Chemistry:Ibuprofen
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˈaɪbjuːproʊfɛn/, /aɪbjuːˈproʊfən/, EYE-bew-PROH-fən |
| Trade names | Advil, Motrin, Nurofen, others |
| Other names | isobutylphenylpropionic acid |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682159 |
| License data | |
| Pregnancy category |
|
| Routes of administration | Oral (by mouth), rectal, topical, intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 80–100% (orally),[2] 87% (rectal) |
| Protein binding | 98%[3] |
| Metabolism | Liver (CYP2C9)[3] |
| Metabolites | ibuprofen glucuronide, 2-hydroxyibuprofen, 3-hydroxyibuprofen, carboxy-ibuprofen, 1-hydroxyibuprofen |
| Onset of action | 30 min[4] |
| Elimination half-life | 2–4 h[5] |
| Excretion | Urine (95%)[3][6] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| Chemical and physical data | |
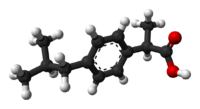
| Formula | C13H18O2 |
| Molar mass | 206.285 g·mol−1 |
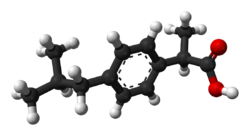
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| Density | 1.03 g/cm3 |
| Melting point | 75 to 78 °C (167 to 172 °F) |
| Boiling point | 157 °C (315 °F) at 4 mmHg |
| Solubility in water | 0.021 mg/mL (20 °C) |
| |
| |
| (verify) | |
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that is used to relieve pain, fever, and inflammation.[7] This includes painful menstrual periods, migraines, and rheumatoid arthritis.[7] It may also be used to close a patent ductus arteriosus in a premature baby.[7] It can be used orally (by mouth) or intravenously.[7] It typically begins working within an hour.[7]
Common side effects include heartburn and a rash.[7] Compared to other NSAIDs, it may have other side effects such as gastrointestinal bleeding.[8] It increases the risk of heart failure, kidney failure, and liver failure.[7] At low doses, it does not appear to increase the risk of heart attack; however, at higher doses it may.[8] Ibuprofen can also worsen asthma.[8] While its safety in early pregnancy is unclear,[7] it appears to be harmful in later pregnancy, so it is not recommended during that period. [9] Like other NSAIDs, it works by inhibiting the production of prostaglandins by decreasing the activity of the enzyme cyclooxygenase (COX).[7] Ibuprofen is a weaker anti-inflammatory agent than other NSAIDs.[8]
Ibuprofen was discovered in 1961 by Stewart Adams and John Nicholson[10] while working at Boots UK Limited and initially marketed as Brufen.[11] It is available under a number of brand names, including Nurofen, Advil, and Motrin.[7][12] Ibuprofen was first marketed in 1969 in the United Kingdom and in 1974 in the United States.[7][11] It is on the World Health Organization's List of Essential Medicines.[13] It is available as a generic medication.[7] In 2021, it was the 36th-most commonly prescribed medication in the United States, with more than 17 million prescriptions.[14][15]
Medical uses
Ibuprofen is used primarily to treat fever (including postvaccination fever), mild to moderate pain (including pain relief after surgery), painful menstruation, osteoarthritis, dental pain, headaches, and pain from kidney stones. About 60% of people respond to any NSAID; those who do not respond well to a particular one may respond to another.[16] A Cochrane medical review of 51 trials of NSAIDS for the treatment of lower back pain found that "NSAIDs are effective for short-term symptomatic relief in patients with acute low back pain".[17]
It is used for inflammatory diseases such as juvenile idiopathic arthritis and rheumatoid arthritis.[18][19] It is also used for pericarditis and patent ductus arteriosus.[20][21]
Ibuprofen lysine
In some countries, ibuprofen lysine (the lysine salt of ibuprofen, sometimes called "ibuprofen lysinate") is licensed for treatment of the same conditions as ibuprofen; the lysine salt is used because it is more water-soluble.[22]
Ibuprofen lysine is sold for rapid pain relief;[23] given in form of a lysine salt, absorption is much quicker (35 minutes compared to 90–120 minutes). However, a clinical trial with 351 participants in 2020, funded by Sanofi, found no significant difference between ibuprofen and ibuprofen lysine concerning the eventual onset of action or analgesic efficacy.[24][unreliable medical source]
In 2006, ibuprofen lysine was approved in the U.S. by the Food and Drug Administration (FDA) for closure of patent ductus arteriosus in premature infants weighing between 500 and 1,500 g (1 and 3 lb), who are no more than 32 weeks gestational age when usual medical management (such as fluid restriction, diuretics, and respiratory support) is not effective.[25]
Adverse effects
Adverse effects include nausea, indigestion, diarrhea, constipation, gastrointestinal ulceration, headache, dizziness, rash, salt and fluid retention, and high blood pressure.[19][26]
Infrequent adverse effects include esophageal ulceration, heart failure, high blood levels of potassium, kidney impairment, confusion, and bronchospasm.[19] Ibuprofen can exacerbate asthma, sometimes fatally.[27]
Allergic reactions, including anaphylaxis and anaphylactic shock, may occur.[28] Ibuprofen may be quantified in blood, plasma, or serum to demonstrate the presence of the drug in a person having experienced an anaphylactic reaction, confirm a diagnosis of poisoning in people who are hospitalized, or assist in a medicolegal death investigation. A monograph relating ibuprofen plasma concentration, time since ingestion, and risk of developing renal toxicity in people who have overdosed has been published.[29]
