Chemistry:Hydrocodone
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Hysingla ER, Zohydro ER |
| Other names | Dihydrocodeinone, hydrocodone bitartrate |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a601006 |
| License data |
|
| Pregnancy category |
|
| Dependence liability | High[1] |
| Routes of administration | Clinical: by mouth[2] Others: intranasal, rectal |
| Drug class | Opioid |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | By mouth: 70%[3] |
| Protein binding | Low[3][4] |
| Metabolism | Liver: CYP3A4 (major), CYP2D6 (minor)[5] |
| Metabolites | • Norhydrocodone[5] • Hydromorphone[5] • Others[5] |
| Onset of action | 10–20 minutes[2] |
| Elimination half-life | Average: 3.8 hours[6] Range: 3.3–4.4 hours[2] |
| Duration of action | 4–8 hours[2] |
| Excretion | Urine[7][8] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
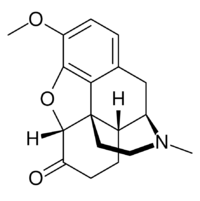
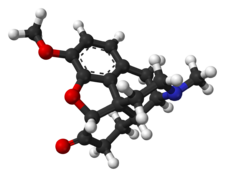
| Chemical and physical data | |
| Formula | C18H21NO3 |
| Molar mass | 299.370 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Hydrocodone, also known as dihydrocodeinone, is a semisynthetic opioid used to treat pain and as a cough suppressant.[9] It is taken by mouth.[9] Typically it is dispensed as the combination acetaminophen/hydrocodone or ibuprofen/hydrocodone for pain severe enough to require an opioid[10][11][12] and in combination with homatropine methylbromide to relieve cough.[9] It is also available by itself in a long-acting form under the brand name Zohydro ER, among others, to treat severe pain of a prolonged duration.[9][13] Hydrocodone is a controlled drug: in the United States a Schedule II Controlled Substance.
Side effects and mechanisms
Common side effects include dizziness, sleepiness, nausea, and constipation.[9] Serious side effects may include low blood pressure, seizures, QT prolongation, respiratory depression, and serotonin syndrome.[9] Rapidly decreasing the dose may result in opioid withdrawal.[9] Use during pregnancy or breastfeeding is generally not recommended.[14] Hydrocodone is believed to work by activating opioid receptors, mainly in the brain and spinal cord.[9] Hydrocodone 10 mg is equivalent to about 10 mg of morphine by mouth.[15]
History and culture
Hydrocodone was patented in 1923, while the long-acting formulation was approved for medical use in the United States in 2013.[9][16] It is most commonly prescribed in the United States, which consumed 99% of the worldwide supply as of 2010.[17] In 2018, it was the 402nd most commonly prescribed medication in the United States, with more than 400,000 prescriptions.[18] Hydrocodone is a semisynthetic opioid, converted from codeine[19][20] or less often from thebaine.[21] Production using genetically engineered yeasts has been developed but is not used commercially.[22][23][24]
Medical uses
Hydrocodone is used to treat moderate to severe pain. In liquid formulations, it is used to treat cough.[9] In one study comparing the potency of hydrocodone to that of oxycodone, it was found that it took 50% more hydrocodone to achieve the same degree of miosis (pupillary contraction).[25] The investigators interpreted this to mean that oxycodone is about 50% more potent than hydrocodone.
However, in a study of emergency department patients with fractures, it was found that an equal amount of either drug provided about the same degree of pain relief, indicating that there is little practical difference between them when used for that purpose.[26] Some references state that the analgesic action of hydrocodone begins in 20–30 minutes and lasts about 4–8 hours.[27] The manufacturer's information says onset of action is about 10-30 minutes and duration is about 4-6 hours.[28] Recommended dosing interval is 4–6 hours. Hydrocodone reaches peak serum levels after 1.3 hours.[29]
Available forms
Hydrocodone is available in a variety of formulations for oral administration:[30][31][32]
- The original oral form of hydrocodone alone, Dicodid, as immediate-release 5- and 10-mg tablets is available for prescription in Continental Europe per national drug control and prescription laws and Title 76 of the Schengen Treaty, but dihydrocodeine has been more widely used for the same indications since the beginning in the early 1920s, with hydrocodone being regulated the same way as morphine in the German Betäubungsmittelgesetz, the similarly named law in Switzerland and the Austrian Suchtmittelgesetz, whereas dihydrocodeine is regulated like codeine. For a number of decades, the liquid hydrocodone products available have been cough medicines.
- Hydrocodone plus homatropine (Hycodan) in the form of small tablets for coughing and especially neuropathic moderate pain (the homatropine, an anticholinergic, is useful in both of those cases and is a deterrent to intentional overdose) was more widely used than Dicodid and was labelled as a cough medicine in the United States whilst Vicodin and similar drugs were the choices for analgesia.
