Biology:Calcitonin gene-related peptide
Calcitonin gene-related peptide (CGRP) is a member of the calcitonin family of peptides consisting of calcitonin, amylin, adrenomedullin, adrenomedullin 2 (intermedin) and calcitonin‑receptor‑stimulating peptide. Calcitonin is mainly produced by thyroid C cells whilst CGRP is secreted and stored in the nervous system.[1] This peptide, in humans, exists in two forms: CGRP alpha (α-CGRP or CGRP I), and CGRP beta (β-CGRP or CGRP II).[2] α-CGRP is a 37-amino acid neuropeptide and is formed by alternative splicing[3] of the calcitonin/CGRP gene located on chromosome 11. β-CGRP is less studied. In humans, β-CGRP differs from α-CGRP by three amino acids and is encoded in a separate, nearby gene.[4] The CGRP family includes calcitonin (CT), adrenomedullin (AM), and amylin (AMY).[5]
Function
CGRP is produced in both peripheral and central neurons.[6] It is a potent peptide vasodilator and can function in the transmission of nociception.[7][8] In the spinal cord, the function and expression of CGRP may differ depending on the location of synthesis. CGRP is derived mainly from the cell bodies of motor neurons when synthesized in the ventral horn of the spinal cord and may contribute to the regeneration of nervous tissue after injury. Conversely, CGRP is derived from dorsal root ganglion when synthesized in the dorsal horn of the spinal cord and may be linked to the transmission of pain.[9] In the trigeminal vascular system, the cell bodies on the trigeminal ganglion are the main source of CGRP. CGRP is thought to play a role in cardiovascular homeostasis and nociception. In the heart, CGRP acts as a chronotrope by increasing heart rate.[10]:202 Apart from these attributes, CGRP is known to modulate the autonomic nervous system and plays a role in ingestion.[10]:201–204
CGRP has moderate effects on calcium homeostasis compared to its extensive actions in other areas, such as the autonomic nervous system.
Appetite
As a neuropeptide, CGRP acts as an appetite suppressant and contributes to gastric acid secretion.[10] It also functions in temperature homeostasis, increases heart rate, and plays a role in the release of the pituitary hormones in a paracrine manner.[10] Because of these characteristics, it has been said that CGRP functions more as a neurotransmitter than a hormone.[10]
Stem cell mobilization
CGRP has a role in human stem cells mobilization. In investigations carried out during last five years, treatment with CGRP resulted in significantly increased CGRP levels in the bone marrow extracellular fluid and substantially increased the number of HSCs mobilized by G-CSF.[11] The results performed on different experiments by the same research group led to the conclusion that G-CSF-induced HSC mobilization is regulated by the nociceptor nerve-derived neuropeptide CGRP. This peptide exerts its effect on HSC mobilization by Ramp 1 pathway.[11]
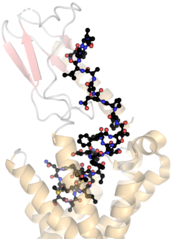
Receptors
CGRP mediates its effects through a heteromeric receptor composed of a G protein-coupled receptor called calcitonin receptor-like receptor (CALCRL) and a receptor activity-modifying protein (RAMP1).[12] CGRP receptors are found throughout all the body, suggesting that the protein may modulate a variety of physiological functions in all major systems (e.g., respiratory, endocrine, gastrointestinal, immune, and cardiovascular).[13] The extracellular loop number 2 is fundamental for ligand induced activation, with key interactions of R274/Y278/D280/W283.[14]
Regulation
Regulation of the calcitonin gene-related peptide (CGRP) gene is in part controlled by the expression of the mitogen-activated protein kinases (MAPK) signaling pathway,[15] cytokines such as TNFα[16] and iNOS.[17]
5HT1 receptor agonists, such as sumatriptan, increase intracellular calcium, which cause decreases in CGRP promoter activity.[15]
CGRP receptor is found in myelinated A-fibers axon which is required for ligand specificity and function of the receptor. The CGRP receptor has three subunits: receptor activity-modifying protein 1 (RAMP1), calcitonin-like receptor (CLR) and receptor component protein (RCP).[18] The complex central receptor is the G protein-coupled receptor calcitonin receptor-like receptor (CALCRL) which is necessary for CGRP and adrenomedullin (AM receptors). For function CGRP, CALCRL must coincide with RAMP1 where the ligand-binding domain of CGRP is located. It also includes two cytoplasmic proteins that associate with the CALCRL-RAMP1 to form signal transduction. CALCRL contains the Gα subunit, which activates adenylyl cyclase and cAMP-dependent signaling pathways. Receptor-mediated transduction elevates in intracellular cAMP activate protein kinase A, which results in the phosphorylation of multiple targets, including potassium- sensitive ATP channels (KATP channels), extracellular signal-related kinases and transcription factors such as cAMP-responsive element-binding protein (CREB). In smooth muscle of neurovascular region, the elevation of cAMP upon CGRP activation results in vasodilation of the blood vessel. Chronic exposure to CGRP causes degradation of lysosomes.[19]