In October 2020, the US FDA required the drug label to be updated for all NSAID medications to describe the risk of kidney problems in unborn babies that result in low amniotic fluid.[30][31]
Cardiovascular risk
Along with several other NSAIDs, chronic ibuprofen use has been found correlated with risk of progression to hypertension in women, though less than for paracetamol (acetaminophen),[32] and myocardial infarction (heart attack),[33] particularly among those chronically using higher doses. On 9 July 2015, the US FDA toughened warnings of increased heart attack and stroke risk associated with ibuprofen and related NSAIDs; the NSAID aspirin is not included in this warning.[34] The European Medicines Agency (EMA) issued similar warnings in 2015.[35][36]
Skin
Along with other NSAIDs, ibuprofen has been associated with the onset of bullous pemphigoid or pemphigoid-like blistering.[37] As with other NSAIDs, ibuprofen has been reported to be a photosensitising agent,[38] but it is considered a weak photosensitising agent compared to other members of the 2-arylpropionic acid class. Like other NSAIDs, ibuprofen is an extremely rare cause of the autoimmune disease Stevens–Johnson syndrome (SJS).[39][40] Ibuprofen is also an extremely rare cause of toxic epidermal necrolysis.[41]
Interactions
Alcohol
Drinking alcohol when taking ibuprofen may increase the risk of stomach bleeding.[42]
Aspirin
According to the FDA, "ibuprofen can interfere with the antiplatelet effect of low-dose aspirin, potentially rendering aspirin less effective when used for cardioprotection and stroke prevention". Allowing sufficient time between doses of ibuprofen and immediate-release (IR) aspirin can avoid this problem. The recommended elapsed time between a dose of ibuprofen and a dose of aspirin depends on which is taken first. It would be 30 minutes or more for ibuprofen taken after IR aspirin, and 8 hours or more for ibuprofen taken before IR aspirin. However, this timing cannot be recommended for enteric-coated aspirin. If ibuprofen is taken only occasionally without the recommended timing, though, the reduction of the cardioprotection and stroke prevention of a daily aspirin regimen is minimal.[43]
Paracetamol
Ibuprofen combined with paracetamol is considered generally safe in children for short-term usage.[44]
Overdose
Ibuprofen overdose has become common since it was licensed for OTC use. Many overdose experiences are reported in the medical literature, although the frequency of life-threatening complications from ibuprofen overdose is low.[45] Human responses in cases of overdose range from an absence of symptoms to a fatal outcome despite intensive-care treatment. Most symptoms are an excess of the pharmacological action of ibuprofen, and include abdominal pain, nausea, vomiting, drowsiness, dizziness, headache, ear ringing, and nystagmus. Rarely, more severe symptoms, such as gastrointestinal bleeding, seizures, metabolic acidosis, hyperkalemia, low blood pressure, slow heart rate, fast heart rate, atrial fibrillation, coma, liver dysfunction, acute kidney failure, cyanosis, respiratory depression, and cardiac arrest have been reported.[46] The severity of symptoms varies with the ingested dose and the time elapsed; however, individual sensitivity also plays an important role. Generally, the symptoms observed with an overdose of ibuprofen are similar to the symptoms caused by overdoses of other NSAIDs.
Correlation between severity of symptoms and measured ibuprofen plasma levels is weak. Toxic effects are unlikely at doses below 100 mg/kg, but can be severe above 400 mg/kg (around 150 tablets of 200 mg units for an average man);[47] however, large doses do not indicate the clinical course is likely to be lethal.[48] A precise lethal dose is difficult to determine, as it may vary with age, weight, and concomitant conditions of the individual person.
Treatment to address an ibuprofen overdose is based on how the symptoms present. In cases presenting early, decontamination of the stomach is recommended. This is achieved using activated charcoal; charcoal absorbs the drug before it can enter the bloodstream. Gastric lavage is now rarely used, but can be considered if the amount ingested is potentially life-threatening, and it can be performed within 60 minutes of ingestion. Purposeful vomiting is not recommended.[49] Most ibuprofen ingestions produce only mild effects, and the management of overdose is straightforward. Standard measures to maintain normal urine output should be instituted and kidney function monitored.[47] Since ibuprofen has acidic properties and is also excreted in the urine, forced alkaline diuresis is theoretically beneficial. However, because ibuprofen is highly protein-bound in the blood, the kidneys' excretion of unchanged drug is minimal. Forced alkaline diuresis is, therefore, of limited benefit.[50]
Miscarriage
A Canadian study of pregnant women suggests that those taking any type or amount of NSAIDs (including ibuprofen, diclofenac, and naproxen) were 2.4 times more likely to miscarry than those not taking the medications.[51] However, an Israeli study found no increased risk of miscarriage in the group of mothers using NSAIDs.[52]
Pharmacology
NSAIDs such as ibuprofen work by inhibiting the cyclooxygenase (COX) enzymes, which convert arachidonic acid to prostaglandin H2 (PGH2). PGH2, in turn, is converted by other enzymes to several other prostaglandins (which are mediators of pain, inflammation, and fever) and to thromboxane A2 (which stimulates platelet aggregation, leading to the formation of blood clots).