- Extended-release hydrocodone in a time-release syrup also containing chlorphenamine/chlorpheniramine is a cough medicine called Tussionex in North America. In Europe, similar time-release syrups containing codeine (numerous), dihydrocodeine (Paracodin Retard Hustensaft), nicocodeine (Tusscodin), thebacon, acetyldihydrocodeine, dionine, and nicodicodeine are used instead.
- Immediate-release hydrocodone with paracetamol (acetaminophen) (Vicodin, Lortab, Lorcet, Maxidone, Norco, Zydone)
- Immediate-release hydrocodone with ibuprofen (Vicoprofen, Ibudone, Reprexain)
- Immediate-release hydrocodone with aspirin (Alor 5/500, Azdone, Damason-P, Lortab ASA, Panasal 5/500)
- Controlled-release hydrocodone (Hysingla ER by Purdue Pharma, Zohydro ER)[33]
Hydrocodone is not available in parenteral or any other non-oral forms.[4][2]
Side effects
Common side effects of hydrocodone are nausea, vomiting, constipation, drowsiness, dizziness, lightheadedness, anxiety, abnormally happy or sad mood, dry throat, difficulty urinating, rash, itching, and contraction of the pupils. Serious side effects include slowed or irregular breathing and chest tightness.[34]
Several cases of progressive bilateral hearing loss unresponsive to steroid therapy have been described as an infrequent adverse reaction to hydrocodone/paracetamol misuse. This adverse effect has been considered by some to be due to the ototoxicity of hydrocodone.[35][36] Other researchers have suggested that paracetamol is the primary agent responsible for the ototoxicity.[37][38]
The U.S. Food and Drug Administration (FDA) assigns the drug to pregnancy category C, meaning that no adequate and well-controlled studies in humans have been conducted. A newborn of a mother taking opioid medications regularly prior to the birth will be physically dependent.[39][40] The baby may also exhibit respiratory depression if the opioid dose was high.[41] An epidemiological study indicated that opioid treatment during early pregnancy results in increased risk of various birth defects.[42]
Symptoms of hydrocodone overdose include narrowed or widened pupils; slow, shallow, or stopped breathing; slowed or stopped heartbeat; cold, clammy, or blue skin; excessive sleepiness; loss of consciousness; seizures; or death.[34]
Hydrocodone can be habit forming, causing physical and psychological dependence. Its abuse liability is similar to morphine and less than oxycodone.[43]
Interactions
Hydrocodone is metabolized by the cytochrome P450 enzymes CYP2D6 and CYP3A4, and inhibitors and inducers of these enzymes can modify hydrocodone exposure.[44] One study found that combination of paroxetine, a selective serotonin reuptake inhibitor (SSRI) and strong CYP2D6 inhibitor, with once-daily extended-release hydrocodone, did not modify exposure to hydrocodone or the incidence of adverse effects.[44][45] These findings suggest that hydrocodone can be coadministered with CYP2D6 inhibitors without dosage modification.[44][45] Conversely, combination of hydrocodone/acetaminophen with the antiviral regimen of ombitasvir, paritaprevir, ritonavir, and dasabuvir for treatment of hepatitis C increased peak concentrations of hydrocodone by 27%, total exposure by 90%, and elimination half-life from 5.1 hours to 8.0 hours.[46] Ritonavir is a strong CYP3A4 inhibitor as well as inducer of CYP3A and other enzymes, and the other antivirals are known to inhibit drug transporters like organic anion transporting polypeptide (OATP) 1B1 and 1B3, P-glycoprotein, and breast cancer resistance protein (BCRP).[46] The changes in hydrocodone levels are consistent with CYP3A4 inhibition by ritonavir.[46] Based on these findings, a 50% lower dose of hydrocodone and closer clinical monitoring was recommended when hydrocodone is used in combination with this antiviral regimen.[46]
People consuming alcohol, other opioids, anticholinergic antihistamines, antipsychotics, anxiolytics, or other central nervous system (CNS) depressants together with hydrocodone may exhibit an additive CNS depression.[41] Hydrocodone taken concomitantly with serotonergic medications like SSRI antidepressants may increase the risk of serotonin syndrome.[47]
Pharmacology
Pharmacodynamics
| Compound | Affinities (Ki) | Ratio | Ref | ||
|---|---|---|---|---|---|
| MOR | DOR | KOR | MOR:DOR:KOR | ||
| Hydrocodone | 11.1 nM | 962 nM | 501 nM | 1:87:45 | [48] |
| Hydromorphone | 0.47 nM | 18.5 nM | 24.9 nM | 1:39:53 | [49] |
| Compound | Route | Dose |
|---|---|---|
| Codeine | PO | 200 mg |
| Hydrocodone | PO | 20–30 mg |
| Hydromorphone | PO | 7.5 mg |
| Hydromorphone | IV | 1.5 mg |
| Morphine | PO | 30 mg |
