Biology:CYP4F2
 Generic protein structure example |
Cytochrome P450 4F2 is a protein that in humans is encoded by the CYP4F2 gene. It is an enzyme, a type of protein that catalyzes (helps speed up) chemical reactions inside cells. It is part of the superfamily of cytochrome P450 (CYP) enzymes, and the encoding gene is part of a cluster of cytochrome P450 genes located on chromosome 19.
CYP enzymes (CYPs) function primarily as monooxygenases – enzymes that add exactly one hydroxy group (−OH) to a molecule. CYPs are membrane-bound and expressed in many cells, but are most highly expressed in the liver. CYPs contain heme (a precursor to hemoglobin) and hence are classified as hemoproteins. CYPs are involved in cellular metabolism, hormone synthesis, sterol and cholesterol metabolism, and are critical in maintaining homeostasis, a process by which an organism can maintain internal stability while adjusting to changing external conditions. In humans, CYPs are responsible for about 80% of oxidative metabolism and 50% of the removal of commonly used medical drugs. In addition, CYPs are often disease modifying and hence are frequent drug targets.
In the case of this specific enzyme, its primary substrate (molecule upon which an enzyme acts) is leukotriene B4 (LTB4), an eicosanoid, which is an inflammatory mediator. By hydroxylating LTB4 to its inactivated form 20-hydroxy-LTB4, this enzyme helps regulate inflammation levels in the body for a proper immune response. This enzyme also metabolizes other eicosanoids, a class of compounds produced in leukocytes (white blood cells) by the oxidation of arachidonic acid to regulate immune inflammation promoters.
The other substrates for this enzyme are certain fatty acids and vitamins. The enzyme bioactivates specific prodrugs into their active metabolites (for example, it converts the prodrug pafuramidine into its active form, furamidine). Variations in the gene can affect enzymatic activity, which has implications for drug dosing and bioavailability of fat-soluble vitamins such as vitamin E and vitamin K. In particular, variations affecting vitamin K bioavailability impact the dosing of vitamin K antagonists like warfarin or coumarin.
Gene
The cytochrome P450 4F2 protein is encoded by the CYP4F2 gene in humans.[1]
The term "encoded" in this context means that the gene contains the information or instructions on how to make the protein. The gene is composed of a sequence of nucleotides—building blocks of DNA. The nucleotides form a code that specifies the order of amino acids, which are the building blocks of proteins. The process of converting the genetic code into a protein is called gene expression. This process involves two main steps: transcription and translation.[2] Transcription is copying the gene's DNA sequence into a messenger RNA (mRNA) molecule.[3] Translation is decoding the mRNA sequence into a protein by the ribosomes, which are cells' protein factories.[4] After transcription and translation, a protein folds into a specific shape that determines its function.[5] This shape, or conformation, is crucial as it determines the protein's function: if a protein does not fold correctly, it may not function properly or at all. Incorrect protein folding is the basis of many diseases which are associated with misfolded proteins.[6][7][8]
CYP4F2 is part of a cluster of cytochrome P450 genes located on chromosome 19, with another closely related gene, CYP4F11, located approximately 16 kbp away.[9][10] The CYP4F2 gene is composed of no fewer than 13 exons.[9][10] The protein-coding sequence of the gene is from the second through the thirteenth exon, whereas the first exon contains a 49‑base‑pair segment forming part of the 5′ untranslated region,[10] which makes the overall genomic organization of CPY4F2 very similar to that of CYP4F3.[11]
Gene polymorphisms (variants) in CYP4F2 affect liver mRNA levels and enzymatic activity of the protein encoded.[12]
The analysis of the gene on a molecular level presents several difficulties:
- CYP4F2 is highly polymorphic, meaning that many genetic variants are present within the population; this nature makes it challenging to identify and define specific causal variants that may be responsible for certain phenotypic effects or disease associations;
- CYP4F2 is located within a cluster of genes of the CYP4F subfamily; these genes exhibit high homology and share similarities in their sequences that can lead to difficulties distinguishing between different members of the CYP4F subfamily during genetic analysis, including distinguishing between functional genes and pseudogenes (non-functional copies of genes) within this cluster;
- the genes of the CYP4F subfamily tend to be closely linked on the chromosome and inherited together due to a phenomenon called linkage disequilibrium, which means that when analyzing one gene from the subfamily, it becomes challenging to differentiate its sequence from other closely related functional genes or pseudogenes within the cluster.[13][14][12]
Protein
Proteins consist of amino acid residues and form a three-dimensional structure. Yet, the exact arrangement of atoms, also known as the crystal structure, of the enzyme CYP4F2 has not been determined. Still, researchers employ homology modeling, a method that uses the structures of similar enzymes as a template, to construct a theoretical model of CYP4F2's structure. Additionally, molecular docking has been employed to create a complex model of how CYP4F2 interacts with its substrates, to predict how the enzyme functions even without knowing its exact structure.[15]
Species
The CYP4F2 gene is widely expressed in vertebrates, including mammals, birds, amphibians, and a class of ray-finned fishes; it has been identified and studied to gain insights into its evolutionary conservation across these diverse vertebrate classes.[16]
As of 2024,[update] information regarding the presence or functional characteristics of the gene in other animal groups, such as invertebrates, is limited. Some studies have examined genes of CYP4 family in major invertebrate classes like Ascidiacea, Echinoidea, Gastropoda, and Insecta. Still, specific information about the existence of CYP4F2 specifically within these groups is not widely available.[16][17] It is assumed that CYP4 enzymes from the same subfamily have similar functions in different vertebrate species, but this assumption may not be valid, as CYP4 enzymes may have diverged in their functions, biochemical properties, and gene expression patterns over evolutionary time. To test the functional hypotheses of CYP4 enzymes in non-mammalian vertebrates, researchers can use computational methods that compare the sequences, structures, and interactions of CYP4 proteins from different species. These methods can help to identify the functional divergence, the radical biochemical changes, and the gene expression patterns.[16]
For example, one study used a computational approach to predict that the Cyp4d2 in a fruit fly (drosophila melanogaster), which is an ortholog of the human CYP4F2, may be involved in the metabolism of insect hormones and in the breakdown of synthetic insecticides.[18] An ortholog is a gene that is related by common ancestry and has the same function in different species.[19] The Cyp4d2 in the fruit fly is expressed in the malpighian tubules, which are the insect equivalent of the kidneys, and may play a role in detoxification and osmoregulation.[18] The human CYP4F2, on the other hand, is mostly expressed in the liver, duodenum, small intestine, and the kidney, and is involved in the metabolism of eicosanoids and vitamin K. Eicosanoids are a class of compounds produced in leukocytes (white blood cells) by the oxidation of arachidonic acid to regulate the immune response.[20]