Like aspirin and indomethacin, ibuprofen is a nonselective COX inhibitor, in that it inhibits two isoforms of cyclooxygenase, COX-1 and COX-2. The analgesic, antipyretic, and anti-inflammatory activity of NSAIDs appears to operate mainly through inhibition of COX-2, which decreases the synthesis of prostaglandins involved in mediating inflammation, pain, fever, and swelling. Antipyretic effects may be due to action on the hypothalamus, resulting in an increased peripheral blood flow, vasodilation, and subsequent heat dissipation. Inhibition of COX-1 instead would be responsible for unwanted effects on the gastrointestinal tract.[53] However, the role of the individual COX isoforms in the analgesic, anti-inflammatory, and gastric damage effects of NSAIDs is uncertain, and different compounds cause different degrees of analgesia and gastric damage.[54]
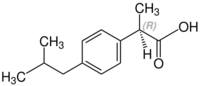
Ibuprofen is administered as a racemic mixture. The R-enantiomer undergoes extensive interconversion to the S-enantiomer in vivo. The S-enantiomer is believed to be the more pharmacologically active enantiomer.[55] The R-enantiomer is converted through a series of three main enzymes. These enzymes include acyl-CoA-synthetase, which converts the R-enantiomer to (−)-R-ibuprofen I-CoA; 2-arylpropionyl-CoA epimerase, which converts (−)-R-ibuprofen I-CoA to (+)-S-ibuprofen I-CoA; and hydrolase, which converts (+)-S-ibuprofen I-CoA to the S-enantiomer.[41] In addition to the conversion of ibuprofen to the S-enantiomer, the body can metabolize ibuprofen to several other compounds, including numerous hydroxyl, carboxyl and glucuronyl metabolites. Virtually all of these have no pharmacological effects.[41]
Unlike most other NSAIDs, ibuprofen also acts as an inhibitor of Rho kinase and may be useful in recovery from spinal-cord injury.[56][57] Another unusual activity is inhibition of the sweet taste receptor.[58]
Pharmacokinetics
After oral administration, peak serum concentration is reached after 1–2 hours, and up to 99% of the drug is bound to plasma proteins.[59] The majority of ibuprofen is metabolized and eliminated within 24 hours in the urine; however, 1% of the unchanged drug is removed through biliary excretion.[55]
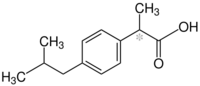
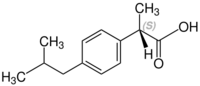
Chemistry
Ibuprofen is practically insoluble in water, but very soluble in most organic solvents like ethanol (66.18 g/100 mL at 40 °C for 90% EtOH), methanol, acetone and dichloromethane.[60]
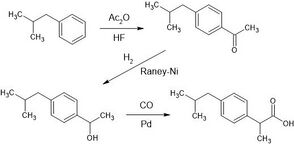
The original synthesis of ibuprofen by the Boots Group started with the compound isobutylbenzene. The synthesis took six steps. A modern, greener technique with fewer waste byproducts for the synthesis involves only three steps was developed in the 1980s by the Celanese Chemical Company.[61][62] The synthesis is initiated with the acylation of isobutylbenzene using the recyclable Lewis acid catalyst hydrogen fluoride.[63][64] The following catalytic hydrogenation of isobutylacetophenone is performed with either Raney nickel or palladium on carbon to lead into the key-step, the carbonylation of 1-(4-isobutylphenyl)ethanol. This is achieved by a PdCl2(PPh3)2 catalyst, at around 50 bar of CO pressure, in the presence of HCl (10%).[65] The reaction presumably proceeds through the intermediacy of the styrene derivative (acidic elimination of the alcohol) and (1-chloroethyl)benzene derivative (Markovnikow addition of HCl to the double bond).[66]
Stereochemistry
Ibuprofen, like other 2-arylpropionate derivatives such as ketoprofen, flurbiprofen and naproxen, contains a stereocenter in the α-position of the propionate moiety.