| Morphine | IV | 10 mg |
| Oxycodone | PO | 20 mg |
| Oxycodone | IV | 10 mg |
| Oxymorphone | PO | 10 mg |
| Oxymorphone | IV | 1 mg |
Hydrocodone is a highly selective full agonist of the μ-opioid receptor (MOR).[27][53][48] This is the main biological target of the endogenous opioid neuropeptide β-endorphin.[54] Hydrocodone has low affinity for the δ-opioid receptor (DOR) and the κ-opioid receptor (KOR), where it is an agonist similarly.[48]
Studies have shown hydrocodone is stronger than codeine but only one-tenth as potent as morphine at binding to receptors and reported to be only 59% as potent as morphine in analgesic properties. However, in tests conducted on rhesus monkeys, the analgesic potency of hydrocodone was actually higher than morphine.[6] Oral hydrocodone has a mean equivalent daily dosage (MEDD) factor of 0.4, meaning that 1 mg of hydrocodone is equivalent to 0.4 mg of intravenous morphine. However, because of morphine's low oral bioavailability, there is a 1:1 correspondence between orally administered morphine and orally administered hydrocodone.[55]
Pharmacokinetics
Absorption
Hydrocodone is only pharmaceutically available as an oral medication.[2] It is well-absorbed, but the oral bioavailability of hydrocodone is only approximately 25%.[3][4] The onset of action of hydrocodone via this route is 10 to 20 minutes, with a peak effect (Tmax) occurring at 30 to 60 minutes,[50] and it has a duration of 4 to 8 hours.[2] The FDA label for immediate-release hydrocodone with acetaminophen does not include any information on the influence of food on its absorption or other pharmacokinetics.[56] Conversely, coadministration with a high-fat meal increases peak concentrations of different formulations of extended-release hydrocodone by 14 to 54%, whereas area-under-the-curve levels are not notably affected.[57][58][59][60]
Distribution
The volume of distribution of hydrocodone is 3.3 to 4.7 L/kg.[4] The plasma protein binding of hydrocodone is 20 to 50%.[27]
Metabolism
In the liver, hydrocodone is transformed into several metabolites, including norhydrocodone, hydromorphone, 6α-hydrocodol (dihydrocodeine), and 6β-hydrocodol.[5] 6α- and 6β-hydromorphol are also formed, and the metabolites of hydrocodone are conjugated (via glucuronidation).[61][62] Hydrocodone has a terminal half-life that averages 3.8 hours (range 3.3–4.4 hours).[6][2] The hepatic cytochrome P450 enzyme CYP2D6 converts hydrocodone into hydromorphone, a more potent opioid (5-fold higher binding affinity to the MOR).[5][63] However, extensive and poor cytochrome 450 CYP2D6 metabolizers had similar physiological and subjective responses to hydrocodone, and CYP2D6 inhibitor quinidine did not change the responses of extensive metabolizers, suggesting that inhibition of CYP2D6 metabolism of hydrocodone has no practical importance.[64][65] Ultra-rapid CYP2D6 metabolizers (1–2% of the population) may have an increased response to hydrocodone; however, hydrocodone metabolism in this population has not been studied.[66]
Norhydrocodone, the major metabolite of hydrocodone, is predominantly formed by CYP3A4-catalyzed oxidation.[5] In contrast to hydromorphone, it is described as inactive.[63] However, norhydrocodone is actually a MOR agonist with similar potency to hydrocodone, but has been found to produce only minimal analgesia when administered peripherally to animals (likely due to poor blood–brain barrier and thus central nervous system penetration).[67] Inhibition of CYP3A4 in a child who was, in addition, a poor CYP2D6 metabolizer, resulted in a fatal overdose of hydrocodone.[68] Approximately 40% of hydrocodone metabolism is attributed to non-cytochrome P450-catalyzed reactions.[69]
Elimination
Hydrocodone is excreted in urine, mainly in the form of conjugates.[7][8]
Chemistry
Detection in body fluids
Hydrocodone concentrations are measured in blood, plasma, and urine to seek evidence of misuse, to confirm diagnoses of poisoning, and to assist in investigations into deaths. Many commercial opiate screening tests react indiscriminately with hydrocodone, other opiates, and their metabolites, but chromatographic techniques can easily distinguish hydrocodone uniquely. Blood and plasma hydrocodone concentrations typically fall into the 5–30 µg/L range among people taking the drug therapeutically, 100–200 µg/L among recreational users, and 100–1,600 µg/L in cases of acute, fatal overdosage. Co-administration of the drug with food or alcohol can very significantly increase the resulting plasma hydrocodone concentrations that are subsequently achieved.[70][71]
Synthesis