Research
Increased levels of CGRP have been reported in migraine and temporomandibular joint disorder patients as well as a variety of other diseases such as cardiac failure, hypertension, and sepsis.[20][21][22][23][24][25][26]
There is mounting evidence to suggest that CGRP may be beneficial in preventing the development of hypertension and cardiovascular pathologies associated with hypertension.[2] Prophylactic therapy with calcitonin gene‐related peptides (CGRPs) may have unknown fertility consequences for women of child bearing age. This is of particular concern, as females (16.6%) are more genetically predisposed to migraine than are males (7.5%).[27]
Preclinical evidence suggests that, during a migraine, activated primary sensory neurons (meningeal nociceptors) in the trigeminal ganglion release CGRP from their peripherally projecting nerve endings located within the meninges.[28][26] This CGRP then binds to and activates CGRP receptors located around meningeal vessels, causing vasodilation, mast cell degranulation, and plasma extravasation.[13][28][29][30] Human observations have further implicated the role of CGRP in the pathophysiology of migraine. Activation of primary sensory neurons in the trigeminal vascular system in humans can cause the release of CGRP. During some migraine attacks, increased concentrations of CGRP can be found in both saliva and in plasma drawn from the external jugular vein.[13][28][29][30] Furthermore, intravenous administration of alpha-CGRP is able to induce headache in individuals susceptible to migraine.[31][26]
Medicines
New medicines are now on the market that contain antibodies against either CGRP itself, or its receptor. They are called monoclonal antibodies (MABs) and are large molecules that do not cross the blood-brain-barrier.[32] They typically are not metabolized by the liver and have little direct impact on the metabolism of more conventional small-molecule drugs.[33] They also tend to have relatively long half-lives in the body, but must be given parenterally (preferably by injection) due to very poor absorption from the digestive tract.[34] They have been proved to be effective in people who experience migraine headaches, both with and without aura, and both episodic and chronic cluster headache. These are the first class of preventive medications originally designed and approved for people with migraine.[26] Monoclonal means all the antibodies are made from the same genetic material, although different MABs may derive from different sources, e.g. from hamster ovarian cells, from yeast cells or from humanized cell cultures. The antibodies are also made repeatedly to make them all identical, which results in difficult and relatively expensive production lines. Antibodies are proteins that counter or interfere with very specific parts of another protein or the site where a protein is supposed to bind to the receptor. Most commonly thought of in being used to prevent or fight off infections.[35]
The first approved by the FDA is called erenumab (trade name Aimovig), produced by pharmaceutical company Amgen and Novartis. It interacts with the CGRP receptor. It is injected once monthly with a dose of 70 or 140 mg. Few adverse effects were reported (most related to injection site reactions) and patients had a significant reduction in migraines.[36][37]
The second approved by the FDA is called fremanezumab (trade name Ajovy), produced by the Teva pharmaceutical company. It interacts with the CGRP protein, whose expression is related to migraine attacks. It may be administered monthly or every three months, giving options for users. Trials have shown a reduction of greater than 50% of migraine days for those who responded. There were few significant side effects during trials, most related to injection site reactions.[38][39]
The third approved by the FDA is called galcanezumab (trade name Emgality), produced by the Eli Lilly Company. It interacts with the CGRP protein, whose expression is related to migraine attacks. It is injected once a month, after the first month having a double dose. The main side effects are injection site reactions.[40][41]
Approved by the FDA in February 2020, ubrogepant is an oral medication manufactured by Allergan.