 |
|
 |
|
| (R)-ibuprofen | (S)-ibuprofen |
The product sold in pharmacies is a racemic mixture of the S and R-isomers. The S (dextrorotatory) isomer is the more biologically active; this isomer has been isolated and used medically (see dexibuprofen for details).[60]
The isomerase enzyme, alpha-methylacyl-CoA racemase, converts (R)-ibuprofen into the (S)-enantiomer.[67][68][69]
(S)-ibuprofen, the eutomer, harbors the desired therapeutic activity. Interestingly, the inactive (R)-enantiomer, the distomer, undergoes a unidirectional chiral inversion to offer the active (S)-enantiomer. That is, when the ibuprofen is administered as a racemate the distomer is converted in vivo into the eutomer while the latter is unaffected.[70][71][72]
History
Ibuprofen was derived from propionic acid by the research arm of Boots Group during the 1960s.[73] The name is derived from the 3 functional groups: isobutyl (ibu) propionic acid (pro) phenyl (fen). Its discovery was the result of research during the 1950s and 1960s to find a safer alternative to aspirin.[11][74] The molecule was discovered and synthesized by a team led by Stewart Adams, with a patent application filed in 1961.[11] Adams initially tested the drug as treatment for his hangover.[75] In 1985, Boots' worldwide patent for ibuprofen expired and generic products were launched.[76]
The drug was launched as a treatment for rheumatoid arthritis in the United Kingdom in 1969, and in the United States in 1974. Later, in 1983 and 1984, it became the first NSAID (other than aspirin) to be available over the counter (OTC) in these two countries.[11][74] Boots was awarded the Queen's Award for Technical Achievement in 1985 for the development of the drug.[77]
In November 2013, work on ibuprofen was recognized by the erection of a Royal Society of Chemistry blue plaque at Boots' Beeston Factory site in Nottingham,[78] which reads:
In recognition of the work during the 1980s by The Boots Company PLC on the development of ibuprofen which resulted in its move from prescription only status to over the counter sale, therefore expanding its use to millions of people worldwide
and another at BioCity Nottingham, the site of the original laboratory,[78] which reads:
In recognition of the pioneering research work, here on Pennyfoot Street, by Dr Stewart Adams and Dr John Nicholson in the Research Department of Boots which led to the discovery of ibuprofen used by millions worldwide for the relief of pain.
Availability and administration
Ibuprofen was made available by prescription in the United Kingdom in 1969 and in the United States in 1974.[79]
Ibuprofen is the International nonproprietary name (INN), British Approved Name (BAN), Australian Approved Name (AAN) and United States Adopted Name (USAN). In the United States, it has been sold under the brand-names Motrin and Advil since 1974[80] and 1984,[81] respectively. Ibuprofen is commonly available in the United States up to the FDA's 1984 dose limit OTC, rarely used higher by prescription.[82][failed verification]
In 2009, the first injectable formulation of ibuprofen was approved in the United States, under the brand name Caldolor.[83][84]
Ibuprofen can be taken orally (by mouth) (as a tablet, a capsule, or a suspension) and intravenously.[7]
Research
Ibuprofen is sometimes used for the treatment of acne because of its anti-inflammatory properties, and has been sold in Japan in topical form for adult acne.[85][86] As with other NSAIDs, ibuprofen may be useful in the treatment of severe orthostatic hypotension (low blood pressure when standing up).[87] NSAIDs are of unclear utility in the prevention and treatment of Alzheimer's disease.[88][89]
Ibuprofen has been associated with a lower risk of Parkinson's disease and may delay or prevent it. Aspirin, other NSAIDs, and paracetamol (acetaminophen) had no effect on the risk for Parkinson's.[90] In March 2011, researchers at Harvard Medical School announced in Neurology that ibuprofen had a neuroprotective effect against the risk of developing Parkinson's disease.[91][92][93] People regularly consuming ibuprofen were reported to have a 38% lower risk of developing Parkinson's disease, but no such effect was found for other pain relievers, such as aspirin and paracetamol. Use of ibuprofen to lower the risk of Parkinson's disease in the general population would not be problem-free, given the possibility of adverse effects on the urinary and digestive systems.[94]
Some dietary supplements might be dangerous to take along with ibuprofen and other NSAIDs, but (As of 2016) more research needs to be conducted to be certain. These supplements include those that can prevent platelet aggregation, including ginkgo, garlic, ginger, bilberry, dong quai, feverfew, ginseng, turmeric, meadowsweet (Filipendula ulmaria), and willow (Salix spp.); those that contain coumarin, including chamomile, horse chestnut, fenugreek and red clover; and those that increase the risk of bleeding, like tamarind.[95]
References
- ↑ Use During Pregnancy and Breastfeeding
- ↑ "Breastfeeding and migraine drugs". European Journal of Clinical Pharmacology 70 (11): 1313–1324. November 2014. doi:10.1007/s00228-014-1748-0. PMID 25217187.
- ↑ 3.0 3.1 3.2 "Clinical pharmacokinetics of ibuprofen. The first 30 years". Clinical Pharmacokinetics 34 (2): 101–154. February 1998. doi:10.2165/00003088-199834020-00002. PMID 9515184.
- ↑ "ibuprofen". http://web.squ.edu.om/med-lib/med_cd/e_cds/Nursing%20Drug%20Guide/mg/ibuprofen.htm.
- ↑ "The Cardiovascular Pharmacology of Nonsteroidal Anti-Inflammatory Drugs". Trends in Pharmacological Sciences 38 (8): 733–748. August 2017. doi:10.1016/j.tips.2017.05.008. PMID 28651847.
- ↑ "Brufen Tablets And Syrup" (PDF). Therapeutic Goods Administration. 31 July 2012. https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2009-PI-00035-3.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 "Ibuprofen". The American Society of Health-System Pharmacists. https://www.drugs.com/monograph/ibuprofen.html.
- ↑ 8.0 8.1 8.2 8.3 British National Formulary, March 2014–September 2014 (2014 ed.). London: British Medical Association. 2014. pp. 686–688. ISBN 978-0857110862.