Hydrocodone is most commonly synthesized from thebaine, a constituent of opium latex from the dried poppy plant. Once thebaine is obtained, the reaction undergoes hydrogenation using a palladium catalyst.[72]
Structure
There are three important structures in hydrocodone: the amine group, which binds to the tertiary nitrogen binding site in the central nervous system's opioid receptor, the hydroxy group that binds to the anionic binding side, and the phenyl group which binds to the phenolic binding site.[73] This triggers a G protein activation and subsequent release of dopamine.[74]
History
Hydrocodone was first synthesized in Germany in 1920 by Carl Mannich and Helene Löwenheim.[75] It was approved by the Food and Drug Administration on 23 March 1943 for sale in the United States and approved by Health Canada for sale in Canada under the brand name Hycodan.[76][77]
Hydrocodone was first marketed by Knoll as Dicodid, starting in February 1924 in Germany. This name is analogous to other products the company introduced or otherwise marketed: Dilaudid (hydromorphone, 1926), Dinarkon (oxycodone, 1917), Dihydrin (dihydrocodeine, 1911), and Dimorphan (dihydromorphine). Paramorfan is the trade name of dihydromorphine from another manufacturer, as is Paracodin, for dihydrocodeine.[78][79]
The name Dicodid was registered in the United States and appears without a monograph as late as 1978 in the Physicians' Desk Reference; Dicodid may have been marketed to one extent or another in North America in the 1920s and early 1930s. The drug was pure hydrocodone in small 5 and 10 mg tablets, physically similar to the Dilaudid tablets. It is no longer manufactured by Knoll in Germany, nor is a generic available. Hydrocodone was never as common in Europe as it is in North America—dihydrocodeine is used for its spectrum of indications. Germany was the number two consumer of hydrocodone until the manufacture of the drug was discontinued there. Now,[when?] the world outside the United States accounts for less than 1% of annual consumption. It was listed as a Suchtgift under the German Betäubungsmittelgesetz and regulated like morphine. It became available in the Schengen Area of the European Union as of 1 January 2002 under Title 76 of the Schengen Treaty.[citation needed]
Society and culture
Formulations
Several common imprints for hydrocodone are M365, M366, M367.[80]
Combination products
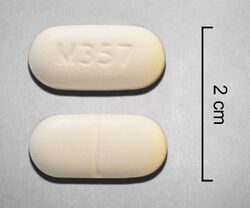
Most hydrocodone formulations include a second analgesic, such as paracetamol (acetaminophen) or ibuprofen. Examples of hydrocodone combinations include Norco, Vicodin, Vicoprofen and Riboxen.[81]
Legal status
United States
The US government imposed tougher prescribing rules for hydrocodone in 2014, changing the drug from Schedule III to Schedule II.[82][83][84][85] In 2011, hydrocodone products were involved in around 100,000 abuse-related emergency department visits in the United States, more than double the number in 2004.[86]
References
- ↑ Today's Medical Assistant: Clinical and Administrative Procedures. Elsevier Health Sciences. 2012. p. 571. ISBN 9781455701506. https://books.google.com/books?id=YalYPI1KqTQC&pg=PA571.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 "Opioids in the management of acute pain". Handbook of Acute Pain Management. CRC Press. 19 April 2016. pp. 79–. ISBN 978-1-4665-9635-1. https://books.google.com/books?id=Em7OBQAAQBAJ&pg=PA79.
- ↑ 3.0 3.1 3.2 "Analgesic Agents in Rheumatic Disease". Kelley and Firestein's Textbook of Rheumatology. Elsevier Health Sciences. 21 June 2016. pp. 1081–. ISBN 978-0-323-41494-4. https://books.google.com/books?id=kBZ6DAAAQBAJ&pg=PA1081.
- ↑ 4.0 4.1 4.2 4.3 "Chapter 37: Drug Therapy of Pain in Cancer Patients". Cancer Chemotherapy and Biotherapy: Principles and Practice. Lippincott Williams & Wilkins. 8 November 2010. pp. 700–. ISBN 978-1-60547-431-1. https://books.google.com/books?id=WL4arNFsQa8C&pg=PA700.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 "Substrates of Human CYP2D6: Opioids and Opioid Receptor Antagonists". Cytochrome P450 2D6: Structure, Function, Regulation and Polymorphism. CRC Press. 6 April 2016. pp. 164–. ISBN 978-1-4665-9788-4. https://books.google.com/books?id=UJqmCwAAQBAJ&pg=PA164.
- ↑ 6.0 6.1 6.2 Opioids in Cancer Pain. Oxford University Press. 2005. pp. 59–68. ISBN 978-0-19-852943-9. https://books.google.com/books?id=BK0WduGnx2kC&pg=PA59.
- ↑ 7.0 7.1 Toxicology and Drug Testing, An Issue of Clinics in Laboratory Medicine, E-Book. Elsevier Health Sciences. 16 November 2016. pp. 85–. ISBN 978-0-323-47795-6. https://books.google.com/books?id=NAKRDQAAQBAJ&pg=PT85.