Tissue and subcellular distribution
In humans, CYP4F2 is expressed in various tissues, including the liver, duodenum, small intestine, kidney, bone marrow, epididymis, and prostate,[21] with the highest expression in the liver.[22] CYP4F2 expression can be influenced by various factors, such as genetic variations, dietary intake, drug interactions, and inflammatory conditions.[23]
The CYP4F2 protein localizes to the endoplasmic reticulum (ER) of an eukariotic cell.[9] As of 2024,[update] the main subcellular location for the encoded protein CYP4F2 in human cells is not known, and is pending cell analysis.[24] ER is a continuous membrane system that forms a series of flattened sacs within the cytoplasm. The ER is divided into two domains: the rough ER, which is studded with ribosomes and is involved in protein synthesis, and the smooth ER, which is devoid of ribosomes and is involved in lipid synthesis, steroid hormone production, detoxification, and calcium storage. CYP4F2 belongs to the cytochrome P450 superfamily of enzymes which are located in the membrane of the smooth ER, where they interact with electron transfer partners, such as NADPH–cytochrome P450 reductase and cytochrome b5.[10][9] The localization of CYP4F2 to the smooth ER is important for its function and regulation, as it allows the enzyme to access its substrates and cofactors, and to be modulated by various factors, such as drugs, hormones, and dietary components.[9]
Function
The cytochrome P450 superfamily
CYP4F2 is a member of the cytochrome P450 (CYP) superfamily of enzymes.[9]
Generally, CYP enzymes are a type of protein bound to the membranes of cells, meaning they are attached to the outer layer of a cell.[10][25] They are found in many types of cells throughout the human body, but are particularly abundant in the liver. These enzymes are classified as hemoproteins, a group of proteins that contain heme, an iron-containing compound that carries oxygen. In the clinical sciences they play critical roles in the detoxification of drugs, that is the process of breakdown and removing toxic substances from the body.[26] CYP enzymes are involved in cellular metabolism, hormone synthesis, sterol and cholesterol metabolism, and are critical in maintaining homeostasis, the body's a natural ability to maintain balanced internal environment despite external changes.[10][25][26][27] Sterols are a type of lipid, or fat, and cholesterol is a specific type of sterol that is indispensable for the body's function. In humans, a significant portion of the body's metabolic processes, specifically around 80%,[28] involve oxidative metabolism, which generally makes the substrate more water-soluble and so more readily excreted by the kidneys.[26][29] CYP enzymes also participate in the elimination of drugs from the body. Approximately 50% of the breakdown and removal of common drugs used in clinical medicine can be attributed to one or more of these CYP enzymes.[25] This function is vital in ensuring that drugs are effectively used and subsequently removed from the body to prevent any potential harm.[26][25][10]
Due to their role in many biological processes such as vascular constriction, sex hormone biosynthesis, and inflammatory response, CYP enzymes can be affected by therapy with the aim of modifying the course of diseases, a concept known as disease-modifying treatment. Because of this role, they are frequently targeted in drug development, a process referred to as identifying biological targets.[30][31][32]
The CYP4F subfamily
The CYP4F subfamily of CYP enzymes exhibits diverse metabolic specificities, but is characterized by the ω-hydroxylation of very long-chain fatty acids (VLCFA), eicosanoids, lipophilic (fat-soluble) vitamins, and hydroxyeicosatetraenoic acids (HETEs).[16] The cytochrome P450 4F2 protein is an enzyme also known as "leukotriene-B4 ω-hydroxylase 1", because it starts the process of inactivating and degrading leukotriene B4 (LTB4), a potent mediator of inflammation, by ω-hydroxylating it to 20-hydroxy-LTB4.[9]
CYP4F2 and CYP4F3 catalyze the ω-hydroxylation of pro- and anti-inflammatory leukotrienes, modulating their biological activities.[11][16] CYP4F8 and CYP4F12 are involved in the metabolism of prostaglandins, endoperoxides, and arachidonic acid, regulating their inflammatory and vascular effects.[16] CYP4F11 and CYP4F12 also metabolize VLCFA and display a unique feature in the CYP4F subfamily, as they are able to hydroxylate xenobiotics such as certain amphetamines, opioids, and macrolide antibiotics.[33][16] As of 2024,[update] the functional roles of CYP4X and CYP4Z subfamilies remains not fully characterized.[10][17] CYP4X gene expression is predominantly associated with the brain and the neurovascular regions, suggesting involvement in neurological disorders. CYP4Z is mainly expressed in the mammary gland, and its expression is up-regulated in breast cancer, implying a role in tumorigenesis.[33][10][16] The CYP4 family of genes is characterized by a wide range of physiological functions of the enzymes and varied gene expression patterns. However, despite this diversity, there is a notable consistency in the structure of the substrates they act upon. This implies that while each enzyme within the CYP4 family may perform different tasks and be expressed differently, they all interact with similar types of substrates.[16]
The CYP4F subfamily plays a role in the development of cancer. Enzymes such as CYP4F2 and CYP4F3B convert arachidonic acid into 20-Hydroxyeicosatetraenoic acid (20-HETE), an eicosanoid metabolite of arachidonic acid. This metabolite impacts the progression of tumors, the formation of new blood vessels (angiogenesis), and the regulation of blood pressure in blood vessels and kidneys.[32][34]
CYP4F2 within the subfamily
As for the CYP4F2, besides its role in degrading LTB4, this enzyme is also involved in the metabolism of various endogenous substrates such as fatty acids, eicosanoids, and numerous fat-soluble vitamins.[35]
It controls the bioavailability of vitamin E.[36]
The enzyme also controls the bioavailability of Vitamin K, a co-factor required for blood to clot.[37]
Gene polymorphisms (variations) in the CYP4F2 affect enzymatic activity, i.e., the ability of the enzyme to metabolize its substrates.[37] The variations in the gene which affect the bioavailability of vitamin K also affect the dosing of vitamin K antagonists such as warfarin,[37][38][39] coumarin, or acenocoumarol.[40][41]
The enzyme also regulates the bioactivation of certain drugs, such as the anti-parasitic prodrug pafuramidine, into its active form, furamidine, by catalyzing the initial oxidative O-demethylation of pafuramidine by human liver microsomes. Pafuramidine could undergo first-pass biotransformation in the intestine, as well as in the liver.[42][43][44]
The enzyme also plays a role in renal water homeostasis.[45]
Metabolism of leukotriene B4
Biosynthesis of leukotriene B4 from arachidonic acid
Leukotriene B4 (LTB4) is a type of lipid mediator that belongs to the family of leukotrienes, which are derived from arachidonic acid by the action of 5-lipoxygenase (5-LOX).[46]