- ↑ "Ibuprofen Pregnancy and Breastfeeding Warnings". https://www.drugs.com/pregnancy/ibuprofen.html.
- ↑ "The Inventor of Ibuprofen Tested the Drug on His Own Hangover" (in en). https://www.smithsonianmag.com/innovation/inventor-ibuprofen-tested-drug-his-own-hangover-180975088/. "Stewart Adams and his associate John Nicholson invented a pharmaceutical drug known as 2-(4-isobutylphenyl) propionic acid."
- ↑ 11.0 11.1 11.2 11.3 11.4 "50th anniversary of the discovery of ibuprofen: an interview with Dr Stewart Adams". Platelets 23 (6): 415–422. 2012. doi:10.3109/09537104.2011.632032. PMID 22098129.
- ↑ "Chemistry in your cupboard: Nurofen". http://www.rsc.org/learn-chemistry/resources/chemistry-in-your-cupboard/nurofen/4.
- ↑ World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. 2021. WHO/MHP/HPS/EML/2021.02.
- ↑ "The Top 300 of 2021". https://clincalc.com/DrugStats/Top300Drugs.aspx.
- ↑ "Ibuprofen. Drug Usage Statistics". https://clincalc.com/DrugStats/Drugs/Ibuprofen.
- ↑ "10.1.1 Non-steroidal anti-inflammatory drugs". https://www.evidence.nhs.uk/formulary/bnf/current/10-musculoskeletal-and-joint-diseases/101-drugs-used-in-rheumatic-diseases-and-gout/1011-non-steroidal-anti-inflammatory-drugs.
- ↑ "Do NSAIDs help in acute or chronic low back pain?". American Family Physician 65 (7): 1319–1321. April 2002. PMID 11996413. https://www.aafp.org/pubs/afp/issues/2002/0401/p1319.html.
- ↑ Joint Formulary Committee (2013). British National Formulary (BNF) (65 ed.). London, UK: Pharmaceutical Press. pp. 665, 671. ISBN 978-0-85711-084-8. https://archive.org/details/bnf65britishnati0000unse/page/665.
- ↑ 19.0 19.1 19.2 Rossi, S, ed (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- ↑ "Colchicine for pericarditis". The Cochrane Database of Systematic Reviews 2014 (8): CD010652. August 2014. doi:10.1002/14651858.CD010652.pub2. PMID 25164988. PMC 10645160. http://openaccess.city.ac.uk/4043/5/Colchicine%20for%20pericarditis.pdf.
- ↑ "Pharmacotherapy for Patent Ductus Arteriosus: Current Options and Outstanding Questions". Current Pediatric Reviews 12 (2): 110–119. 2016. doi:10.2174/157339631202160506002028. PMID 27197952.
- ↑ "Review of the analgesic efficacy of ibuprofen". International Journal of Clinical Practice. Supplement (135): 13–17. April 2003. PMID 12723741.
- ↑ "Comparison of two different preparations of ibuprofen with regard to the time course of their analgesic effect. A randomised, placebo-controlled, double-blind cross-over study using laser somatosensory evoked potentials obtained from UW-irritated skin in healthy volunteers". Arzneimittel-Forschung 54 (8): 444–451. 2004. doi:10.1055/s-0031-1296997. PMID 15460211.
- ↑ "A Randomized, Double-Blind, Placebo-Controlled Trial of Ibuprofen Lysinate in Comparison to Ibuprofen Acid for Acute Postoperative Dental Pain". Pain and Therapy 9 (1): 249–259. June 2020. doi:10.1007/s40122-019-00148-1. PMID 31912434.
- ↑ "Ibuprofen and acute kidney injury in the newborn". The Turkish Journal of Pediatrics 52 (3): 231–238. 2010. PMID 20718179.
- ↑ "Individual NSAIDs and upper gastrointestinal complications: a systematic review and meta-analysis of observational studies (the SOS project)". Drug Safety 35 (12): 1127–46. December 2012. doi:10.1007/BF03261999. PMID 23137151.
- ↑ "Asthma death due to ibuprofen". Lancet 1 (8541): 1082. May 1987. doi:10.1016/S0140-6736(87)90499-5. PMID 2883408.
- ↑ "Ibuprofen-induced Anaphylactic Shock in Adult Saudi Patient". Cureus 11 (12): e6425. December 2019. doi:10.7759/cureus.6425. PMID 31993263.
- ↑ Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, USA: Biomedical Publications. 2008. pp. 758–761.
- ↑ "FDA Warns that Using a Type of Pain and Fever Medication in Second Half of Pregnancy Could Lead to Complications". U.S. Food and Drug Administration (FDA) (Press release). 15 October 2020. Retrieved 15 October 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "NSAIDs may cause rare kidney problems in unborn babies". 21 July 2017. https://www.fda.gov/drugs/drug-safety-and-availability/fda-recommends-avoiding-use-nsaids-pregnancy-20-weeks-or-later-because-they-can-result-low-amniotic.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Non-narcotic analgesic dose and risk of incident hypertension in US women". Hypertension 46 (3): 500–7. September 2005. doi:10.1161/01.HYP.0000177437.07240.70. PMID 16103274.
