Medicine:Pacemaker current
The pacemaker current (If, or IKf, also called funny current) is an electric current in the heart that flows through the HCN channel or pacemaker channel. Such channels are important parts of the electrical conduction system of the heart and form a component of the natural pacemaker.
First described in the late 1970s in Purkinje fibers and sinoatrial myocytes, the cardiac pacemaker "funny" (If) current has been extensively characterized and its role in cardiac pacemaking has been investigated.[1][2][3] Among the unusual features which justified the name "funny" are mixed Na+ and K+ permeability, activation on hyperpolarization, and very slow kinetics.[1]
Function
The funny current is highly expressed in spontaneously active cardiac regions, such as the sinoatrial node (SAN, the natural pacemaker region), the atrioventricular node (AVN) and the Purkinje fibres of conduction tissue. The funny current is a mixed sodium–potassium current that activates upon hyperpolarization at voltages in the diastolic range (normally from −60/−70 mV to −40 mV). When, at the end of a sinoatrial action potential, the membrane repolarizes below the If threshold (about −40/−50 mV), the funny current is activated and supplies inward current, which is responsible for starting the diastolic depolarization phase (DD); by this mechanism, the funny current controls the rate of spontaneous activity of sinoatrial myocytes, and thus the cardiac rate. The reversal potential of the funny current lies between -20 and -10 mV. [4]
Another unusual feature of If is its dual activation by voltage and by cyclic nucleotides. Cyclic adenosine monophosphate (cAMP) molecules bind directly to f-channels and increase their open probability.[5] cAMP dependence is a particularly relevant physiological property, since it underlies the If-dependent autonomic regulation of heart rate. Sympathetic stimulation raises the level of cAMP-molecules which bind to f-channels and shift the If activation range to more positive voltages; this mechanism leads to an increase of the current at diastolic voltages and therefore to an increase of the steepness of DD and heart rate acceleration.
Parasympathetic stimulation (which acts to increase probability of potassium channels opening but decreases the probability of calcium channel opening) decreases the heart rate by the opposite action, that is by shifting the If activation curve towards more negative voltages. When vagally-released acetylcholine (ACh) binds to muscarinic M2 receptors, this promotes dissociation of βγ subunit complexes, leading to direct opening of the G-protein–gated inwardly rectifying K+ channel (Girk/Kir) IKACh.[6]
Related currents
A similar current, termed Ih (hyperpolarization-activated), has also been described in different types of neurons, where it has a variety of functions, including the contribution to control of rhythmic firing, regulation of neuronal excitability, sensory transduction, synaptic plasticity and more.[7]
Molecular determinants
The molecular determinants of the pacemaker current belong to the HCN channel (hyperpolarization-activated cyclic nucleotide–gated channel), of which 4 isoforms (HCN1 to HCN4) are known. Based on their sequence, HCN channels are classified as members of the superfamily of voltage-gated K+ (Kv) and CNG channels.[3][8]
Clinical significance
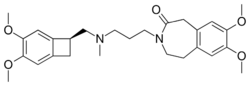
Because of their relevance to generation of pacemaker activity and modulation of spontaneous frequency, f-channels are natural targets of drugs aimed to pharmacologically control heart rate. Several agents called "heart rate reducing agents" act by specifically inhibiting f-channel function.[3] Ivabradine is the most specific and selective If inhibitor and the only member of this family that is now marketed for pharmacological treatment of chronic stable angina in patients with normal sinus rhythm who have a contraindication or intolerance to beta-blockers. Recent studies have also indicated that funny channel inhibition can be used to reduce the incidence of coronary artery disease outcomes in a subgroup of patients with heart rate ≥70 bpm.[9]
Cardiovascular diseases represent a major cause of worldwide mortality, and the relevance of the genetic component in these diseases has recently become more apparent. Genetic alterations of HCN4 channels (the molecular correlate of sinoatrial f-channels) coupled to rhythm disturbances have been reported in humans. For example, an inherited mutation of a highly conserved residue in the CNBD of the HCN4 protein (S672R) is associated with inherited sinus bradycardia.[10] In vitro studies indicate that the S672R mutation causes a hyperpolarizing shift of the HCN4 channel open probability curve of about 5 mV in heterozygosis, an effect similar to the hyperpolarizing shift caused by parasympathetic stimulation and able to explain a reduction of inward current during diastole and the resulting slower spontaneous rate.[citation needed]
Biological pacemakers, generally intended as cell substrates able to induce spontaneous activity in silent tissue, represent a potential tool to overcome the limitations of electronic pacemakers. One of the strategies used to generate biological pacemakers involves the use of cells inherently expressing or engineered to express funny channels. Different types of stem cells can be used for this purpose.[8]
See also
References
- ↑ 1.0 1.1 "How does adrenaline accelerate the heart?". Nature 280 (5719): 235–6. July 1979. doi:10.1038/280235a0. PMID 450140. Bibcode: 1979Natur.280..235B.
- ↑ "Properties of the current if in the sino-atrial node of the rabbit compared with those of the current iK, in Purkinje fibres". The Journal of Physiology 308: 353–67. November 1980. doi:10.1113/jphysiol.1980.sp013475. PMID 6262501.
- ↑ 3.0 3.1 3.2 "Physiology and pharmacology of the cardiac pacemaker ("funny") current". Pharmacology & Therapeutics 107 (1): 59–79. July 2005. doi:10.1016/j.pharmthera.2005.01.005. PMID 15963351.
- ↑ DiFrancesco, Dario (19 February 2010). "The Role of the Funny Current in Pacemaker Activity". Circulation Research 106 (3): 434–446. doi:10.1161/CIRCRESAHA.109.208041. https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.109.208041. Retrieved 6 September 2023.
- ↑ "Direct activation of cardiac pacemaker channels by intracellular cyclic AMP". Nature 351 (6322): 145–7. May 1991. doi:10.1038/351145a0. PMID 1709448. Bibcode: 1991Natur.351..145D.
- ↑ "The G-protein-gated K+ channel, IKACh, is required for regulation of pacemaker activity and recovery of resting heart rate after sympathetic stimulation". The Journal of General Physiology 142 (2): 113–26. August 2013. doi:10.1085/jgp.201310996. PMID 23858001. PMC 3727310. https://dash.harvard.edu/bitstream/handle/1/11879733/3727310.pdf?sequence=1.
- ↑ "Dysfunctional HCN ion channels in neurological diseases" (in English). Frontiers in Cellular Neuroscience 6: 174. 2015. doi:10.3389/fncel.2015.00071. PMID 25805968.
- ↑ 8.0 8.1 "The pacemaker current: from basics to the clinics". Journal of Cardiovascular Electrophysiology 18 (3): 342–7. March 2007. doi:10.1111/j.1540-8167.2006.00736.x. PMID 17284289.
- ↑ "Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial". Lancet 372 (9641): 807–16. September 2008. doi:10.1016/S0140-6736(08)61170-8. PMID 18757088.
- ↑ "Familial sinus bradycardia associated with a mutation in the cardiac pacemaker channel". The New England Journal of Medicine 354 (2): 151–7. January 2006. doi:10.1056/NEJMoa052475. PMID 16407510.
 |