningitis.
It is likely that Mollaret meningitis is underrecognized by physicians, and improved recognition may limit unwarranted antibiotic use and shorten or eliminate unnecessary hospital admission.[13]
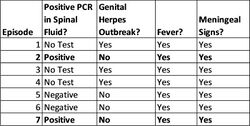
PCR testing has advanced the state of the art in research, but PCR can be negative in individuals with Mollaret's, even during episodes with severe symptoms. For example, Kojima et al. published a case study for an individual who was hospitalized repeatedly, and who had clinical symptoms including genital herpes lesions. However, the patient was sometimes negative for HSV-2 by PCR, even though his meningitis symptoms were severe. Treatment with acyclovir was successful, indicating that a herpes virus was the cause of his symptoms.[17]
Treatment
Acyclovir is the treatment of choice for Mollaret's meningitis. Some patients see a drastic difference in how often they get sick and others don't. Often treatment means managing symptoms, such as pain management and strengthening the immune system.[citation needed]
The IHMF recommends that patients with benign recurrent lymphocytic meningitis receive intravenous acyclovir in the amount of 10 mg/kg every 8 hours, for 14–21 days. More recently, the second-generation antiherpetic drugs valacyclovir and famciclovir have been used to successfully treat patients with Mollaret's. Additionally, it has been reported that Indomethacin administered in the amount of 25 mg 3 times per day after meals, or 50 mg every 4 hours, has resulted in a faster recovery for patients, as well as more extended symptom-free intervals, between episodes.[18]
Prognosis
Recurring Mollaret meningitis attacks generally resolve within 3 to 5 years after the first occurrence, but some patients live with the disease for much longer.[19] With suppressive antiviral therapy, some patients who have Mollaret's report experiencing fewer attacks. However, there are some that have flare ups all throughout the year.[18]
See also
- Encephalitis
- Meningitis
- Herpes simplex virus
- Varicella zoster virus
References
- ↑ Shalabi, M; Whitley, RJ (Nov 1, 2006). "Recurrent benign lymphocytic meningitis.". Clinical Infectious Diseases 43 (9): 1194–7. doi:10.1086/508281. PMID 17029141.
- ↑ 2.0 2.1 2.2 2.3 Raimund Helbok; Gregor Broessner; Bettina Pfausler; Erich Schmutzhard (2009). "Chronic meningitis". J Neurol 256 (2): 168–175. doi:10.1007/s00415-009-0122-0. PMID 19224317.
- ↑ synd/1537 at Who Named It?
- ↑ Mollaret P (1944). "Méningite endothélio-leucocytaire multirécurrente bénigne. Syndrome nouveau ou maladie nouvelle? (Documents cliniques)". Revue neurologique, Paris 76: 57–76.
- ↑ "La méningite endothélio-leukocytaire multi-récurrente bénigne". Rev Neurol (Paris) 76: 57–67. 1944.
- ↑ 6.0 6.1 6.2 Olaf Willmann; Parviz Ahmad-Nejad; Michael Neumaier; Michael G. Hennerici; Marc Fatar (2010). "Toll-Like Receptor 3 Immune Deficiency May Be Causative for HSV-2-Associated Mollaret Meningitis". Eur Neurol 63 (4): 249–251. doi:10.1159/000287585. PMID 20375513.
- ↑ Ugo K. Ihekwaba; Goura Kudesia; Michael W. McKendrick (2008). "Clinical Features of Viral Meningitis in Adults: Significant Differences in Cerebrospinal Fluid Findings among Herpes Simplex Virus, Varicella Zoster Virus, and Enterovirus Infections". Clinical Infectious Diseases 47 (6): 783–9. doi:10.1086/591129. PMID 18680414.
- ↑ Kasper, Dennis L.; Larry Jameson, J.; Hauser, Stephen L.; Loscalzo, Joseph; Fauci, Anthony S.; Longo, Dan L. (2015-04-08). Harrisons Principles of Internal Medicine (19th ed.). p. 1179. ISBN 9780071802154.
- ↑ ((Tarakad S Ramachandran, MBBS, FRCP(C), FACP)) (Feb 12, 2010). "Aseptic Meningitis". Emedicine. http://emedicine.medscape.com/article/1169489-overview.
- ↑ Ohmichi, T.; Takezawa, H.; Fujii, C.; Tomii, Y.; Yoshida, T.; Nakagawa, M. (2012). "Mollaret cells detected in a patient with varicella-zoster virus meningitis.". Clinical Neurology and Neurosurgery 114 (7): 1086–7. doi:10.1016/j.clineuro.2012.02.015. PMID 22402203.
- ↑ Jhaveri, Ravi M.D.; Sankar, Raman M.D.; Yazdani, Shahram M.D.; Cherry, James D. M.D. (2003). "Varicella-zoster virus: an overlooked cause of aseptic meningitis". Pediatric Infectious Disease Journal 22 (1): 96–97. doi:10.1097/00006454-200301000-00026. PMID 12553305.
- ↑ Mollaret's meningitis at patient.co.uk
- ↑ 13.0 13.1 "Mollaret meningitis: case report with a familial association.". Am J Emerg Med 29 (7): 840.e1–840.e2. 2011. doi:10.1016/j.ajem.2010.02.008. PMID 20825883.
- ↑ Tal Kramer; Lynn W. Enquist (2013). "Directional Spread of Alphaherpesviruses in the Nervous System". Viruses 5 (2): 678–707. doi:10.3390/v5020678. PMID 23435239.
- ↑ Mohammed Abu Khattab; Hussam Al Soub; Mona Al Maslamani; Jameela Al Khuwaiter; Yasser El Deeb (2009). "Herpes simplex virus type 2 (Mollaret's) meningitis: A case report". International Journal of Infectious Diseases 13 (6): e476–e479. doi:10.1016/j.ijid.2009.01.003. PMID 19329344.
- ↑ Birgitta Sundén; Marie Larsson; Tina Falkeborn; Jakob Paues; Urban Forsum; Magnus Lindh; Liselotte Ydrenius; Britt Åkerlind et al. (2011). "Real-time PCR detection of Human Herpesvirus 1–5 in patients lacking clinical signs of a viral CNS infection". BMC Infectious Diseases 11: 220. doi:10.1186/1471-2334-11-220. PMID 21849074.
- ↑ Yuki Kojima; Hideyuki Hashiguchi; Tomoko Hashimoto; Sadatoshi Tsuji; Hiroshi Shoji; Yukumasa Kazuyama (2002). "Recurrent Herpes Simplex Virus Type 2 Meningitis: A Case Report of Mollaret's Meningitis". Jpn. J. Infect. Dis. 55 (3): 85–88. PMID 12195049. http://www0.nih.go.jp/JJID/SC-29.pdf. Retrieved 2014-09-21.
- ↑ 18.0 18.1 Shalabi, Marwan; Whitley, Richard J. (2006-11-01). "Recurrent Benign Lymphocytic Meningitis" (in en). Clinical Infectious Diseases 43 (9): 1194–1197. doi:10.1086/508281. ISSN 1058-4838. PMID 17029141.
- ↑ Mirakhur, Beloo; McKenna, Marc (2004-07-01). "Recurrent Herpes Simplex Type 2 Virus (Mollaret) Meningitis" (in en). The Journal of the American Board of Family Practice 17 (4): 303–305. doi:10.3122/jabfm.17.4.303. ISSN 1557-2625. PMID 15243021.
External links
| Classification | |
|---|---|
| External resources |
 |