Arachidonic acid is a polyunsaturated fatty acid that is present in the phospholipids of cell membranes. It can be released from the membrane by the action of phospholipase A2, a peripheral membrane protein, which is activated by stimuli such as hormones, cytokines, growth factors and stress. Arachidonic acid can then be metabolized by three major pathways: the cyclooxygenase (COX) pathway, the lipoxygenase (LOX) pathway, and the cytochrome P450 (CYP) pathway.[47] These pathways produce different types of lipid mediators, which are collectively called eicosanoids.[46]
Eicosanoids are a group of bioactive molecules that have diverse and potent effects on physiological and pathological processes such as inflammation, immunity, pain, fever, blood pressure, blood clotting, reproduction and cancer. There are multiple types of eicosanoids, such as prostaglandins, leukotrienes, hydroxyeicosatetraenoic acids (HETEs), and so on.[20]
Leukotriene B4 (LTB4) is one of the eicosanoids that is produced by the LOX pathway. It is synthesized from arachidonic acid by the sequential actions of 5-LOX, 5-LOX activating protein (FLAP), and leukotriene A4 hydrolase (LTA4H).[46]
LTB4 is produced by activated innate immune cells, such as neutrophils, macrophages and mast cells.[48][46] It induces the activation of polymorphonuclear leukocytes, monocytes and fibroblasts, the production of superoxide and the release of cytokines to attract neutrophils.[49][50][51]
The role of leukotriene B4 in inflammatory response
LTB4 plays a key role in the initiation and maintenance of inflammation, as it can recruit and activate immune cells such as neutrophils, macrophages, mast cells, monocytes and fibroblasts. LTB4 also stimulates the production of reactive oxygen species, cytokines, chemokines and cell adhesion molecules, which further amplify the inflammatory response.[52][53]
Inactivation of leukotriene B4 by CYP4F2
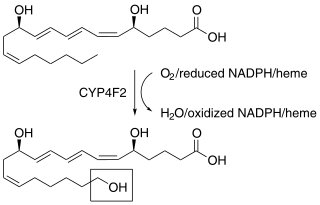
Excessive or prolonged inflammation can be harmful to the host, as it can cause tissue damage and chronic diseases, so that the inflammatory process must be tightly regulated and resolved in a timely manner. One of the mechanisms that contributes to the resolution of inflammation is the enzymatic inactivation and degradation of LTB4 by the cytochrome P450 (CYP) family of enzymes. CYP enzymes are mainly expressed in the liver, but they can also be found in other tissues, such as the lungs, kidneys, intestines, and skin.[54][55]
Among the CYP enzymes, CYP4F2 is the most important one for the metabolism of LTB4.[33][10][56]
CYP4F2 catalyzes the ω-hydroxylation of LTB4, which is the first step of its inactivation and degradation. It converts LTB4 to 20-hydroxy-LTB4, which has much lower biological activity.[57]
CYP4F2 then coverts 20-hydroxy-LTB4 to 20-oxo-LTB4 and then to 20-carboxy-LTB4,[57] which are both inactive and can be excreted from the body.[58][11]
Fatty acid ω-hydroxylation
CYP4F2 belongs to cytochrome P450 omega hydroxylase set of enzymes that catalyze the addition of a hydroxy functional group (−OH) to a molecule of the fatty acid substrate. Specifically, CYP4F2 performs ω-hydroxylation of fatty acids, which means that the functional group is added to the ω- or (ω-1)-C atom. In the context of fatty acids, the ω (omega) atom refers to the carbon atom (C) at the end of the hydrocarbon chain, furthest from the carboxyl group, so that the ω- or (ω-1)-C atom refers to the last carbon atom or the second-to-last carbon atom in the hydrocarbon chain of the fatty acid: the hydroxy group (−OH) is added to one of these atoms during the ω-hydroxylation process.[58]
The enzymes which are members of the CYP4A and CYP4F sub-families, including CYP4F2, may ω-hydroxylate and thereby reduce the activity of fatty acid metabolites of arachidonic acid such as LTB4, 5-HETE, 5-oxo-eicosatetraenoic acid, 12-HETE, and several prostaglandins. These enzymatic reactions lead to the production of metabolites involved in regulating inflammatory and vascular responses in animals and humans.[57][51] By reducing the activity of these fatty acid metabolites, ω-hydroxylation plays a role in dampening inflammatory pathways and maintaining immune system balance.[51]
Certain single-nucleotide polymorphisms (SNPs) in the CYP4F2 have been associated with human diseases like Crohn's disease[59][60] and Coeliac disease.[51][61][11] These genetic variations may impact the function or expression level of the enzyme, influencing its ability to perform ω-hydroxylation reactions effectively.[11]
The CYP4F2 enzyme also catalyzes ω-hydroxylation of 3-hydroxy fatty acids.[62] It converts monoepoxides of linoleic acid leukotoxin and isoleukotoxin to ω-hydroxylated metabolites.[63] By ω-hydroxylating 3-hydroxy fatty acids, the enzyme contributes to the modification of these molecules, which can have implications for their signaling functions in cellular processes. The production of ω-hydroxylated metabolites from monoepoxides derived from linoleic acid leukotoxin and isoleukotoxin helps regulate inflammation by reducing their activity as pro-inflammatory mediators.[62][63]
The enzyme also contributes to the degradation of VLCFAs by catalyzing successive ω-oxidations and chain shortening. This enzymatic activity ensures efficient breakdown and clearance of these fatty acids, preventing accumulation that could lead to metabolic imbalances or contribute to disease pathology.[64][65]
Fatty acid chain shortening
The process of chain shortening refers to the modification of a fatty acid molecule by removing carbon atoms from its chain. Fatty acids are organic molecules consisting of a long hydrocarbon chain, typically with an even number of carbon (C) atoms. These chains can vary in length, and their length affects their biological activities. CYP4F2 acts on fatty acids and introduces oxidative reactions that lead to the removal of carbon atoms from the chain. This process is often accompanied by the addition of oxygen to the fatty acid molecule, resulting in the formation of metabolites or breakdown products. By shortening the fatty acid chains, the CYP4F2 enzyme plays a role in vitamin metabolism. This process can affect the bioavailability, transportation, and utilization of certain fat-soluble vitamins in the body. The specific impact of chain shortening on vitamin metabolism may vary depending on the specific fatty acid and vitamin involved. This process is essential for maintaining lipid homeostasis and regulating biological activities influenced by fatty acids.[42]
Fatty acid chain shortening by CYP4F2 is performed by their α-, β-, and ω-oxidation, with the preferred pathway being the β-oxidation in the mitochondria and peroxisomes. VLCFAs cannot be β-oxidized. The number of carbon atoms in the chains of such acids exceeds 22. Such chains must be shortened before being oxidized by mitochondria. The CYP4F2 enzyme is involved in catalyzing the ω-oxidation and chain shortening of such acids.[42]
Additionally, the CYP4F2 enzyme plays a significant role in mediating the metabolism of long-chain polyunsaturated fatty acids (PUFAs), such as ω−3 and ω−6 fatty acids, which are required for physiological processes such as brain development, inflammation modulation, and cardiovascular health.[42]
Metabolism of vitamins
