Chemistry:Durvalumab

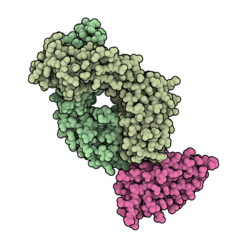 Antigen-binding fragment of durvalumab (pale green) in complex with PD-L1 (pink). PDB: 5X8M. | |
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Human |
| Target | CD274 |
| Clinical data | |
| Trade names | Imfinzi |
| Other names | MEDI4736, MEDI-4736 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a617030 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider |
|
| UNII | |
| KEGG | |
| Chemical and physical data | |
| Formula | C6502H10018N1742O2024S42 |
| Molar mass | 146322.36 g·mol−1 |
Durvalumab,[6] sold under the brand name Imfinzi, is an FDA-approved immunotherapy for cancer, developed by Medimmune/AstraZeneca.[7] It is a human immunoglobulin G1 kappa (IgG1κ) monoclonal antibody that blocks the interaction of programmed cell death ligand 1 (PD-L1) with the PD-1 (CD279).
Durvalumab is an immune checkpoint inhibitor drug.[8]
Medical uses
The US Food and Drug Administration (FDA) approved durvalumab for certain types of bladder, lung, and biliary tract cancer:[4][9]
- Adults with locally advanced or metastatic urothelial carcinoma who either have disease progression during or following platinum-containing chemotherapy or have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- Adults with unresectable, Stage III non-small cell lung cancer whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy.
- In combination with etoposide and either carboplatin or cisplatin, as first-line treatment for adults with extensive-stage small cell lung cancer.
- In combination with gemcitabine and cisplatin for adults with locally advanced or metastatic biliary tract cancer (BTC).[9]
Clinical trials
A phase Ib clinical trial of durvalumab and tremelimumab showed some activity in non-small cell lung cancer (NSCLC)[citation needed] Phase I data in advanced metastatic urothelial bladder (Study 1108) has led to FDA breakthrough therapy designation.[8][10] Early results of a phase I trial combining durvalumab and gefitinib in lung cancer patients "showed promise".[11] A phase I clinical trial is currently underway using durvalumab with a TLR 7/8 agonist (MEDI 9197) for solid tumors.[12] A phase 1b/2a trial is underway combining durvalumab with an HPV DNA vaccine (MEDI 0457) in patients with HPV-associated recurrent/metastatic head and neck cancer.[13]
MYSTIC
In July 2017, AstraZeneca announced that a phase III trial of durvalumab with tremelimumab as a first-line treatment of non-small cell lung cancer failed to meet its primary endpoint of progression-free survival.[14]
PACIFIC
In November 2017, the double-blinded phase III AstraZeneca PACIFIC clinical trial demonstrated the efficacy of durvalumab in the treatment of stage III non-small cell lung cancer.[15] 709 patients with stage III NSCLC who did not have disease progression after two or more cycles of a platinum-based chemotherapy were randomly assigned to receive durvalumab or a placebo as consolidation therapy for their lung cancer. Durvalumab increased the median progression-free survival from 5.6 months (placebo) to 16.8 months (durvalumab); the 12 month progression-free survival rate was increased from 35.3% (placebo) to 55.9% (durvalumab), and the 18 month progression-free survival rate was increased from 27.0% (placebo) to 44.2% (durvalumab).[8] The median time to death or distant metastases was also increased from 14.6 months (placebo) to 23.2 months (durvalumab). Extreme side effects were also increased from 26.1% of patients (placebo) to 29.9% of patients (durvalumab).[citation needed]
CASPIAN
In March 2021, the open-label, sponsor-blind (AstraZeneca), randomised, controlled phase III trial at 209 cancer treatment centres in 23 countries worldwide (CASPIAN) demonstrated the efficacy of durvalumab in combination with platinum-based chemotherapy in the treatment of small cell lung cancer.[16]
