Chemistry:Miltefosine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Impavido, Miltex, others |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | High |
| Protein binding | ~98% |
| Metabolism | Slow hepatic (non-CYP-dependent) |
| Elimination half-life | 6 to 8 days and 31 days[1] |
| Excretion | Primarily fecal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| Chemical and physical data | |
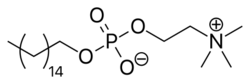
| Formula | C21H46NO4P |
| Molar mass | 407.576 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 232 to 234 °C (450 to 453 °F) |
| |
| |
| | |
Miltefosine, sold under the trade name Impavido among others, is a medication mainly used to treat leishmaniasis and free-living amoeba infections such as Naegleria fowleri and Balamuthia mandrillaris.[2] This includes the three forms of leishmaniasis: cutaneous, visceral and mucosal.[3] It may be used with liposomal amphotericin B or paromomycin.[4] It is taken by mouth.[3]
Common side effects include vomiting, abdominal pain, fever, headaches, and decreased kidney function.[2] More severe side effects may include Stevens–Johnson syndrome or low blood platelets.[2] Use during pregnancy appears to cause harm to the baby and use during breastfeeding is not recommended.[2] How it works is not entirely clear.[2]
Miltefosine was first made in the early 1980s and studied as a treatment for cancer.[5] A few years later it was found to be useful for leishmaniasis and was approved for this use in 2002 in India.[6] It is on the World Health Organization's List of Essential Medicines.[7][8]
Medical uses
Leishmaniasis
Miltefosine is primarily used for the treatment of visceral and New World cutaneous leishmaniasis, and is undergoing clinical trials for this use in several countries.[9][10] This drug is now listed as a core medication for the treatment of leishmaniasis under the WHO Model List of Essential Medicines.[11] Several medical agents have some efficacy against visceral or cutaneous leishmaniasis, however, a 2005 survey concluded that miltefosine is the only effective oral treatment for both forms of leishmaniasis.[12]
Amoeba infections
Miltefosine has been used successfully in some cases of the very rare, but highly lethal, brain infection by the amoeba, Naegleria fowleri, acquired through water entering the nose during a plunge in contaminated water.[13] It has orphan drug status in the United States for acanthamoeba keratitis and primary amebic meningoencephalitis (PAM).[14][15]
Pregnancy and breastfeeding
Miltefosine is listed as pregnancy category D by the FDA. This means there is evidence-based adverse reaction data from investigational or marketing experience or studies in humans of harm to the human fetus.[16] Despite this evidence, the potential benefits of miltefosine may warrant use of the drug in pregnant women despite potential risks. A pregnancy test should be done prior to starting treatment. Effective birth control should be used while on miltefosine and 5 months after discontinuation of treatment. Its use during breast feeding is most likely unsafe.[1]
Contraindications
Miltefosine is contraindicated in individuals who have a hypersensitivity to this medication, pregnant women, and people who have the Sjögren-Larsson syndrome.[17] It is embryotoxic and fetotoxic in rats and rabbits, and teratogenic in rats but not in rabbits. It is therefore contraindicated for use during pregnancy, and contraception is required beyond the end of treatment in women of child-bearing age.[18]
Side effects
Common side effects from miltefosine treatment are nausea and vomiting, which occur in 60% of people. Other common side effects are dizziness, headache, and daytime sleepiness.[19]
Serious side effects include rash, diarrhea, and arthritis.[19] The side effects are more severe in women and young children. The overall effects are quite mild and easily reversed.[20]
Mechanism of action
Miltefosine primarily acts on Leishmania by affecting the species's promastigote and amastigote stages.[21] Miltefosine exerts its activity by interacting with lipids, inhibiting cytochrome c oxidase and causing apoptosis-like cell death.[22] This may affect membrane integrity and mitochondrial function of the parasite.[citation needed]