The enzyme plays its role in metabolism of vitamins E and K by chain shortening,[66][67] i.e., by reducing the number of carbon atoms in certain hydrocarbon chains of the molecules of the vitamin, depending on a particular vitamin molecule. This process is also known as ω-hydroxylation, because it involves adding a hydroxy group (-OH) to the last carbon atom (omega position) of the chain. This makes the vitamin molecule more polar (increase chemical polarity) and less stable, and facilitates its further degradation by other enzymes.[68][69]
CYP4F2 is the only known enzyme to ω-hydroxylate tocotrienols and tocopherols which are forms (vitamers) of vitamin E, thus making it a key regulator of circulating plasma vitamin E levels.[70][51][71] It catalyzes ω-hydroxylation of the phytyl chain of tocopherols, with preference for γ-tocopherols over α-tocopherols, thus promoting retention of α-tocopherols in tissues.[72]
Vitamin E is a collective term for eight different molecules that have antioxidant properties and protect cell membranes from oxidative damage. They are divided into two groups: tocotrienols and tocopherols. Both groups have a chromanol ring, which is the active part of the molecule, and a phytyl chain, which is a long hydrocarbon tail. CYP4F2 shortens the phytyl chain of both tocopherols and tocotrienols by ω-hydroxylation, which reduces their biological activity and stability.[72]
Vitamin K is a collective term for two natural forms of vitamin K: vitamin K1 (phylloquinone) and vitamin K2 (menaquinone).[10][73][74] Vitamin K is essential for the synthesis of several proteins involved in blood clotting and bone metabolism.[10][73] Vitamin K1 has a phytyl chain, similar to vitamin E, while vitamin K2 has an isoprenoid chain, which is a series of five-carbon units. CYP4F2 shortens the phytyl chain of vitamin K1 and the isoprenoid chain of vitamin K2 by ω-hydroxylation, which reduces their biological activity and stability.[73]
Both types of Vitamin K (K1 and K2) can be used as co-factors for γ-glutamyl carboxylase, an enzyme that catalyzes the post-translational modification of Vitamin K-dependent proteins, thus biochemically activating the proteins involved in blood coagulation and bone mineralization.[75][76]
CYP4F2 plays a pivotal role in modulating circulating levels of vitamin K1 by ω-hydroxylating and deactivating it: in the liver, where this enzyme is predominantly expressed, it functions as a primary oxidase responsible for metabolizing vitamin K1 into hydroxylated forms. By doing so, it acts synergistically with VKORC1 enzyme to prevent excessive accumulation of biologically active vitamin K in the body. Termed the "siphoning" pathway,[13] this mechanism primarily occurs when there is an excess amount of vitamin K1 present. This enzymatic process positions CYP4F2 as a critical negative regulator for maintaining appropriate levels of active vitamin K1 within the body.[73][77]
Biosynthesis of 20-HETE
CYP4F2 along with CYP4A22, CYP4A11, CYP4F3 and CYP2U1 enzymes also metabolize arachidonic acid to 20-hydroxyeicosatetraenoic acid (20-HETE) by an ω-oxidation reaction, with the predominant 20-HETE-synthesizing enzymes in humans being CYP4F2, followed by CYP4A11.[11]
One of the main roles of 20-HETE is to regulate various physiological processes within the body, such as blood flow, vascularization (or angiogenesis, that is the growth of blood vessels), maintenance of proper blood pressure, and kidney tubule absorption of ions in rodents and possibly humans.[78] By controlling blood flow and vascularization, it helps with the formation of new blood vessels when needed. To influence blood pressure levels, it regulates the diameter of blood vessels and constriction or relaxation of smooth muscles that line them. To regulate ion transport and water reabsorption in kidney tubules, it regulates how ions are absorbed or excreted by kidney cells, ultimately impacting electrolyte balance within the bodies. Research on animal models suggests that changes in levels or activity of 20-HETE may be involved in conditions such as hypertension (high blood pressure), renal diseases (kidney disorders), cerebral ischemia (reduced blood flow to the brain), and even cancer progression.[79][80][81]
The production and actions of 20-HETE can be influenced by genetic variations known in the CYP4F2 gene. These variations may alter how efficiently arachidonic acid is converted into 20-HETE, affecting its overall impact on bodily functions.[82]
Drug metabolism
Drug metabolism involves the breakdown and transformation of drugs into their active or inactive forms. The CYP4F2 enzyme plays a significant role in regulating the bioactivation of certain drugs.[39]
Specifically, the enzyme regulates the bioactivation of the anti-parasitic drug pafuramidine. Pafuramidine is a prodrug of furamidine, which means that pafuramidine requires enzymatic conversion to its bioactive form furamidine. Several studies have identified CYP4F2 as one of the key enzymes responsible for this conversion process in human liver microsomes and enteric microsomes.[83][84]
CYP4F2 is also involved in metabolism of fingolimod, a drug to treat multiple sclerosis.[85]
Clinical significance
Genetic variants
Genetic variations in CYP4F2 play a role in physiological processes and health outcomes.[37] Genetic variations in CYP4F2 are considered in personalized treatments related to drug dosages and vitamin supplementation strategies.[86]
Confirmed variations in in CYP4F2 serve as biomarkers for individual differences in response to warfarin—adjusting warfarin dosage based on genetic information has demonstrated a decrease in negative clinical outcomes.[87]
Warfarin dosing algorithms that specifically incorporate the CYP4F2 genetic variants are a subset of the broader range of warfarin dosing algorithms. As of May 2020, 92 out of 433 described warfarin dosing algorithms in the literature included CYP4F2 variants; the other covariates included in these algorithms have been age, concomitant medications, weight, and the variants in the other genes: CYP2C9 and VKORC1.[87]
One specific genetic variant which produces the enzyme with valine residue replaced to methionine residue at position 433 of the protein (V433M substitution), a single-nucleotide polymorphism denoted as CYP4F2*3[88] (rs2108622),[89] that is present in 28% of global population,[90] leads to reduced enzymetic activity due to decrease in steady-state hepatic concentrations of the enzyme.[41][36] This variant has a role in eicosanoid and Vitamin E metabolism,[71][91][36] in the bioavailability of Vitamin K,[73] in affecting doses of antigoagulants such as warfarin[37][12] or coumarin,[41] and is also associated with hypertension,[92][93] with increased risk of cerebral infarction (i.e. ischemic stroke) and myocardial infarction.[81] Individuals who carry this genetic variant, either in a homozygous form (on one chromosome) or heterozygous form (on both chromosomes), may have an increased risk of excessive anticoagulation when treated with warfarin, although not all studies confirm this association.[94] This variant accounted for a difference in warfarin dose of approximately 1 mg/day between CC and TT subjects.[87] Most of the studies on warfarin pharmacogenetics, including those involving CYP4F2, have been conducted in European ancestry patients; still, there has been significant activity in developing dosing algorithms for individuals of Asian ancestry.[87]