- ↑ "Risk of myocardial infarction in patients taking cyclo-oxygenase-2 inhibitors or conventional non-steroidal anti-inflammatory drugs: population based nested case-control analysis". BMJ 330 (7504): 1366. June 2005. doi:10.1136/bmj.330.7504.1366. PMID 15947398.
- ↑ "FDA Drug Safety Communication: FDA strengthens warning that non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) can cause heart attacks or strokes". U.S. Food and Drug Administration (FDA). 9 July 2015. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-strengthens-warning-non-aspirin-nonsteroidal-anti-inflammatory.
- ↑ "Ibuprofen- and dexibuprofen-containing medicines". 22 May 2015. https://www.ema.europa.eu/en/medicines/human/referrals/ibuprofen-dexibuprofen-containing-medicines.
- ↑ "High-dose ibuprofen (≥2400mg/day): small increase in cardiovascular risk". 26 June 2015. https://www.gov.uk/drug-safety-update/high-dose-ibuprofen-2400mg-day-small-increase-in-cardiovascular-risk.
- ↑ Hall, R; Vinson, RP; Nunley, JR et al., eds (12 June 2014). "Bullous Pemphigoid Clinical Presentation". Medscape Reference. United States: WebMD. http://emedicine.medscape.com/article/1062391-clinical#showall.
- ↑ "Photosensitization caused by ibuprofen". Journal of the American Academy of Dermatology 26 (1): 114–6. January 1992. doi:10.1016/0190-9622(92)70018-b. PMID 1531054.
- ↑ "Clinical study of cutaneous drug eruptions in 200 patients". Indian Journal of Dermatology, Venereology and Leprology 74 (1): 80. 2008. doi:10.4103/0378-6323.38431. PMID 18193504.
- ↑ "Severe adverse skin reactions to nonsteroidal antiinflammatory drugs: A review of the literature". American Journal of Health-System Pharmacy 67 (3): 206–13. February 2010. doi:10.2146/ajhp080603. PMID 20101062.
- ↑ 41.0 41.1 41.2 Ibuprofen: Pharmacology, Therapeutics and Side Effects. London: Springer. 2012.
- ↑ "Ibuprofen". Drugs.com. https://www.drugs.com/ibuprofen.html.
- ↑ "Information for Healthcare Professionals: Concomitant Use of Ibuprofen and Aspirin". U.S. Food and Drug Administration (FDA). September 2006. https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm125222.htm.
- ↑ "A clinical and safety review of paracetamol and ibuprofen in children". Inflammopharmacology 25 (1): 1–9. February 2017. doi:10.1007/s10787-016-0302-3. PMID 28063133.
- ↑ "A prospective, population-based study of acute ibuprofen overdose: complications are rare and routine serum levels not warranted". Annals of Emergency Medicine 19 (6): 657–662. June 1990. doi:10.1016/S0196-0644(05)82471-0. PMID 2188537.
- ↑ "Acute poisoning due to non-steroidal anti-inflammatory drugs. Clinical features and management". Medical Toxicology 1 (1): 12–31. January 1986. doi:10.1007/BF03259825. PMID 3537613.
- ↑ 47.0 47.1 "Non-opioid analgesic poisoning". Clinical Medicine 3 (2): 119–123. March–April 2003. doi:10.7861/clinmedicine.3-2-119. PMID 12737366.
- ↑ "Massive ibuprofen ingestion with survival". Journal of Toxicology. Clinical Toxicology 38 (1): 55–57. 2000. doi:10.1081/clt-100100917. PMID 10696926.
- ↑ American Academy Of Clinical Toxico (2004). "Position paper: Ipecac syrup". Journal of Toxicology. Clinical Toxicology 42 (2): 133–143. doi:10.1081/CLT-120037421. PMID 15214617.
- ↑ "Ibuprofen overdose: 126 cases". Annals of Emergency Medicine 15 (11): 1308–1313. November 1986. doi:10.1016/S0196-0644(86)80617-5. PMID 3777588.
- ↑ "Use of non-aspirin NSAIDs during pregnancy may increase the risk of spontaneous abortion". Evidence-Based Nursing 15 (3): 76–77. July 2012. doi:10.1136/ebnurs-2011-100439. PMID 22411163.
- ↑ "Fetal exposure to nonsteroidal anti-inflammatory drugs and spontaneous abortions". CMAJ 186 (5): E177–E182. March 2014. doi:10.1503/cmaj.130605. PMID 24491470.
- ↑ "Evolution of nonsteroidal anti-inflammatory drugs (NSAIDs): cyclooxygenase (COX) inhibition and beyond". Journal of Pharmacy & Pharmaceutical Sciences 11 (2): 81s–110s. September 2008. doi:10.18433/J3T886. PMID 19203472.
- ↑ "Cyclooxygenase-1-selective inhibitors are attractive candidates for analgesics that do not cause gastric damage. design and in vitro/in vivo evaluation of a benzamide-type cyclooxygenase-1 selective inhibitor". Journal of Medicinal Chemistry 51 (8): 2400–2411. April 2008. doi:10.1021/jm701191z. PMID 18363350.