History
Cancer
While initially studied as a cancer medication, due to side effects it was never used for this purpose.[23]
Phospholipid group alkylphosphocholine were known since the early 1980s, particularly in terms of their binding affinity with cobra venom.[24] In 1987 the phospholipids were found to be potent toxins on leukemic cell culture.[25] Initial in vivo investigation on the antineoplastic activity showed positive result, but then only at high dosage and at high toxicity.[26] At the same time in Germany, Hansjörg Eibl, at the Max Planck Institute for Biophysical Chemistry, and Clemens Unger, at the University of Göttingen, demonstrated that the antineoplastic activity of the phospholipid analogue miltefosine (at the time known as hexadecylphosphocholine) was indeed tumour-specific. It was highly effective against methylnitrosourea-induced mammary carcinoma, but less so on transplantable mammary carcinomas and autochthonous benzo(a)pyrene-induced sarcomas, and relatively inactive on Walker 256 carcinosarcoma and autochthonous acetoxymethylmethylnitrosamine-induced colonic tumors of rats.[27][28] It was subsequently found that miltefosine was structurally unique among lipids having anticancer property in that it lacks the glycerol group, is highly selective on cell types and acts through different mechanism.[29][30]
Leishmaniasis
In the same year as the discovery of the anticancer property, miltefosine was reported by S. L. Croft and his team at the London School of Hygiene and Tropical Medicine as having antileishmanial effect as well. The compound was effective against Leishmania donovani amastigotes in cultured mouse peritoneal macrophages at a dose of 12.8 mg/kg/day in a five-day course.[31] However, priority was given to the development of the compound for cutaneous metastases of breast cancer. In 1992 a new research was reported in which the compound was highly effective in mouse against different life cycle stages of different Leishmania species, and in fact, more potent than the conventional sodium stibogluconate therapy by a factor of more than 600.[32] Results of the first clinical trial in humans were reported from Indian patients with chronic leishmaniasis with high degree of success and safety.[33] This promising development promulgated a unique public–private partnership collaboration between ASTA Medica (later Zentaris GmbH), the World Health Organization (WHO) Special Programme for Research and Training in Tropical Diseases, and the Government of India. Eventually, several successful Phase II and III trials led to the approval of miltefosine in 2002 as the first and only oral drug for leishmaniasis.[1]
Naegleria fowleri and Acanthamoeba
In 2013, the US Centers for Disease Control and Prevention recommended miltefosine for the treatment of free-living amoeba infections such as granulomatous amoebic encephalitis and primary amoebic meningoencephalitis, two fatal protozoal diseases.[34] Historically, only four survivors have been recorded out of 138 confirmed infections in North America. One American survived the infection in 1978 and one individual from Mexico in 2003. In 2013, two children survived and recovered from primary amoebic meningoencephalitis after treatment with miltefosine.[35][36] In 2016 after treatment that included miltefosine, another child became the fourth person in the United States to survive Naegleria fowleri infection.[37]
Society and culture
Availability
Since 2017 Miltefosine is commercially available in the United States through Profounda.[38] Previously one could only get it from the CDC for emergency use under an expanded access IND protocol for treatment of free-living amoeba (FLA) infections: primary amoebic meningoencephalitis caused by Naegleria fowleri and granulomatous amoebic encephalitis caused by Balamuthia mandrillaris and Acanthamoeba species.[35] Miltefosine is almost exclusively produced by Profounda, a private pharmaceutical company.[39]
Economics
In the developing world a course of treatment costs US$65 to $150.[4] In the developed world treatment may be 10 to 50 times greater.[4]
Further research