- ↑ 8.0 8.1 Opioid Therapy in the 21st Century. OUP USA. 21 February 2013. pp. 68–. ISBN 978-0-19-984497-5. https://books.google.com/books?id=MBxWFigSEE8C&pg=PT68.
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 "Hydrocodone Bitartrate Monograph for Professionals". American Society of Health-System Pharmacists. https://www.drugs.com/monograph/hydrocodone-bitartrate.html.
- ↑ Mallinckrodt (March 10, 2021). "HYDROCODONE BITARTRATE AND ACETAMINOPHEN tablet (label)". https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=73c1059b-0c7d-42ef-9827-f018858fc447.
- ↑ Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk. Lippincott Williams & Wilkins. 2011. p. 692. ISBN 9781608317080. https://books.google.com/books?id=OIgTE4aynrMC&pg=PA692.
- ↑ "Hydrocodone Combination Products: MedlinePlus Drug Information" (in en). https://medlineplus.gov/druginfo/meds/a601006.html.
- ↑ "Hydrocodone: MedlinePlus Drug Information". https://medlineplus.gov/druginfo/meds/a614045.html.
- ↑ "Hydrocodone Use During Pregnancy". https://www.drugs.com/pregnancy/hydrocodone.html.
- ↑ "Opioid Dose Calculator". http://www.agencymeddirectors.wa.gov/calculator/dosecalculator.htm.
- ↑ Analogue-based Drug Discovery. John Wiley & Sons. 2006. p. 526. ISBN 9783527607495. https://books.google.com/books?id=FjKfqkaKkAAC&pg=PA526.
- ↑ "Making Some Painkillers Harder to Get". The New York Times. 21 February 2013. https://www.nytimes.com/2013/02/22/opinion/making-some-painkillers-harder-to-get.html.
- ↑ "Hydrocodone - Drug Usage Statistics". https://clincalc.com/DrugStats/Drugs/Hydrocodone.
- ↑ General, Organic, and Biological Chemistry. Cengage Learning. 2012. p. 567. ISBN 9781133711285. https://books.google.com/books?id=lPltCgAAQBAJ&pg=PA567.
- ↑ (in en) Synthesis of Essential Drugs. Elsevier. 2006-03-10. ISBN 978-0-08-046212-7. https://books.google.com/books?id=Jjc7KYWZdOYC&q=hydrocodone.
- ↑ Narcotic Drugs 2020, Estimated World Requirements for 2021, Statistics for 2019. International Narcotics Control Board. 2020. pp. 37. ISBN 978-92-1-148355-0. https://www.incb.org/documents/Narcotic-Drugs/Technical-Publications/2020/Narcotic_Drugs_Technical_publication_2020.pdf. "Thebaine itself is not used in therapy, but it is an important starting material for the manufacture of a number of opioids, mainly codeine, dihydrocodeine, etorphine, hydrocodone, oxycodone and oxymorphone..."
- ↑ "Complete biosynthesis of opioids in yeast". Science 349 (6252): 1095–1100. September 2015. doi:10.1126/science.aac9373. PMID 26272907. Bibcode: 2015Sci...349.1095G.
- ↑ "A microbial biomanufacturing platform for natural and semisynthetic opioids". Nature Chemical Biology 10 (10): 837–844. October 2014. doi:10.1038/nchembio.1613. PMID 25151135.
- ↑ "Total biosynthesis of opiates by stepwise fermentation using engineered Escherichia coli". Nature Communications 7 (1): 10390. February 2016. doi:10.1038/ncomms10390. PMID 26847395. Bibcode: 2016NatCo...710390N.
- ↑ "Within-subject comparison of the psychopharmacological profiles of oral hydrocodone and oxycodone combination products in non-drug-abusing volunteers". Drug and Alcohol Dependence 101 (1–2): 107–114. April 2009. doi:10.1016/j.drugalcdep.2008.11.013. PMID 19118954. https://zenodo.org/record/896375.
- ↑ "Comparison of oxycodone and hydrocodone for the treatment of acute pain associated with fractures: a double-blind, randomized, controlled trial". Academic Emergency Medicine 12 (4): 282–288. April 2005. doi:10.1197/j.aem.2004.12.005. PMID 15805317.
- ↑ 27.0 27.1 27.2 "Pharmacology of opioids in the treatment of chronic pain syndromes". Pain Physician 14 (4): E343–E360. 2011. doi:10.36076/ppj.2011/14/E343. PMID 21785485.
- ↑ "Opioid (Narcotic Analgesics and Acetaminophen Systemic )". https://www.drugs.com/mmx/vicodin.html.
- ↑ "Labeling-Package Insert: Hydrocodone/acetaminophen 7.5 mg/325 mg". Chartwell. October 18, 2013. https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/040432s006,40556s012,40658s006,%2040846s005,%2089699s044lbl.pdf.