Also FDA approved in February 2020, eptinezumab (Vyepti), is an intravenous migraine prophylactic medication manufactured by Lundbeck.
The phytocannabinoids delta-9 tetrahydrocannabinol (Δ9-THC) and its oxidative byproduct cannabinol (CBN) are found to induce a CB1 and CB2 cannabinoid receptor-independent release of calcitonin gene-related peptide from capsaicin-sensitive perivascular sensory nerves, an action other psychotropic cannabinoids cannot do.[42][43]
References
- ↑ "Calcitonin gene-related peptide enhances osteogenic differentiation and recruitment of bone marrow mesenchymal stem cells in rats". Experimental and Therapeutic Medicine 18 (2): 1039–1046. August 2019. doi:10.3892/etm.2019.7659. PMID 31316600.
- ↑ "Alternative RNA processing in calcitonin gene expression generates mRNAs encoding different polypeptide products". Nature 298 (5871): 240–4. July 1982. doi:10.1038/298240a0. PMID 6283379. Bibcode: 1982Natur.298..240A.
- ↑ "alphaCGRP and betaCGRP transcript amount in mouse tissues of various developmental stages and their tissue expression sites". Brain & Development 31 (9): 682–93. October 2009. doi:10.1016/j.braindev.2008.10.011. PMID 19062206.
- ↑ "The Trigeminovascular Pathway: Role of CGRP and CGRP Receptors in Migraine". Headache 57 Suppl 2 (S2): 47–55. May 2017. doi:10.1111/head.13081. PMID 28485848.
- ↑ "Production of a novel neuropeptide encoded by the calcitonin gene via tissue-specific RNA processing". Nature 304 (5922): 129–35. 1983. doi:10.1038/304129a0. PMID 6346105. Bibcode: 1983Natur.304..129R.
- ↑ "Calcitonin gene-related peptide is a potent vasodilator". Nature 313 (5997): 54–6. 1985. doi:10.1038/313054a0. PMID 3917554. Bibcode: 1985Natur.313...54B.
- ↑ "Calcitonin gene-related peptide: functional role in cerebrovascular regulation". Proceedings of the National Academy of Sciences of the United States of America 83 (15): 5731–5. August 1986. doi:10.1073/pnas.83.15.5731. PMID 3488550. Bibcode: 1986PNAS...83.5731M.
- ↑ "Expression of calcitonin gene-related peptide in anterior and posterior horns of the spinal cord after brachial plexus injury". Journal of Clinical Neuroscience 17 (1): 87–91. January 2010. doi:10.1016/j.jocn.2009.03.042. PMID 19969463.
- ↑ Jump up to: 10.0 10.1 10.2 10.3 10.4 Hormones. Amsterdam: Elsevier. 2014. ISBN 978-0-12-369444-7.
- ↑ Jump up to: 11.0 11.1 "Nociceptive nerves regulate haematopoietic stem cell mobilization". Nature 589 (7843): 591–596. January 2021. doi:10.1038/s41586-020-03057-y. PMID 33361809. Bibcode: 2021Natur.589..591G.
- ↑ "International Union of Pharmacology. XXXII. The mammalian calcitonin gene-related peptides, adrenomedullin, amylin, and calcitonin receptors". Pharmacological Reviews 54 (2): 233–46. June 2002. doi:10.1124/pr.54.2.233. PMID 12037140.