The CYP4F2 enzyme also regulates the bioactivation of anti-parasitic drug pafuramidine; as such, genetic variations in the CYP4F2 that alter enzyme function can impact the efficacy and safety of these drugs for patients receiving therapy. For example, individuals with a variation that leads to reduced activity of the enzyme may not fully metabolize pafuramidine, leading to lower drug concentrations and reducing its effectiveness against malaria. In contrast, variations associated with increased enzyme activity could result in faster metabolism of pafuramidine and furamidine, leading to higher than expected drug concentrations which may increase the risk of adverse effects.[42]
Drug interactions
There can be interactions between the drugs that rely on CYP4F2 on their metabolism or bioactivation (e.g., fingolimod, furamidine, warfarin)[85][95] and the substances that inhibit or induce CYP4F2 expression, such as statins and peroxisomal proliferators (drugs to lower low-density lipoproteins and reduce risk of risk of cardiovascular disease), 25-hydroxycholesterol, vitamin K, ketoconazole (an antifungal medication), sesamin (a component of sesame oil), and others.[42]
For instance, the use of ketoconazole, which is a CYP4F2 inhibitor, has been observed to cause an increase in the concentrations of fingolimod.[85]
Biological target
CYP4F2, along with the other enzymes that convert arachidonic acid to 20-HETE, can be a drug target in disease-modifying therapy for cancer. 20-HETE is a molecule that affects tumor progression, angiogenesis, and blood pressure regulation in the circulatory system and kidneys.[10][32] In the tumor microenvironment, proinflammatory cytokines can induce or inhibit CYP4F2 and other enzymes, which can promote carcinogenesis and affect chemotherapy, leading to adverse effects, toxicity, or therapeutic failure.[96][97] CYP enzymes could be targeted to modify the course of diseases like cancer.[98] Targeting CYPs in preclinical and clinical trials for chemoprevention and chemotherapy has become an effective way to improve antitumor treatment outcomes.[99] Intratumoral CYP enzymes can play a role in the fate of antitumor agents by drug activation or inactivation.[100] Still, they can also provide a mechanism for drug resistance due to their aberrant expression and their supporting roles in tumor progression and metastasis.[31][10]
History
In 1997, Heng et al. found that the human CYP4F2 gene is mapped to chromosome 19 based on analysis of monochromosomal human-rodent cell hybrids using PCR.[101]
In 1999, Kikuta et al. isolated the CYP4F2 gene and determined its genomic organization and the functional activity of its promoters. The study found that the CYP4F2 gene contains at least 13 exons, with its open reading frame being encoded from exon II to exon XIII. The structure of this gene was found to be very similar to that of CYP4F3. The study also reported that CYP4F2 is constitutively expressed in a human hepatoma cell line, HepG2, and is not induced by clofibrate. The study also observed that the human liver CYP4F2 protein plays a role in the metabolic inactivation and degradation of LTB4, a mediator of inflammation.[102][10]
In 2007, Stec et al. identified a SNP in the coding region of the CYP4F2 gene, resulting in a V433M substitution, denoted as CYP4F2*3, that was frequent in both African and European American samples (9 to 21% minor allele frequency). In vitro functional expression assays indicated that the V433M variant decreased 20-HETE production levels to 56 to 66% of control levels. In contrast, the variant had no effect on the ω-hydroxylation of LTB4. The study also reported that CYP4F2 also encodes for the major CYP enzyme responsible for the synthesis of 20-HETE in the human kidney. The study found that 20-HETE plays an important role in the regulation of renal tubular and vascular function.[50][10][34]
In 2008, Caldwell et al., referring to the V433M variant as rs2108622, indicated that it affects warfarin therapy.[101][10]
In 2010, Ross et al. genotyped 963 individuals from 7 geographic regions worldwide for the CYP4F2 V433M substitution, to understand better algorithms for warfarin dose adjustment.[14][10]
In 2023, Farajzadeh-Dehkordi et al. utilized computational analysis to investigate the V433M substitution and its association with human CYP4F2 enzyme dysfunction, using computer-based methods and bioinformatics tools to analyze complex biological data, employing 14 different bioinformatics tools. The results demonstrated that this genetic variant affects the dynamics and stability of the protein biomolecule by reducing its compactness and stability, leading to alterations in overall structural conformation and flexibility.[13]
References
- ↑ "UniProt". https://www.uniprot.org/uniprotkb/P78329/entry.
- ↑ "How do genes direct the production of proteins?: MedlinePlus Genetics" (in en). https://medlineplus.gov/genetics/understanding/howgeneswork/makingprotein/.
- ↑ "Gene Expression" (in en). https://www.genome.gov/genetics-glossary/Gene-Expression.
- ↑ "Translation: DNA to mRNA to Protein". Learn Science at Scitable. https://www.nature.com/scitable/topicpage/translation-dna-to-mrna-to-protein-393/.
- ↑ "The Shape and Structure of Proteins" (in en). Molecular Biology of the Cell (4th ed.). Garland Science. 2002. Template:NCBIBook.
- ↑ "Protein folding, misfolding and aggregation: The importance of two-electron stabilizing interactions". PLOS ONE 12 (9). 2017. doi:10.1371/journal.pone.0180905. PMID 28922400. Bibcode: 2017PLoSO..1280905C.
- ↑ "The TRiCky Business of Protein Folding in Health and Disease". Front Cell Dev Biol 10. 2022. doi:10.3389/fcell.2022.906530. PMID 35602608.
- ↑ "Rethinking the protein folding problem from a new perspective". Eur Biophys J 52 (3): 189–193. April 2023. doi:10.1007/s00249-023-01657-w. PMID 37165178.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Template:NCBI RefSeq
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 10.12 10.13 10.14 10.15 10.16 10.17 Online Mendelian Inheritance in Man (OMIM) 604426
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 "Human cytochrome P450 4F3: structure, functions, and prospects". Drug Metabol Drug Interact 27 (2): 63–71. April 2012. doi:10.1515/dmdi-2011-0037. PMID 22706230.
- ↑ 12.0 12.1 12.2 "Effect of Genetic Variability in the CYP4F2, CYP4F11, and CYP4F12 Genes on Liver mRNA Levels and Warfarin Response". Frontiers in Pharmacology 8. 2017. doi:10.3389/fphar.2017.00323. PMID 28620303.
- ↑ 13.0 13.1 13.2 "Computational analysis of missense variant CYP4F2*3 (V433M) in association with human CYP4F2 dysfunction: a functional and structural impact". BMC Molecular and Cell Biology 24 (1). May 2023. doi:10.1186/s12860-023-00479-0. PMID 37161313.
- ↑ 14.0 14.1 "CYP4F2 genetic variant alters required warfarin dose". Blood 111 (8): 4106–4112. April 2008. doi:10.1182/blood-2007-11-122010. PMID 18250228.
- ↑ "Insights into the binding mechanism between α-TOH and CYP4F2: A homology modeling, molecular docking, and molecular dynamics simulation study". J Cell Biochem 124 (4): 573–585. April 2023. doi:10.1002/jcb.30391. PMID 36924012.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 16.6 16.7 16.8 "Phylogenetic and functional analyses of the cytochrome P450 family 4". Molecular Phylogenetics and Evolution 62 (1): 458–471. January 2012. doi:10.1016/j.ympev.2011.10.016. PMID 22079551. Bibcode: 2012MolPE..62..458K.
- ↑ 17.0 17.1 "New Proluciferin Substrates for Human CYP4 Family Enzymes". Applied Biochemistry and Biotechnology 193 (1): 218–237. January 2021. doi:10.1007/s12010-020-03388-6. PMID 32869209.