- ↑ "Appendix: Opioid Formulations". Demystifying Opioid Conversion Calculations: A Guide for Effective Dosing. ASHP. 24 August 2009. pp. 187–188. ISBN 978-1-58528-297-5. https://books.google.com/books?id=6oBA9z5wl9wC&pg=PA187.
- ↑ PeriAnesthesia Nursing: A Critical Care Approach. Elsevier Health Sciences. 11 February 2008. pp. 751–. ISBN 978-1-4377-2610-7. https://books.google.com/books?id=2DxxrrJafncC&pg=PT751.
- ↑ "Hydrocodone". Mosby's Drug Guide for Nursing Students, with 2014 Update. Elsevier Health Sciences. 27 June 2013. pp. 524–. ISBN 978-0-323-22268-6. https://books.google.com/books?id=r71EBAAAQBAJ&pg=PA524.
- ↑ "The Clinical Applications of Extended-Release Abuse-Deterrent Opioids". CNS Drugs 30 (7): 637–646. July 2016. doi:10.1007/s40263-016-0357-0. PMID 27290716.
- ↑ 34.0 34.1 "Hydrocodone Combination Products". MedlinePlus. U.S. National Library of Medicine. 1 October 2008. https://www.nlm.nih.gov/medlineplus/druginfo/meds/a601006.html.
- ↑ "Profound hearing loss associated with hydrocodone/acetaminophen abuse". The American Journal of Otology 21 (2): 188–191. March 2000. doi:10.1016/S0196-0709(00)80007-1. PMID 10733182.
- ↑ "Hydrocodone use and sensorineural hearing loss". Pain Physician 10 (3): 467–472. May 2007. PMID 17525781. http://www.painphysicianjournal.com/linkout_vw.php?issn=1533-3159&vol=10&page=467.
- ↑ "Acetaminophen ototoxicity after acetaminophen/hydrocodone abuse: evidence from two parallel in vitro mouse models". Otolaryngology--Head and Neck Surgery 142 (6): 814–9, 819.e1–2. June 2010. doi:10.1016/j.otohns.2010.01.010. PMID 20493351.
- ↑ "Analgesic use and the risk of hearing loss in men". The American Journal of Medicine 123 (3): 231–237. March 2010. doi:10.1016/j.amjmed.2009.08.006. PMID 20193831.
- ↑ "Neonatal abstinence syndrome: MedlinePlus Medical Encyclopedia" (in en). https://medlineplus.gov/ency/article/007313.htm.
- ↑ "Opioid Use and Opioid Use Disorder in Pregnancy" (in en). https://www.acog.org/en/clinical/clinical-guidance/committee-opinion/articles/2017/08/opioid-use-and-opioid-use-disorder-in-pregnancy.
- ↑ 41.0 41.1 "REPREXAIN (hydrocodone bitartrate, ibuprofen) tablet, film coated". NIH. http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=7b71e4c3-86f2-464a-b0a9-4f98adfef9c5.
- ↑ "Maternal treatment with opioid analgesics and risk for birth defects". American Journal of Obstetrics and Gynecology 204 (4): 314.e1–314.11. April 2011. doi:10.1016/j.ajog.2010.12.039. PMID 21345403.
- ↑ "Likeability and abuse liability of commonly prescribed opioids". Journal of Medical Toxicology 8 (4): 335–340. December 2012. doi:10.1007/s13181-012-0263-x. PMID 22992943.
- ↑ 44.0 44.1 44.2 "Opioid analgesics-related pharmacokinetic drug interactions: from the perspectives of evidence based on randomized controlled trials and clinical risk management". Journal of Pain Research 10: 1225–1239. 2017. doi:10.2147/JPR.S138698. PMID 28579821.
- ↑ 45.0 45.1 "Effects of paroxetine, a CYP2D6 inhibitor, on the pharmacokinetic properties of hydrocodone after coadministration with a single-entity, once-daily, extended-release hydrocodone tablet". Clinical Therapeutics 37 (10): 2286–2296. October 2015. doi:10.1016/j.clinthera.2015.08.007. PMID 26350273.
- ↑ 46.0 46.1 46.2 46.3 "Drug-Drug Interactions Between the Anti-Hepatitis C Virus 3D Regimen of Ombitasvir, Paritaprevir/Ritonavir, and Dasabuvir and Eight Commonly Used Medications in Healthy Volunteers". Clinical Pharmacokinetics 55 (8): 1003–1014. August 2016. doi:10.1007/s40262-016-0373-8. PMID 26895022.
- ↑ "The serotonin syndrome". The New England Journal of Medicine 352 (23): 2454–6; author reply 2454–6. June 2005. doi:10.1056/NEJM200506093522320. PMID 15948273.
- ↑ 48.0 48.1 48.2 "Serotonin and norepinephrine uptake inhibiting activity of centrally acting analgesics: structural determinants and role in antinociception". The Journal of Pharmacology and Experimental Therapeutics 274 (3): 1263–1270. September 1995. PMID 7562497. http://jpet.aspetjournals.org/content/274/3/1263.short.