Between March 2017, and May 2018, 972 patients were screened and 805 were randomly assigned (268 to durvalumab plus tremelimumab plus platinum–etoposide, 268 to durvalumab plus platinum–etoposide, and 269 to platinum–etoposide). As of Jan 27, 2020, the median follow-up was 25·1 months (IQR 22·3–27·9). Durvalumab plus tremelimumab plus platinum–etoposide was not associated with a significant improvement in overall survival versus platinum–etoposide (hazard ratio [HR] 0·82 [95% CI 0·68–1·00]; p=0·045); median overall survival was 10·4 months (95% CI 9·6–12·0) versus 10·5 months (9·3–11·2). Durvalumab plus platinum–etoposide showed sustained improvement in overall survival versus platinum–etoposide (HR 0·75 [95% CI 0·62–0·91]; nominal p=0·0032); median overall survival was 12·9 months (95% CI 11·3–14·7) versus 10·5 months (9·3–11·2). The most common any-cause grade 3 or worse adverse events were neutropenia (85 [32%] of 266 patients in the durvalumab plus tremelimumab plus platinum–etoposide group, 64 [24%] of 265 patients in the durvalumab plus platinum–etoposide group, and 88 [33%] of 266 patients in the platinum–etoposide group) and anaemia (34 [13%], 24 [9%], and 48 [18%]). Any-cause serious adverse events were reported in 121 (45%) patients in the durvalumab plus tremelimumab plus platinum–etoposide group, 85 (32%) in the durvalumab plus platinum–etoposide group, and 97 (36%) in the platinum–etoposide group. Treatment-related deaths occurred in 12 (5%) patients in the durvalumab plus tremelimumab plus platinum–etoposide group (death, febrile neutropenia, and pulmonary embolism [n=2 each]; enterocolitis, general physical health deterioration and multiple organ dysfunction syndrome, pneumonia, pneumonitis and hepatitis, respiratory failure, and sudden death [n=1 each]), six (2%) patients in the durvalumab plus platinum–etoposide group (cardiac arrest, dehydration, hepatotoxicity, interstitial lung disease, pancytopenia, and sepsis [n=1 each]), and two (1%) in the platinum–etoposide group (pancytopenia and thrombocytopenia [n=1 each]).[17]
TOPAZ-1
Efficacy was evaluated in TOPAZ-1 (NCT03875235), a randomized, double-blind, placebo-controlled, multiregional trial that enrolled 685 patients with histologically confirmed locally advanced unresectable or metastatic BTC who had not previously received systemic therapy for advanced disease.[9]
Trial demographics were as follows: 56% Asian, 37% White, 2% Black, and 4% other race; 7% Hispanic or Latino; 50% male and 50% female; median age was 64 years (range 20-85) and 47% were 65 years or older.[9] Fifty-six percent had intrahepatic cholangiocarcinoma, 25% had gallbladder cancer, and 19% had extrahepatic cholangiocarcinoma.[9]
The major efficacy outcome measure was overall survival (OS).[9] Tumor assessments were conducted every 6 weeks for the first 24 weeks, then every 8 weeks until confirmed objective disease progression.[9] A statistically significant improvement in OS was demonstrated in patients randomized to receive durvalumab with gemcitabine and cisplatin compared to those randomized to receive placebo with gemcitabine and cisplatin.[9] Median OS was 12.8 months (95% CI: 11.1, 14) and 11.5 months (95% CI: 10.1, 12.5) in the durvalumab and placebo arms, respectively (hazard ratio 0.80; 95% CI: 0.66, 0.97, p=0.021).[9] The median progression-free survival was 7.2 months (95% CI: 6.7, 7.4) and 5.7 months (95% CI: 5.6, 6.7) in the durvalumab and placebo arms, respectively. Investigator-assessed overall response rate was 27% (95% CI: 22% - 32%) and 19% (95% CI: 15%-23%) in the durvalumab and placebo arms, respectively.[9]
References
- ↑ "Durvalumab (Imfinzi) Use During Pregnancy". 30 August 2019. https://www.drugs.com/pregnancy/durvalumab.html.
- ↑ "Imfinzi (AstraZeneca Pty Ltd)". 5 December 2022. https://www.tga.gov.au/resources/prescription-medicines-registrations/imfinzi-astrazeneca-pty-ltd-2.