- ↑ 55.0 55.1 "Ibuprofen". DrugBank. https://www.drugbank.ca/drugs/DB01050.
- ↑ "Small-molecule-induced Rho-inhibition: NSAIDs after spinal cord injury". Cell and Tissue Research 349 (1): 119–132. July 2012. doi:10.1007/s00441-012-1334-7. PMID 22350947.
- ↑ "Exploring the potential of RhoA inhibitors to improve exercise-recoverable spinal cord injury: A systematic review and meta-analysis". Journal of Chemical Neuroanatomy 111: 101879. November 2020. doi:10.1016/j.jchemneu.2020.101879. PMID 33197553.
- ↑ Nakagita, Tomoya; Taketani, Chiaki; Narukawa, Masataka; Hirokawa, Takatsugu; Kobayashi, Takuya; Misaka, Takumi (2020-11-07). "Ibuprofen, a Nonsteroidal Anti-Inflammatory Drug, is a Potent Inhibitor of the Human Sweet Taste Receptor" (in en). Chemical Senses 45 (8): 667–673. doi:10.1093/chemse/bjaa057. ISSN 0379-864X. PMID 32832995. https://academic.oup.com/chemse/article/45/8/667/5896498.
- ↑ "An overview of clinical pharmacology of Ibuprofen". Oman Medical Journal 25 (3): 155–161. July 2010. doi:10.5001/omj.2010.49. PMID 22043330.
- ↑ 60.0 60.1 Brayfield, A, ed (14 January 2014). "Ibuprofen". Martindale: The Complete Drug Reference. London, UK: Pharmaceutical Press. http://www.medicinescomplete.com/mc/martindale/current/ms-2657-h.htm.
- ↑ "The Synthesis of Ibuprofen". Royal Society of Chemistry. http://www.rsc.org/learn-chemistry/resource/download/res00000012/cmp00000014/pdf.
- ↑ "The Ibuprofen Revolution". Science. https://www.science.org/content/blog-post/ibuprofen-revolution.
- ↑ "Early Industrial Roots of Green Chemistry and the history of the BHC Ibuprofen process invention and its Quality connection" (in en). Foundations of Chemistry 20 (2): 121–165. 1 July 2018. doi:10.1007/s10698-017-9300-9. ISSN 1572-8463.
- ↑ "Life Cycle Assessment of an Enzymatic Ibuprofen Production Process with Automatic Recycling and Purification" (in en). ACS Sustainable Chemistry & Engineering 9 (39): 13135–13150. 4 October 2021. doi:10.1021/acssuschemeng.1c02309. ISSN 2168-0485. https://wrap.warwick.ac.uk/158477/1/WRAP-Life-cycle-assessment-enzymatic-ibuprofen-automatic-recycling-purification-2021.pdf.
- ↑ Elango V, Murphy MA, Smith BL, Davenport KG, "Method for producing ibuprofen", patent US4981995A, issued 1991-01-01
- ↑ "Highly active supported palladium catalyst for the regioselective synthesis of 2-arylpropionic acids by carbonylation". Chemical Communications (12): 1067–1068. 1999. doi:10.1039/a902541c. http://xlink.rsc.org/?DOI=a902541c.
- ↑ "Metabolic inversion of (R)-ibuprofen. Epimerization and hydrolysis of ibuprofenyl-coenzyme A". Drug Metabolism and Disposition 20 (2): 322–327. March–April 1992. PMID 1352228.
- ↑ "Metabolic stereoisomeric inversion of ibuprofen in mammals". Biochimica et Biophysica Acta (BBA) - Protein Structure and Molecular Enzymology 1078 (3): 411–417. July 1991. doi:10.1016/0167-4838(91)90164-U. PMID 1859831. http://ntur.lib.ntu.edu.tw//handle/246246/173009.
- ↑ "Molecular cloning and expression of a 2-arylpropionyl-coenzyme A epimerase: a key enzyme in the inversion metabolism of ibuprofen". Molecular Pharmacology 51 (4): 576–582. April 1997. doi:10.1124/mol.51.4.576. PMID 9106621. http://pdfs.semanticscholar.org/a21e/78f2ae338b18b086911c23ccbbef4fd51275.pdf.
- ↑ "The metabolic chiral inversion and dispositional enantioselectivity of the 2-arylpropionic acids and their biological consequences". Biochemical Pharmacology 37 (1): 105–114. January 1988. doi:10.1016/0006-2952(88)90762-9. PMID 3276314.
- ↑ "On chiral drug action". Medicinal Research Reviews 4 (3): 359–413. 1984. doi:10.1002/med.2610040304. PMID 6087043.
- ↑ "The metabolic chiral inversion of 2-arylpropionic acids--a novel route with pharmacological consequences". The Journal of Pharmacy and Pharmacology 35 (11): 693–704. November 1983. doi:10.1111/j.2042-7158.1983.tb02874.x. PMID 6139449.
- ↑ "The propionic acids: a personal perspective". Journal of Clinical Pharmacology 32 (4): 317–323. April 1992. doi:10.1002/j.1552-4604.1992.tb03842.x. PMID 1569234.