- ↑ 18.0 18.1 "UniProt". https://www.uniprot.org/uniprotkb/Q27589/entry.
- ↑ "Orthologs, paralogs, and evolutionary genomics". Annual Review of Genetics 39: 309–338. 2005. doi:10.1146/annurev.genet.39.073003.114725. PMID 16285863. https://zenodo.org/record/1234975. Retrieved 25 November 2023.
- ↑ 20.0 20.1 "Eicosanoids". Essays Biochem 64 (3): 423–441. September 2020. doi:10.1042/EBC20190083. PMID 32808658. https://eprints.soton.ac.uk/443186/1/Calder_Eicosanoids_Revised_Clean.pdf. Retrieved 25 November 2023.
- ↑ "CYP4F2 protein expression summary". The Human Protein Atlas. https://www.proteinatlas.org/ENSG00000186115-CYP4F2.
- ↑ "Prostaglandin and leukotriene omega-hydroxylases". Prostaglandins & Other Lipid Mediators 68: 345–362. August 2002. doi:10.1016/s0090-6980(02)00039-4. PMID 12432928.
- ↑ "Determination of CYP450 Expression Levels in the Human Small Intestine by Mass Spectrometry-Based Targeted Proteomics". International Journal of Molecular Sciences 22 (23). November 2021. doi:10.3390/ijms222312791. PMID 34884595.
- ↑ "CYP4F2 Subcellular RNA expression". The Human Protein Atlas. https://www.proteinatlas.org/ENSG00000186115-CYP4F2/subcellular.
- ↑ 25.0 25.1 25.2 25.3 "Cytochrome P450 Enzymes and Drug Metabolism in Humans". Int J Mol Sci 22 (23). November 2021. doi:10.3390/ijms222312808. PMID 34884615.
- ↑ 26.0 26.1 26.2 26.3 "Enzyme Kinetics of Oxidative Metabolism: Cytochromes P450". Enzyme Kinetics in Drug Metabolism. Methods in Molecular Biology. 1113. Humana Press. 2014. pp. 149–166. doi:10.1007/978-1-62703-758-7_8. ISBN 978-1-62703-757-0.
- ↑ "Homeostasis | Definition, Function, Examples, & Facts | Britannica". 17 November 2023. https://www.britannica.com/science/homeostasis.
- ↑ "Inflammatory signaling on cytochrome P450-mediated drug metabolism in hepatocytes". Front Pharmacol 13. 2022. doi:10.3389/fphar.2022.1043836. PMID 36353494.
- ↑ "Cytochrome P450 Structure, Function and Clinical Significance: A Review". Curr Drug Targets 19 (1): 38–54. 2018. doi:10.2174/1389450118666170125144557. PMID 28124606.
- ↑ "Cytochrome P450 enzymes as drug targets in human disease". Drug Metab Dispos 52 (6): 493–497. October 2023. doi:10.1124/dmd.123.001431. PMID 37793784.
- ↑ 31.0 31.1 "Drug-Metabolizing Cytochrome P450 Enzymes Have Multifarious Influences on Treatment Outcomes". Clin Pharmacokinet 60 (5): 585–601. May 2021. doi:10.1007/s40262-021-01001-5. PMID 33723723.
- ↑ 32.0 32.1 32.2 "Involvement of cytochrome P450 enzymes in inflammation and cancer: a review". Cancer Chemother Pharmacol 87 (3): 295–309. March 2021. doi:10.1007/s00280-020-04181-2. PMID 33112969.
- ↑ 33.0 33.1 33.2 "Molecular Functionality of Cytochrome P450 4 (CYP4) Genetic Polymorphisms and Their Clinical Implications". Int J Mol Sci 20 (17): 4274. August 2019. doi:10.3390/ijms20174274. PMID 31480463.
- ↑ 34.0 34.1 "The Functions of Cytochrome P450 ω-hydroxylases and the Associated Eicosanoids in Inflammation-Related Diseases". Front Pharmacol 12. 2021. doi:10.3389/fphar.2021.716801. PMID 34594219.
- ↑ "CYP4F2 Gene". https://www.uniprot.org/uniprot/P78329#function.
- ↑ 36.0 36.1 36.2 "Complexity of vitamin E metabolism". World Journal of Biological Chemistry 7 (1): 14–43. February 2016. doi:10.4331/wjbc.v7.i1.14. PMID 26981194.
- ↑ 37.0 37.1 37.2 37.3 37.4 "Warfarin dosing algorithms: A systematic review". British Journal of Clinical Pharmacology 87 (4): 1717–1729. April 2021. doi:10.1111/bcp.14608. PMID 33080066.
- ↑ "Genetic Factors Influencing Warfarin Dose in Han Chinese Population: A Systematic Review and Meta-Analysis of Cohort Studies". Clinical Pharmacokinetics 62 (6): 819–833. June 2023. doi:10.1007/s40262-023-01258-y. PMID 37273173.
- ↑ 39.0 39.1 "A network meta-analysis of CYP2C9, CYP2C9 with VKORC1 and CYP2C9 with VKORC1 and CYP4F2 genotype-based warfarin dosing strategies compared to traditional". Journal of Clinical Pharmacy and Therapeutics 46 (3): 640–648. June 2021. doi:10.1111/jcpt.13334. PMID 33346393.
- ↑ "Very Important Pharmacogene: CYP4F2". PharmGKB. Stanford University. https://www.pharmgkb.org/vip/PA166169424.
- ↑ 41.0 41.1 41.2 "Effect of CYP4F2, VKORC1, and CYP2C9 in Influencing Coumarin Dose: A Single-Patient Data Meta-Analysis in More Than 15,000 Individuals". Clinical Pharmacology and Therapeutics 105 (6): 1477–1491. June 2019. doi:10.1002/cpt.1323. PMID 30506689.
- ↑ 42.0 42.1 42.2 42.3 42.4 42.5 "PharmGKB summary: very important pharmacogene information for CYP4F2". Pharmacogenetics and Genomics 25 (1): 41–47. January 2015. doi:10.1097/FPC.0000000000000100. PMID 25370453.
- ↑ "Novel amidines and analogues as promising agents against intracellular parasites: a systematic review". Parasitology 140 (8): 929–51. July 2013. doi:10.1017/S0031182013000292. PMID 23561006.
- ↑ "Cytochrome P450-activated prodrugs". Future Med Chem 5 (2): 213–28. February 2013. doi:10.4155/fmc.12.197. PMID 23360144.
- ↑ "Formation of 20-hydroxyeicosatetraenoic acid, a vasoactive and natriuretic eicosanoid, in human kidney. Role of Cyp4F2 and Cyp4A11". The Journal of Biological Chemistry 275 (6): 4118–4126. February 2000. doi:10.1074/jbc.275.6.4118. PMID 10660572.
- ↑ 46.0 46.1 46.2 46.3 "Leukotriene B4: metabolism and signal transduction". Archives of Biochemistry and Biophysics 385 (2): 231–241. January 2001. doi:10.1006/abbi.2000.2168. PMID 11368003.