It is active against some bacteria and fungi,[1][40] as well as human trematode Schistosoma mansoni and the snail that spreads it Biomphalaria alexandrina.[41]
Antiprotozoal and antifungal activities
Miltefosine is being investigated by researchers interested in finding treatments for infections which have become resistant to existing drugs. Animal and in vitro studies suggest it may have broad anti-protozoal and anti-fungal properties:
- Animal studies suggest miltefosine may also be effective against Trypanosoma cruzi, the parasite responsible for Chagas' disease.[42]
- Several studies have found the drug to be effective against types of fungus: Cryptococcus neoformans, Candida, Aspergillus and Fusarium.[43]
- A 2006 in vitro study found that miltefosine is effective against metronidazole-resistant variants of Trichomonas vaginalis, a sexually transmitted protozoal disease.[44]
- Cetrimonium bromide, a compound related to miltefosine, was demonstrated in 2007 to exhibit potent in vitro activity against Plasmodium falciparum.[45]
- An in vitro test in 2006 showed that miltefosine is effective against the deadly protozoan pathogens, Naegleria fowleri, Balamuthia mandrillaris, and Acanthamoeba.[46] However, later in vitro and animal model experiments showed that it is not as potent as other drugs, such as chlorpromazine[47] and diminazene aceturate (Berenil).[48]
- In 2013, there were reports of failure of miltefosine in the treatment of leishmaniasis.[49][50] Although drug resistance was suspected, studies in 2014 reported that miltefosine is not so effective in children, most probably related to a lack of drug exposure in children.[51] Moverover, males appeared to have a higher probability of relapse as well.[52]
- A 2012 in vitro study found that miltefosine had promising activity against Candida albicans biofilms.[53]
Anti-HIV activity
Miltefosine targets HIV infected macrophages, which play a role in vivo as long-lived HIV-1 reservoirs. The HIV protein Tat activates pro-survival PI3K/Akt pathway in primary human macrophages. Miltefosine acts by inhibiting the PI3K/Akt pathway, thus removing the infected macrophages from circulation, without affecting healthy cells.[54][55] It significantly reduces replication of HIV-1 in cocultures of human dendritic cells (DCs) and CD4+ T cells, which is due to a rapid secretion of soluble factors and is associated with induction of type-I interferon (IFN) in the human cells.[56]
References
- ↑ 1.0 1.1 1.2 1.3 "Miltefosine: a review of its pharmacology and therapeutic efficacy in the treatment of leishmaniasis". The Journal of Antimicrobial Chemotherapy 67 (11): 2576–2597. November 2012. doi:10.1093/jac/dks275. PMID 22833634.
- ↑ 2.0 2.1 2.2 2.3 2.4 "Miltefosine Monograph for Professionals". 26 February 2016. https://www.drugs.com/monograph/miltefosine.html.
- ↑ 3.0 3.1 "FDA approves Impavido to treat tropical disease leishmaniasis". U.S. Food and Drug Administration (FDA) (Press release). 19 March 2014. Archived from the original on 3 September 2014. Retrieved 30 August 2014.
- ↑ 4.0 4.1 4.2 Control of the leishmaniasis: report of a meeting of the WHO Expert Committee on the Control of Leishmaniases. World Health Organization. March 2010. pp. 59, 88, 186. ISBN 9789241209496.
- ↑ Antimicrobial Drugs: Chronicle of a Twentieth Century Medical Triumph. OUP Oxford. 2008. p. 310. ISBN 9780199534845. https://books.google.com/books?id=i4_FZHmzjzwC&pg=PA310.
- ↑ Leishmania and Leishmaniasis. Springer Science & Business Media. 2013. p. 39. ISBN 9781461488699. https://books.google.com/books?id=5eG5BAAAQBAJ&pg=PA39.
- ↑ World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. 2019. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. 2021. WHO/MHP/HPS/EML/2021.02.
- ↑ "Hospital de Doenças Tropicais testa droga contra calazar" (in pt). Sapiência (Fundação de Amparo à Pesquisa do Estado do Piauí). September 2005. http://www.fapepi.pi.gov.br/sapiencia6/pesquisa3.php.
- ↑ "Treatment of New World cutaneous leishmaniasis with miltefosine". Transactions of the Royal Society of Tropical Medicine and Hygiene 100 (Suppl 1): S34–S40. December 2006. doi:10.1016/j.trstmh.2006.02.022. PMID 16930649. https://zenodo.org/record/1259409.