- ↑ "Molecular determinants of non-specific recognition of delta, mu, and kappa opioid receptors". Bioorganic & Medicinal Chemistry 9 (1): 69–76. January 2001. doi:10.1016/S0968-0896(00)00223-6. PMID 11197347.
- ↑ 50.0 50.1 "Analgesia and Anesthesia". Pharmacology for Women's Health. Jones & Bartlett Publishers. 25 October 2010. pp. 332–. ISBN 978-1-4496-1073-9. https://books.google.com/books?id=o_rHHCsIpckC&pg=PA332.
- ↑ "Chapter 27 Postoperative and Chronic Pain: Systemic and Regional Analgesic Techniques". Chestnut's Obstetric Anesthesia: Principles and Practice E-Book. Elsevier Health Sciences. 28 February 2014. pp. 611–. ISBN 978-0-323-11374-8. https://books.google.com/books?id=FMU0AwAAQBAJ&pg=PA611.
- ↑ "Opiod Analgesics". Havard's Nursing Guide to Drugs. Elsevier Health Sciences. 1 June 2013. pp. 933–. ISBN 978-0-7295-8162-2. https://books.google.com/books?id=XpzQAgAAQBAJ&pg=PA933.
- ↑ "Activation of G-proteins by morphine and codeine congeners: insights to the relevance of O- and N-demethylated metabolites at mu- and delta-opioid receptors". The Journal of Pharmacology and Experimental Therapeutics 308 (2): 547–554. February 2004. doi:10.1124/jpet.103.058602. PMID 14600248.
- ↑ "Palliative Medicine". Essentials of Internal Medicine (3rd ed.). Elsevier Health Sciences. 10 February 2015. pp. 491–. ISBN 978-0-7295-8081-6. https://books.google.com/books?id=0Zq9BwAAQBAJ&pg=PA491.
- ↑ "Instructions for Mean Equivalent Daily Dose (MEDD)". http://www.palliative.org/PC/ClinicalInfo/AssessmentTools/MeanEquivalent%20for%20program%20v3.pdf.
- ↑ https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/040099s023lbl.pdf
- ↑ "The effects of food on opioid-induced nausea and vomiting and pharmacological parameters: a systematic review". Postgraduate Medicine 129 (7): 698–708. September 2017. doi:10.1080/00325481.2017.1345282. PMID 28635354.
- ↑ "Effect of Food on the Pharmacokinetics of Single- and Multiple-Dose Hydrocodone Extended Release in Healthy Subjects". Clinical Drug Investigation 37 (12): 1153–1163. December 2017. doi:10.1007/s40261-017-0575-3. PMID 28948482.
- ↑ "Effects of food and alcohol on the pharmacokinetics of an oral, extended-release formulation of hydrocodone in healthy volunteers". Clinical Pharmacology 7: 1–9. 2015. doi:10.2147/CPAA.S70831. PMID 25653563.
- ↑ "Single-dose pharmacokinetics of 2 or 3 tablets of biphasic immediate-release/extended-release hydrocodone bitartrate/acetaminophen (MNK-155) under fed and fasted conditions: two randomized open-label trials". BMC Pharmacology & Toxicology 16: 31. November 2015. doi:10.1186/s40360-015-0032-y. PMID 26614499.
- ↑ "Pharmacokinetics of Specific Drugs". Pharmacokinetics and Pharmacodynamics of Abused Drugs. CRC Press. 9 October 2007. pp. 56–. ISBN 978-1-4200-5460-6. https://books.google.com/books?id=9fwUQvF4r-cC&pg=PA56.
- ↑ "Challenges in Confirmation Testing for Drugs of Abuse". Accurate Results in the Clinical Laboratory: A Guide to Error Detection and Correction. Newnes. 22 January 2013. pp. 239–. ISBN 978-0-12-415858-0. https://books.google.com/books?id=HEBloh3nxiAC&pg=PA239.
- ↑ 63.0 63.1 "Genetic Aspect of Opiate Metabolism and Addiction". Pharmacogenomics of Alcohol and Drugs of Abuse. CRC Press. 23 April 2012. pp. 175–. ISBN 978-1-4398-5611-6. https://books.google.com/books?id=AiHaRjs3grYC&pg=PA175.
- ↑ "Inhibition of cytochrome P450 2D6 metabolism of hydrocodone to hydromorphone does not importantly affect abuse liability". The Journal of Pharmacology and Experimental Therapeutics 281 (1): 103–108. April 1997. PMID 9103485.
- ↑ "Pharmacogenetics, drug-metabolizing enzymes, and clinical practice". Pharmacological Reviews 58 (3): 521–590. September 2006. doi:10.1124/pr.58.3.6. PMID 16968950.