- ↑ "Regulatory Decision Summary - Imfinzi". Health Canada. 23 October 2014. https://hpr-rps.hres.ca/reg-content/regulatory-decision-summary-detail.php?lang=en&linkID=RDS00366.
- ↑ 4.0 4.1 "Imfinzi- durvalumab injection, solution". 5 June 2020. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=8baba4ea-2855-42fa-9bd9-5a7548d4cec3.
- ↑ "Imfinzi EPAR". 17 September 2018. https://www.ema.europa.eu/en/medicines/human/EPAR/imfinzi.
- ↑ "International Nonproprietary Names for Pharmaceutical Substances (INN). Proposed INN: List 112". WHO Drug Information 28 (4). 2014. https://www.who.int/medicines/publications/druginformation/innlists/PL112.pdf. Retrieved 6 September 2022.
- ↑ "Durvalumab (Imfinzi)". https://www.fda.gov/drugs/resources-information-approved-drugs/durvalumab-imfinzi.
- ↑ 8.0 8.1 8.2 "De-novo and acquired resistance to immune checkpoint targeting". The Lancet Oncology 18 (12): e731–e741. December 2017. doi:10.1016/s1470-2045(17)30607-1. PMID 29208439.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 9.8 9.9 "FDA approves durvalumab". 2 September 2022. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-durvalumab-locally-advanced-or-metastatic-biliary-tract-cancer.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ AstraZeneca's (AZN) Durvalumab Granted FDA Breakthrough Therapy Designation . StreeInsider.com Corporate News, FDA, Management Comments. 17 February 2016.
- ↑ "Promising Drug for Lung Cancer and Mesothelioma Patients". 19 May 2016. https://www.mesotheliomahelp.org/2016/05/clinical-trial-points-promising-drug-combo-lung-cancer-mesothelioma-patients-42357/.
- ↑ Clinical trial number NCT02556463 for "A Study of MEDI9197 in Subjects With Solid Tumors or CTCL and in Combination With Durvalumab and/or Palliative Radiation in Subjects With Solid Tumors" at ClinicalTrials.gov
- ↑ Clinical trial number NCT03162224? for "Safety and Efficacy of MEDI0457 and Durvalumab in Patients With HPV Associated Recurrent/Metastatic Head and Neck Cancer" at ClinicalTrials.gov
- ↑ "AstraZeneca reports initial results from the ongoing MYSTIC trial in Stage IV lung cancer". https://www.astrazeneca.com/media-centre/press-releases/2017/astrazeneca-reports-initial-results-from-the-ongoing-mystic-trial-in-stage-iv-lung-cancer-27072017.html.
- ↑ "AstraZeneca presents superior progression-free survival for Imfinzi in the PACIFIC trial of patients with locally-advanced unresectable lung cancer at ESMO 2017 Congress". Sep 2017. https://www.astrazeneca.com/media-centre/press-releases/2017/astrazeneca-presents-superior-progression-free-survival-for-imfinzi-in-the-pacific-trial-of-patients-with-locally-advanced-unresectable-lung-cancer-at-esmo-2017-congress-08092017.html.
- ↑ "A Phase III, Randomized, Multicenter,Open-Label, Comparative Study to Determine the Efficacy of Durvalumab or Durvalumab and Tremelimumab in Combination with Platinum-Based Chemotherapy for the First-Line Treatment in Patients with Extensive Disease Small-Cell Lung Cancer (SCLC) (CASPIAN)". 30 September 2021. https://clinicaltrials.gov/ct2/show/results/NCT03043872.
- ↑ "Durvalumab, with or without tremelimumab, plus platinum–etoposide versus platinum–etoposide alone in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): Updated results from a randomised, controlled, open-label, phase 3 trial". The Lancet Oncology 22 (1): 51–65. January 2021. doi:10.1016/S1470-2045(20)30539-8. PMID 33285097.
External links
- "Durvalumab". NCI Drug Dictionary. National Cancer Institute. https://www.cancer.gov/publications/dictionaries/cancer-drug/def/durvalumab.
- "Durvalumab". 5 May 2017. https://www.cancer.gov/about-cancer/treatment/drugs/durvalumab.
 |