- ↑ "19th WHO Model List of Essential Medicines". WHO. 2015. https://www.who.int/medicines/publications/essentialmedicines/EML2015_8-May-15.pdf.
- ↑ "Clinical status of agents being developed for leishmaniasis". Expert Opinion on Investigational Drugs 14 (11): 1337–1346. November 2005. doi:10.1517/13543784.14.11.1337. PMID 16255674. https://zenodo.org/record/1236265.
- ↑ "Successful treatment of an adolescent with Naegleria fowleri primary amebic meningoencephalitis". Pediatrics 135 (3): e744–e748. March 2015. doi:10.1542/peds.2014-2292. PMID 25667249.
- ↑ "Profounda Inc. receives FDA orphan-drug designation for the Treatment of Primary Amebic Meningoencephalitis (PAM) with Miltefosine". Profounda Inc. (Press release). Archived from the original on 2016-12-22. Retrieved 2017-05-25 – via www.prnewswire.com.
- ↑ "FDA Orphan Drug Designation Granted to Profounda Inc. for the treatment of Acanthamoeba Keratitis with miltefosine.". Profounda Inc.. http://www.prnewswire.com/news-releases/fda-orphan-drug-designation-granted-to-profounda-inc-for-the-treatment-of-acanthamoeba-keratitis-with-miltefosine-300380273.html.
- ↑ "New FDA Pregnancy Categories Explained". Drugs.com. https://www.drugs.com/pregnancy-categories.html.
- ↑ "Impavido- miltefosine capsule". Profounda, Inc.. 5 June 2019. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=bcb387ac-2e90-4f5e-94b2-d3635190678e.
- ↑ "Development of miltefosine as an oral treatment for leishmaniasis". Transactions of the Royal Society of Tropical Medicine and Hygiene 100 (Suppl 1): S17–S20. December 2006. doi:10.1016/j.trstmh.2006.02.010. PMID 16730362.
- ↑ 19.0 19.1 "Miltefosine Side Effects in Detail". Drugs.com. https://www.drugs.com/sfx/miltefosine-side-effects.html.
- ↑ "Drug therapy of leishmaniasis". Textbook of Pharmacology. Elsevier India. 2008. p. 31. ISBN 9788131211588. https://books.google.com/books?id=51ozlZRBvQwC.
- ↑ "Impavido New FDA Drug Approval". CenterWatch. http://www.centerwatch.com/drug-information/fda-approved-drugs/drug/1311/impavido-miltefosine.
- ↑ "Miltefosine (Impravido) for the Treatment of Visceral, Mucosal and Cutaneous Leishmaniasis". U.S. Food and Drug Administration. https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/Anti-InfectiveDrugsAdvisoryCommittee/UCM371074.pdf.
- ↑ Infectious Diseases. Elsevier Health Sciences. 2016. p. 1367. ISBN 9780702063381. https://books.google.com/books?id=Dhq3DAAAQBAJ&pg=PA1367.
- ↑ "Bindings of cobra venom phospholipases A2 to micelles of n-hexadecylphosphorylcholine". Journal of Biochemistry 94 (1): 223–232. July 1983. doi:10.1093/oxfordjournals.jbchem.a134333. PMID 6619110.
- ↑ "Metabolism of ether phospholipids and analogs in neoplastic cells". Lipids 22 (11): 856–861. November 1987. doi:10.1007/bf02535544. PMID 3444378.
- ↑ "Therapeutic ratio of mono or combination bacterial lipopolysaccharide therapy in methylnitrosourea-induced rat mammary carcinoma". Journal of Cancer Research and Clinical Oncology 113 (5): 437–445. 1987. doi:10.1007/bf00390037. PMID 3624299.
- ↑ "Alkyl phosphocholines: toxicity and anticancer properties". Lipids 22 (11): 930–934. November 1987. doi:10.1007/bf02535558. PMID 3444388.