- ↑ 74.0 74.1 "Discovery, mechanisms of action and safety of ibuprofen". International Journal of Clinical Practice. Supplement (135): 3–8. April 2003. PMID 12723739.
- ↑ "Dr Stewart Adams: 'I tested ibuprofen on my hangover'". The Daily Telegraph (UK). 8 October 2007. https://www.telegraph.co.uk/news/health/3351540/Dr-Stewart-Adams-I-tested-ibuprofen-on-my-hangover.html.(Subscription content?)
- ↑ "A brief History of Ibuprofen". 27 July 2017. https://pharmaceutical-journal.com/article/infographics/a-brief-history-of-ibuprofen.
- ↑ "Boots Hidden Heroes - Honoring Dr Stewart Adams". Boots. https://www.boots-uk.com/newsroom/features/boots-hidden-heroes-honouring-dr-stewart-adams/.
- ↑ 78.0 78.1 "Chemical landmark plaque honours scientific discovery past and future" (Press release). Royal Society of Chemistry (RSC). 21 November 2013.
- ↑ "Written submission to the NDAC meeting on risks of NSAIDs presented by the International Ibuprofen Foundation". U.S. Food and Drug Administration (FDA). August 2002. https://www.fda.gov/ohrms/dockets/ac/02/briefing/3882b2_06_international%20ibuprofen%20foundation.htm.
- ↑ "New Drug Application (NDA): 017463". https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=017463.
- ↑ "New Drug Application (NDA): 018989". https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=018989.
- ↑ "Ibuprofen". U.S. Food and Drug Administration (FDA). http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction=Search.SearchAction&SearchTerm=Ibuprofen&SearchType=BasicSearch.
- ↑ "Drug Approval Package: Caldolor (Ibuprofen) NDA #022348". U.S. Food and Drug Administration (FDA). 11 March 2010. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2009/022348_caldolor_toc.cfm.
- ↑ "FDA Approves Injectable Form of Ibuprofen" (Press release). U.S. Food and Drug Administration (FDA). 11 June 2009. Archived from the original on 18 October 2012.
- ↑ "Oral ibuprofen and tetracycline for the treatment of acne vulgaris". Journal of the American Academy of Dermatology 11 (6): 1076–1081. December 1984. doi:10.1016/S0190-9622(84)80192-9. PMID 6239884.
- ↑ "In Japan, an OTC ibuprofen ointment (Fukidia) for alleviating adult acne has been launched". Inpharma Weekly 1 (1530): 18. 25 March 2006. doi:10.2165/00128413-200615300-00043. ISSN 1173-8324.
- ↑ "Renal consequences of nonsteroidal antiinflammatory drugs". Postgraduate Medicine 71 (5): 223–230. May 1982. doi:10.1080/00325481.1982.11716077. PMID 7041104.
- ↑ "Non-steroidal anti-inflammatory drugs as a treatment for Alzheimer's disease: a systematic review and meta-analysis of treatment effect". Drugs & Aging 32 (2): 139–147. February 2015. doi:10.1007/s40266-015-0239-z. PMID 25644018.
- ↑ "Anti-inflammatory drugs and risk of Alzheimer's disease: an updated systematic review and meta-analysis". Journal of Alzheimer's Disease 44 (2): 385–396. 2015. doi:10.3233/JAD-141506. PMID 25227314.
- ↑ "Nonsteroidal antiinflammatory drug use and the risk for Parkinson's disease". Annals of Neurology 58 (6): 963–967. December 2005. doi:10.1002/ana.20682. PMID 16240369.
- ↑ "Is the answer for Parkinson disease already in the medicine cabinet?: Unfortunately not". Neurology 76 (10): 854–855. March 2011. doi:10.1212/WNL.0b013e31820f2e7a. PMID 21368280.
- ↑ "Use of ibuprofen and risk of Parkinson disease". Neurology 76 (10): 863–9. March 2011. doi:10.1212/WNL.0b013e31820f2d79. PMID 21368281.
- ↑ "Parkinson disease: Could over-the-counter treatment protect against Parkinson disease?". Nature Reviews. Neurology 7 (5): 244. May 2011. doi:10.1038/nrneurol.2011.49. PMID 21555992.
- ↑ "Regular nonsteroidal anti-inflammatory drug use and erectile dysfunction". The Journal of Urology 185 (4): 1388–1393. April 2011. doi:10.1016/j.juro.2010.11.092. PMID 21334642.
- ↑ "Herbal medication: potential for adverse interactions with analgesic drugs". Journal of Clinical Pharmacy and Therapeutics 27 (6): 391–401. December 2002. doi:10.1046/j.1365-2710.2002.00444.x. PMID 12472978.
External links
- & John Stuart Nicholson"Anti-Inflammatory Agents" GB patent 971700, published 1964-09-30, assigned to Boots Pure Drug Co Ltd
- "Evidence for the efficacy of pain medications". National Safety Council (NSC). 26 August 2020. https://www.nsc.org/Portals/0/Documents/RxDrugOverdoseDocuments/Evidence-Efficacy-Pain-Medications.pdf.
- "The Ibuprofen Revolution". https://www.science.org/content/blog-post/ibuprofen-revolution.
 |