- ↑ Jump up to: 13.0 13.1 13.2 "Calcitonin gene-related peptide and its role in migraine pathophysiology". European Journal of Pharmacology 500 (1–3): 315–30. October 2004. doi:10.1016/j.ejphar.2004.07.035. PMID 15464043.
- ↑ "Understanding the molecular functions of the second extracellular loop (ECL2) of the calcitonin gene-related peptide (CGRP) receptor using a comprehensive mutagenesis approach". Molecular and Cellular Endocrinology 454: 39–49. October 2017. doi:10.1016/j.mce.2017.05.034. PMID 28572046. http://repository.essex.ac.uk/19762/1/Molecular_functions_of_ECL2_of_CGRP.pdf.
- ↑ Jump up to: 15.0 15.1 "Stimulation of the calcitonin gene-related peptide enhancer by mitogen-activated protein kinases and repression by an antimigraine drug in trigeminal ganglia neurons". The Journal of Neuroscience 23 (3): 807–15. February 2003. doi:10.1523/JNEUROSCI.23-03-00807.2003. PMID 12574409.
- ↑ "Tumor necrosis factor-alpha induces mechanical allodynia after spinal nerve ligation by activation of p38 MAPK in primary sensory neurons". The Journal of Neuroscience 23 (7): 2517–21. April 2003. doi:10.1523/JNEUROSCI.23-07-02517.2003. PMID 12684435.
- ↑ "Calcitonin gene-related peptide stimulation of nitric oxide synthesis and release from trigeminal ganglion glial cells". Brain Research 1196: 22–32. February 2008. doi:10.1016/j.brainres.2007.12.028. PMID 18221935.
- ↑ "Blocking CGRP in migraine patients - a review of pros and cons". The Journal of Headache and Pain 18 (1): 96. September 2017. doi:10.1186/s10194-017-0807-1. PMID 28948500.
- ↑ "CGRP as the target of new migraine therapies - successful translation from bench to clinic". Nature Reviews. Neurology 14 (6): 338–350. June 2018. doi:10.1038/s41582-018-0003-1. PMID 29691490.
- ↑ "Neurogenic model of migraine". Cephalalgia 15 (4): 277–80. 1995. doi:10.1046/j.1468-2982.1995.1504277.x. PMID 7585923.
- ↑ "Calcitonin gene-related peptide in the regulation of cardiac function". Annals of the New York Academy of Sciences 657 (1): 194–203. June 1992. doi:10.1111/j.1749-6632.1992.tb22768.x. PMID 1637085. Bibcode: 1992NYASA.657..194G.
- ↑ "Calcitonin gene-related peptide levels are elevated in patients with sepsis". Surgery 108 (6): 1097–101. December 1990. PMID 2247835.
- ↑ "Neuropeptides in migraine and cluster headache". Cephalalgia 14 (5): 320–7. October 1994. doi:10.1046/j.1468-2982.1994.1405320.x. PMID 7828188.
- ↑ "On serotonin and migraine: a clinical and pharmacological review". Cephalalgia 13 (3): 151–65. June 1993. doi:10.1046/j.1468-2982.1993.1303151.x. PMID 8395342.
- ↑ "Human in vivo evidence for trigeminovascular activation in cluster headache. Neuropeptide changes and effects of acute attacks therapies". Brain 117 ( Pt 3) (3): 427–34. June 1994. doi:10.1093/brain/117.3.427. PMID 7518321.
- ↑ Jump up to: 26.0 26.1 26.2 26.3 "What to Know About the New CGRP Migraine Treatment Options". https://americanmigrainefoundation.org/resource-library/what-to-know-about-the-new-anti-cgrp-migraine-treatment-options/.
- ↑ "Spotlight on Anti-CGRP Monoclonal Antibodies in Migraine: The Clinical Evidence to Date". Clinical Pharmacology in Drug Development 6 (6): 534–547. November 2017. doi:10.1002/cpdd.345. PMID 28409893.