- ↑ "New cytostatics with experimentally different toxic profiles". Cancer Treatment Reviews 14 (3–4): 307–317. December 1987. doi:10.1016/0305-7372(87)90023-5. PMID 3440252.
- ↑ "Hexadecylphosphocholine: a new and selective antitumor drug". Cancer Treatment Reviews 17 (2–3): 233–242. September 1990. doi:10.1016/0305-7372(90)90053-i. PMID 2272038.
- ↑ "Characterization of the antitumor activity of hexadecylphosphocholine (D 18506)". European Journal of Cancer & Clinical Oncology 24 (9): 1457–1461. September 1988. doi:10.1016/0277-5379(88)90336-7. PMID 3141197.
- ↑ "The activity of alkyl phosphorylcholines and related derivatives against Leishmania donovani". Biochemical Pharmacology 36 (16): 2633–2636. August 1987. doi:10.1016/0006-2952(87)90543-0. PMID 3606662.
- ↑ "Hexadecylphosphocholine: oral treatment of visceral leishmaniasis in mice". Antimicrobial Agents and Chemotherapy 36 (8): 1630–1634. August 1992. doi:10.1128/AAC.36.8.1630. PMID 1329624.
- ↑ "Trial of oral miltefosine for visceral leishmaniasis". Lancet 352 (9143): 1821–1823. December 1998. doi:10.1016/S0140-6736(98)04367-0. PMID 9851383.
- ↑ Centers for Disease Control and Prevention (CDC) (August 2013). "Investigational drug available directly from CDC for the treatment of infections with free-living amebae". MMWR. Morbidity and Mortality Weekly Report 62 (33): 666. PMID 23965830. PMC 4604798. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6233a4.htm.
- ↑ 35.0 35.1 "Naegleria fowleri - Primary Amebic Meningoencephalitis (PAM)". Centers for Disease Control and Prevention. 2014. https://www.cdc.gov/parasites/naegleria/treatment.html.
- ↑ "Brain-Eating Amoeba: How One Girl Survived". livescience. 14 August 2013. http://www.livescience.com/38897-how-to-survive-a-brain-eating-amoeba.html.
- ↑ "Rare recovery: Florida teen survives brain-eating amoeba". CNN. http://www.cnn.com/2016/08/23/health/brain-eating-amoeba-florida-teen-survives/.
- ↑ "Profounda, Inc. launches Impavido (miltefosine), the first and only oral Rx treatment for visceral, mucosal and cutaneous leishmaniasis, in the United States". Profounda Inc. (Press release). Archived from the original on 2017-03-16. Retrieved 2017-05-25 – via www.prnewswire.com.
- ↑ "A life-saving drug that treats a rare infection is almost impossible to find". 17 September 2016. http://www.businessinsider.com/why-brain-eating-amoeba-miltefosine-medicine-is-hard-to-find-2016-9?amp.
- ↑ "Alkylphospholipids - a promising class of chemotherapeutic agents with a broad pharmacological spectrum". Journal of Pharmacy & Pharmaceutical Sciences 16 (5): 742–759. 2013. doi:10.18433/J3CW23. PMID 24393556.
- ↑ "Bioactivity of miltefosine against aquatic stages of Schistosoma mansoni, Schistosoma haematobium and their snail hosts, supported by scanning electron microscopy". Parasites & Vectors 4 (1): 73. May 2011. doi:10.1186/1756-3305-4-73. PMID 21569375.
- ↑ "Proinflammatory and cytotoxic effects of hexadecylphosphocholine (miltefosine) against drug-resistant strains of Trypanosoma cruzi". Antimicrobial Agents and Chemotherapy 46 (11): 3472–3477. November 2002. doi:10.1128/AAC.46.11.3472-3477.2002. PMID 12384352.
- ↑ "Hexadecylphosphocholine (miltefosine) has broad-spectrum fungicidal activity and is efficacious in a mouse model of cryptococcosis". Antimicrobial Agents and Chemotherapy 50 (2): 414–421. February 2006. doi:10.1128/AAC.50.2.414-421.2006. PMID 16436691.