- ↑ "Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines for codeine therapy in the context of cytochrome P450 2D6 (CYP2D6) genotype". Clinical Pharmacology and Therapeutics 91 (2): 321–326. February 2012. doi:10.1038/clpt.2011.287. PMID 22205192.
- ↑ "Fatal hydrocodone overdose in a child: pharmacogenetics and drug interactions". Pediatrics 126 (4): e986–e989. October 2010. doi:10.1542/peds.2009-1907. PMID 20837591.
- ↑ "Pharmacogenomic considerations in opioid analgesia". Pharmacogenomics and Personalized Medicine 5: 73–87. 2012. doi:10.2147/PGPM.S23422. PMID 23226064.
- ↑ "Postmortem oxycodone and hydrocodone blood concentrations". Journal of Forensic Sciences 48 (2): 429–431. March 2003. doi:10.1520/JFS2002309. PMID 12665006.
- ↑ Disposition of Toxic Drugs and Chemicals in Man. Biomedical Publications. 2017. pp. 1050–1052. ISBN 978-0-692-77499-1. https://books.google.com/books?id=AoKctAEACAAJ.
- ↑ "One-pot conversion of thebaine to hydrocodone and synthesis of neopinone ketal". The Journal of Organic Chemistry 74 (2): 747–752. January 2009. doi:10.1021/jo802454v. PMID 19072148.
- ↑ The Essence of Analgesia and Analgesics. Cambridge: Cambridge University Press. 6 December 2010. pp. 73, 81. ISBN 9780511841378.
- ↑ Neuroscience in the 21st Century. New York, NY: Springer. 27 October 2016. pp. 3626, 3657. ISBN 978-1-4939-3474-4.
- ↑ "Ueber zwei neue Reduktionsprodukte des Kodeins". Archiv der Pharmazie 258 (2–4): 295–316. 1920. doi:10.1002/ardp.19202580218. ISSN 0365-6233. https://zenodo.org/record/1424591.
- ↑ "Drugs@FDA—Approval History: Hycodan". FDA. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction=Search.Overview&DrugName=HYCODAN.
- ↑ "FDA Docket No. 2007N-0353, Drug Products Containing Hydrocodone; Enforcement Action Dates". FDA. https://www.fda.gov/OHRMS/DOCKETS/98fr/E7-19340.htm. See section I. B., DESI Review of Hydrocodone Products
- ↑ "Dihydromorphine" (in en). PubChem. U.S. National Library of Medicine. https://pubchem.ncbi.nlm.nih.gov/compound/5359421.
- ↑ "Dihydrocodeine". PubChem. U.S. National Library of Medicine. https://pubchem.ncbi.nlm.nih.gov/compound/5284543.
- ↑ International Narcotics Control Board Report 2008. United Nations Pubns. 2009. p. 20. ISBN 978-9211482324. https://books.google.com/books?id=7iDhYnsYaocC&pg=PA20.[yes|permanent dead link|dead link}}]
- ↑ "Hydrocodone Combination Products". The American Society of Health-System Pharmacists, Inc.. https://medlineplus.gov/druginfo/meds/a601006.html.
- ↑ "Prescriptions for hydrocodone plummet after US tightens prescribing rules". BMJ 352: i549. January 2016. doi:10.1136/bmj.i549. PMID 26819247.
- ↑ "Effect of US Drug Enforcement Administration's Rescheduling of Hydrocodone Combination Analgesic Products on Opioid Analgesic Prescribing". JAMA Internal Medicine 176 (3): 399–402. March 2016. doi:10.1001/jamainternmed.2015.7799. PMID 26809459.
- ↑ "An Online Survey of Patients' Experiences Since the Rescheduling of Hydrocodone: The First 100 Days". Pain Medicine 17 (9): 1686–1693. September 2016. doi:10.1093/pm/pnv064. PMID 26814291.
- ↑ "Schedules of Controlled Substances: Rescheduling of Hydrocodone Combination Products From Schedule III to Schedule II". Federal Register. 22 August 2014. https://www.federalregister.gov/documents/2014/08/22/2014-19922/schedules-of-controlled-substances-rescheduling-of-hydrocodone-combination-products-from-schedule.
- ↑ "Drug-Related Hospital Emergency Room Visits". National Institute on Drug Abuse. https://www.drugabuse.gov/publications/drugfacts/drug-related-hospital-emergency-room-visits.
External links
- "Hydrocodone". Drug Information Portal. U.S. National Library of Medicine. https://druginfo.nlm.nih.gov/drugportal/name/hydrocodone.
- "DEA Schedules of Controlled Substances: Rescheduling of Hydrocodone Combination Products From Schedule III to Schedule II". Federal Register. 6 October 2014. https://www.federalregister.gov/articles/2014/08/22/2014-19922/schedules-of-controlled-substances-rescheduling-of-hydrocodone-combination-products-from-schedule#h-27.
 |