- ↑ "Arachidonic Acid Metabolism and Kidney Inflammation". International Journal of Molecular Sciences 20 (15): 3683. July 2019. doi:10.3390/ijms20153683. PMID 31357612.
- ↑ "The role of leukotriene B(4) in allergic diseases". Allergology International 57 (4): 291–298. December 2008. doi:10.2332/allergolint.08-RAI-0019. PMID 18797182.
- ↑ "Cytochrome P450 4F subfamily: at the crossroads of eicosanoid and drug metabolism". Pharmacology & Therapeutics 112 (3): 589–611. December 2006. doi:10.1016/j.pharmthera.2006.03.008. PMID 16926051.
- ↑ 50.0 50.1 "Functional polymorphism in human CYP4F2 decreases 20-HETE production". Physiological Genomics 30 (1): 74–81. June 2007. doi:10.1152/physiolgenomics.00003.2007. PMID 17341693.
- ↑ 51.0 51.1 51.2 51.3 51.4 "Cytochrome P450 omega hydroxylase (CYP4) function in fatty acid metabolism and metabolic diseases". Biochemical Pharmacology 75 (12): 2263–2275. June 2008. doi:10.1016/j.bcp.2008.03.004. PMID 18433732.
- ↑ "Leukotriene B4". The International Journal of Biochemistry & Cell Biology 30 (2): 173–178. February 1998. doi:10.1016/s1357-2725(97)00123-4. PMID 9608670.
- ↑ "Leukotriene B4, an endogenous stimulator of the innate immune response against pathogens". Journal of Innate Immunity 6 (2): 159–168. 2014. doi:10.1159/000353694. PMID 23988515.
- ↑ "Essential Fatty Acids and Their Metabolites in the Pathobiology of Inflammation and Its Resolution". Biomolecules 11 (12): 1873. December 2021. doi:10.3390/biom11121873. PMID 34944517.
- ↑ "The role of the LTB4-BLT1 axis in health and disease". Pharmacological Research 158. August 2020. doi:10.1016/j.phrs.2020.104857. PMID 32439596.
- ↑ "Role of human CYP4F2 in hepatic catabolism of the proinflammatory agent leukotriene B4". Archives of Biochemistry and Biophysics 359 (1): 89–98. November 1998. doi:10.1006/abbi.1998.0880. PMID 9799565.
- ↑ 57.0 57.1 57.2 "Purification and characterization of recombinant human neutrophil leukotriene B4 omega-hydroxylase (cytochrome P450 4F3)". Archives of Biochemistry and Biophysics 355 (2): 201–205. July 1998. doi:10.1006/abbi.1998.0724. PMID 9675028.
- ↑ 58.0 58.1 "Cytochrome P450 ω-Hydroxylases in Inflammation and Cancer". Cytochrome P450 Function and Pharmacological Roles in Inflammation and Cancer. Adv Pharmacol. 74. Academic Press. 2015. pp. 223–62. doi:10.1016/bs.apha.2015.05.002. ISBN 978-0-12-803119-3.
- ↑ "Interactions between the dietary polyunsaturated fatty acid ratio and genetic factors determine susceptibility to pediatric Crohn's disease". Gastroenterology 146 (4): 929–931. April 2014. doi:10.1053/j.gastro.2013.12.034. PMID 24406470. https://zenodo.org/record/896397. Retrieved 3 July 2020.
- ↑ "Genes involved in the metabolism of poly-unsaturated fatty-acids (PUFA) and risk for Crohn's disease in children & young adults". PLOS ONE 5 (12). December 2010. doi:10.1371/journal.pone.0015672. PMID 21187935. Bibcode: 2010PLoSO...515672C.
- ↑ "A functional candidate screen for coeliac disease genes". European Journal of Human Genetics 14 (11): 1215–1222. November 2006. doi:10.1038/sj.ejhg.5201687. PMID 16835590.
- ↑ 62.0 62.1 "Omega oxidation of 3-hydroxy fatty acids by the human CYP4F gene subfamily enzyme CYP4F11". Journal of Lipid Research 49 (3): 612–624. March 2008. doi:10.1194/jlr.M700450-JLR200. PMID 18065749.
- ↑ 63.0 63.1 "Human CYP4F3s are the main catalysts in the oxidation of fatty acid epoxides". Journal of Lipid Research 45 (8): 1446–1458. August 2004. doi:10.1194/jlr.M300463-JLR200. PMID 15145985.
- ↑ "Omega-oxidation of very long-chain fatty acids in human liver microsomes. Implications for X-linked adrenoleukodystrophy". The Journal of Biological Chemistry 281 (19): 13180–13187. May 2006. doi:10.1074/jbc.M513481200. PMID 16547005.
- ↑ "Characterization of the human omega-oxidation pathway for omega-hydroxy-very-long-chain fatty acids". FASEB Journal 22 (6): 2064–2071. June 2008. doi:10.1096/fj.07-099150. PMID 18182499. https://biblio.ugent.be/publication/745741. Retrieved 3 July 2020.
- ↑ Biochemical, Physiological, and Molecular Aspects of Human Nutrition - E-Book (4th ed.). Elsevier Health Sciences. 2018. ISBN 978-0-323-40213-2. https://books.google.com/books?id=fEpVDwAAQBAJ&pg=PA711. Retrieved 4 July 2020.
- ↑ Vitamin E. MDPI - Multidisciplinary Digital Publishing Institute. 2018. p. 60. doi:10.3390/books978-3-03842-906-7. ISBN 978-3-03842-906-7. https://www.mdpi.com/books/pdfview/book/635. Retrieved 4 July 2020.
- ↑ Lipid metabolism in mammals. Springer Science & Business Media. 6 December 2012. p. 44. ISBN 978-1-4684-2832-2. https://books.google.com/books?id=mqLzBwAAQBAJ&pg=PA44. Retrieved 12 July 2020.
- ↑ Fatty Acid Metabolism and its Regulation. Elsevier. January 1984. p. 132. ISBN 0-444-80528-1. https://books.google.com/books?id=PlfcoPVDb6YC&pg=PA132. Retrieved 12 July 2020.
- ↑ "Discovery, characterization, and significance of the cytochrome P450 omega-hydroxylase pathway of vitamin E catabolism". Annals of the New York Academy of Sciences 1031 (1): 13–21. December 2004. doi:10.1196/annals.1331.002. PMID 15753130. Bibcode: 2004NYASA1031...13P.
- ↑ 71.0 71.1 "Common variants of cytochrome P450 4F2 exhibit altered vitamin E-{omega}-hydroxylase specific activity". The Journal of Nutrition 140 (11): 1901–1906. November 2010. doi:10.3945/jn.110.128579. PMID 20861217.
- ↑ 72.0 72.1 "Cytochrome P450 omega-hydroxylase pathway of tocopherol catabolism. Novel mechanism of regulation of vitamin E status". The Journal of Biological Chemistry 277 (28): 25290–25296. July 2002. doi:10.1074/jbc.M201466200. PMID 11997390.