- ↑ "In vitro activity of hexadecylphosphocholine (miltefosine) against metronidazole-resistant and -susceptible strains of Trichomonas vaginalis". The Journal of Antimicrobial Chemotherapy 57 (2): 273–278. February 2006. doi:10.1093/jac/dki417. PMID 16344287.
- ↑ "Inhibition of Plasmodium falciparum choline kinase by hexadecyltrimethylammonium bromide: a possible antimalarial mechanism". Antimicrobial Agents and Chemotherapy 51 (2): 696–706. February 2007. doi:10.1128/AAC.00919-06. PMID 17145794.
- ↑ "In-vitro activity of miltefosine and voriconazole on clinical isolates of free-living amebas: Balamuthia mandrillaris, Acanthamoeba spp., and Naegleria fowleri". The Journal of Eukaryotic Microbiology 53 (2): 121–126. 2006. doi:10.1111/j.1550-7408.2005.00082.x. PMID 16579814.
- ↑ "Effect of therapeutic chemical agents in vitro and on experimental meningoencephalitis due to Naegleria fowleri". Antimicrobial Agents and Chemotherapy 52 (11): 4010–4016. November 2008. doi:10.1128/AAC.00197-08. PMID 18765686.
- ↑ "The in vitro efficacy of antimicrobial agents against the pathogenic free-living amoeba Balamuthia mandrillaris". The Journal of Eukaryotic Microbiology 60 (5): 539–543. 2013. doi:10.1111/jeu.12062. PMID 23869955.
- ↑ "Increasing failure of miltefosine in the treatment of Kala-azar in Nepal and the potential role of parasite drug resistance, reinfection, or noncompliance". Clinical Infectious Diseases 56 (11): 1530–1538. June 2013. doi:10.1093/cid/cit102. PMID 23425958.
- ↑ "Relapse after treatment with miltefosine for visceral leishmaniasis is associated with increased infectivity of the infecting Leishmania donovani strain". mBio 4 (5): e00611–e00613. October 2013. doi:10.1128/mBio.00611-13. PMID 24105765.
- ↑ "Failure of miltefosine in visceral leishmaniasis is associated with low drug exposure". The Journal of Infectious Diseases 210 (1): 146–153. July 2014. doi:10.1093/infdis/jiu039. PMID 24443541.
- ↑ "Failure of miltefosine treatment for visceral leishmaniasis in children and men in South-East Asia". PLOS ONE 9 (6): e100220. 2014. doi:10.1371/journal.pone.0100220. PMID 24941345. Bibcode: 2014PLoSO...9j0220O.
- ↑ "Effect of alkylphospholipids on Candida albicans biofilm formation and maturation". The Journal of Antimicrobial Chemotherapy 68 (1): 113–125. January 2013. doi:10.1093/jac/dks353. PMID 22995097.
- ↑ "Akt inhibitors as an HIV-1 infected macrophage-specific anti-viral therapy". Retrovirology 5 (1): 11. January 2008. doi:10.1186/1742-4690-5-11. PMID 18237430.
- ↑ "Parasitic Drug Shows HIV-Fighting Promise". AIDSmeds.com. 2008-02-01. http://www.aidsmeds.com/articles/hiv_miltefosine_macrophages_1667_13933.shtml.
- ↑ "Miltefosine represses HIV-1 replication in human dendritic cell/T-cell cocultures partially by inducing secretion of type-I interferon". Virology 432 (2): 271–276. October 2012. doi:10.1016/j.virol.2012.05.032. PMID 22704066.
External links
- "Miltefosine". Drug Information Portal. U.S. National Library of Medicine. https://druginfo.nlm.nih.gov/drugportal/name/miltefosine.
- "Miltefosine". Drugs.com. https://www.drugs.com/international/miltefosine.html.
 |