- ↑ Jump up to: 28.0 28.1 28.2 "Calcitonin gene-related peptide (CGRP) and migraine". Headache 46 (Suppl 1): S3-8. June 2006. doi:10.1111/j.1526-4610.2006.00483.x. PMID 16927957.
- ↑ Jump up to: 29.0 29.1 "Vasoactive peptide release in the extracerebral circulation of humans during migraine headache". Annals of Neurology 28 (2): 183–7. August 1990. doi:10.1002/ana.410280213. PMID 1699472.
- ↑ Jump up to: 30.0 30.1 "Neuronal signal substances as biomarkers of migraine". Headache 46 (7): 1088–94. 2006. doi:10.1111/j.1526-4610.2006.00502.x. PMID 16866713.
- ↑ "CGRP may play a causative role in migraine". Cephalalgia 22 (1): 54–61. February 2002. doi:10.1046/j.1468-2982.2002.00310.x. PMID 11993614.
- ↑ "Delivery of Biologics Across the Blood-Brain Barrier with Molecular Trojan Horse Technology". BioDrugs 31 (6): 503–519. December 2017. doi:10.1007/s40259-017-0248-z. PMID 29067674.
- ↑ "Pharmacokinetics interactions of monoclonal antibodies". Pharmacological Research 111: 592–599. September 2016. doi:10.1016/j.phrs.2016.07.015. PMID 27438459.
- ↑ "Monoclonal antibody pharmacokinetics and pharmacodynamics". Clinical Pharmacology and Therapeutics 84 (5): 548–58. November 2008. doi:10.1038/clpt.2008.170. PMID 18784655.
- ↑ "CGRP: What You Need To Know". 2018-01-16. https://headaches.org/2018/01/16/cgrp-need-know/.
- ↑ "FDA Approves Erenumab, First CGRP Inhibitor for Prevention of Migraine". 18 May 2018. https://www.ajmc.com/newsroom/fda-approves-erenumab-first-cgrp-inhibitor-for-prevention-of-migraine.
- ↑ "Erenumab for Preventive Treatment of Migraine: A Systematic Review and Meta-Analysis of Efficacy and Safety". Drugs 79 (4): 417–431. March 2019. doi:10.1007/s40265-019-01069-1. PMID 30793254.
- ↑ "FDA Approves Second Anti-CGRP Treatment for Migraines". https://americanmigrainefoundation.org/resource-library/fda-approves-second-anti-cgrp-treatment-for-migraine/.
- ↑ "From LBR-101 to Fremanezumab for Migraine". CNS Drugs 32 (11): 1025–1037. November 2018. doi:10.1007/s40263-018-0579-4. PMID 30311143.
- ↑ "Lilly's Emgality™ (galcanezumab-gnlm) Receives U.S. FDA Approval for the Preventive Treatment of Migraine in Adults". https://investor.lilly.com/news-releases/news-release-details/lillys-emgalitytm-galcanezumab-gnlm-receives-us-fda-approval.
- ↑ "Galcanezumab: First Global Approval". Drugs 78 (16): 1769–1775. November 2018. doi:10.1007/s40265-018-1002-7. PMID 30378008.
- ↑ "Degradants Formed During Phytocannabinoid Processing" (in en). https://www.caymanchem.com/news/degradants-formed-during-phytocannabinoid-processing.
- ↑ "Δ9-Tetrahydrocannabinol and Cannabinol Activate Capsaicin-Sensitive Sensory Nerves via a CB1 and CB2 Cannabinoid Receptor-Independent Mechanism". The Journal of Neuroscience 22 (11): 4720–7. June 2002. doi:10.1523/JNEUROSCI.22-11-04720.2002. PMID 12040079.
External links
- Calcitonin+Gene-Related+Peptide at the US National Library of Medicine Medical Subject Headings (MeSH)
 |