- ↑ 73.0 73.1 73.2 73.3 73.4 "Impact of the CYP4F2 p.V433M polymorphism on coumarin dose requirement: systematic review and meta-analysis". Clinical Pharmacology and Therapeutics 92 (6): 746–756. December 2012. doi:10.1038/clpt.2012.184. PMID 23132553.
- ↑ "Vitamin K2 in electron transport system: are enzymes involved in vitamin K2 biosynthesis promising drug targets?". Molecules 15 (3): 1531–53. March 2010. doi:10.3390/molecules15031531. PMID 20335999.
- ↑ "Vitamin K-Dependent Biosynthesis of γ-Carboxyglutamic Acid". Blood 93 (6): 1798–1808. 1999. doi:10.1182/blood.V93.6.1798.406k22_1798_1808. PMID 10068650.
- ↑ "Vitamin K and the Vitamin K-dependent Proteins involved in Haemostasis". 9 May 2024. https://practical-haemostasis.com/Useful%20information/Vitamin%20K%20%26%20Vitamin%20K-dependent%20Factors.html.
- ↑ "CYP4F2 is a vitamin K1 oxidase: An explanation for altered warfarin dose in carriers of the V433M variant". Molecular Pharmacology 75 (6): 1337–1346. June 2009. doi:10.1124/mol.109.054833. PMID 19297519.
- ↑ "Vascular actions of 20-HETE". Prostaglandins & Other Lipid Mediators 120: 9–16. July 2015. doi:10.1016/j.prostaglandins.2015.03.002. PMID 25813407.
- ↑ "The CYP/20-HETE/GPR75 axis in hypertension". New Targets for the Treatment of Hypertension and Associated Diseases. Adv Pharmacol. 94. Academic Press. 2022. pp. 1–25. doi:10.1016/bs.apha.2022.02.003. ISBN 978-0-323-91087-3.
- ↑ "Vascular contributions to cognitive impairment and dementia: the emerging role of 20-HETE". Clinical Science 135 (15): 1929–1944. August 2021. doi:10.1042/CS20201033. PMID 34374423.
- ↑ 81.0 81.1 "Conflicting Roles of 20-HETE in Hypertension and Stroke". International Journal of Molecular Sciences 20 (18): 4500. September 2019. doi:10.3390/ijms20184500. PMID 31514409.
- ↑ "Eicosanoids via CYP450 and cardiovascular disease: Hints from genetic and nutrition studies". Prostaglandins & Other Lipid Mediators 139: 41–47. November 2018. doi:10.1016/j.prostaglandins.2018.10.001. PMID 30296490.
- ↑ "Human enteric microsomal CYP4F enzymes O-demethylate the antiparasitic prodrug pafuramidine". Drug Metabolism and Disposition 35 (11): 2067–2075. November 2007. doi:10.1124/dmd.107.016428. PMID 17709372.
- ↑ "CYP4F enzymes are the major enzymes in human liver microsomes that catalyze the O-demethylation of the antiparasitic prodrug DB289 [2,5-bis(4-amidinophenyl)furan-bis-O-methylamidoxime"]. Drug Metabolism and Disposition 34 (12): 1985–1994. December 2006. doi:10.1124/dmd.106.010587. PMID 16997912.
- ↑ 85.0 85.1 85.2 "Clinical pharmacokinetics of fingolimod". Clin Pharmacokinet 51 (1): 15–28. January 2012. doi:10.2165/11596550-000000000-00000. PMID 22149256.
- ↑ "Warfarin dosing strategies evolution and its progress in the era of precision medicine, a narrative review". International Journal of Clinical Pharmacy 44 (3): 599–607. June 2022. doi:10.1007/s11096-022-01386-8. PMID 35247148.
- ↑ 87.0 87.1 87.2 87.3 "Being precise with anticoagulation to reduce adverse drug reactions: are we there yet?". Pharmacogenomics J 24 (2). March 2024. doi:10.1038/s41397-024-00329-y. PMID 38443337.
- ↑ "PharmGKB". https://www.pharmgkb.org/haplotype/PA165860687.
- ↑ Template:NCBI RefSNP
- ↑ Template:NCBI RefSNP
- ↑ "Genome-wide association study identifies common variants associated with circulating vitamin E levels". Human Molecular Genetics 20 (19): 3876–3883. October 2011. doi:10.1093/hmg/ddr296. PMID 21729881.
- ↑ "Association Between the CYP4F2 Gene rs1558139 and rs2108622 Polymorphisms and Hypertension: A Meta-Analysis". Genetic Testing and Molecular Biomarkers 23 (5): 342–347. May 2019. doi:10.1089/gtmb.2018.0202. PMID 30932691.
- ↑ "Association of the CYP4F2 rs2108622 genetic polymorphism with hypertension: a meta-analysis". Genetics and Molecular Research 14 (4): 15133–15139. November 2015. doi:10.4238/2015.November.25.1. PMID 26634476.
- ↑ "PharmGKB". https://www.pharmgkb.org/clinicalAnnotation/1449269278.
- ↑ "The revised human liver cytochrome P450 "Pie": absolute protein quantification of CYP4F and CYP3A enzymes using targeted quantitative proteomics". Drug Metab Dispos 42 (8): 1241–51. August 2014. doi:10.1124/dmd.114.058040. PMID 24816681.
- ↑ "The Inflammatory Profile of the Tumor Microenvironment, Orchestrated by Cyclooxygenase-2, Promotes Epithelial-Mesenchymal Transition". Front Oncol 11. 2021. doi:10.3389/fonc.2021.686792. PMID 34178680.
- ↑ "Chronic inflammation and cytokines in the tumor microenvironment". J Immunol Res 2014. 2014. doi:10.1155/2014/149185. PMID 24901008.
- ↑ "Targeting drug-metabolizing enzymes for effective chemoprevention and chemotherapy". Drug Metab Dispos 38 (4): 539–44. April 2010. doi:10.1124/dmd.109.031351. PMID 20233842.
- ↑ "Cytochrome P450 3A4, 3A5, and 2C8 expression in breast, prostate, lung, endometrial, and ovarian tumors: relevance for resistance to taxanes". Cancer Chemother Pharmacol 84 (3): 487–499. September 2019. doi:10.1007/s00280-019-03905-3. PMID 31309254.
- ↑ "Epigenetic modulation of antitumor immunity for improved cancer immunotherapy". Mol Cancer 20 (1). December 2021. doi:10.1186/s12943-021-01464-x. PMID 34930302.
- ↑ 101.0 101.1 "A novel murine P-450 gene, Cyp4a14, is part of a cluster of Cyp4a and Cyp4b, but not of CYP4F, genes in mouse and humans". The Biochemical Journal 325 (Pt 3): 741–749. August 1997. doi:10.1042/bj3250741. PMID 9271096.
- ↑ "Expression and molecular cloning of human liver leukotriene B4 omega-hydroxylase (CYP4F2) gene". DNA and Cell Biology 18 (9): 723–730. September 1999. doi:10.1089/104454999315006. PMID 10492403.
 |
