Chemistry:Suvorexant
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Belsomra |
| Other names | MK-4305; MK4305 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a614046 |
| License data |
|
| Pregnancy category |
|
| Dependence liability | Low |
| Addiction liability | Low |
| Routes of administration | By mouth[2] |
| Drug class | Orexin receptor antagonist; Hypnotic; Sedative |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 82% (10 mg; lower at higher doses)[2][5] |
| Protein binding | 99.5%[6][2] |
| Metabolism | Liver (CYP3A major, CYP2C19 minor)[2] |
| Metabolites | Hydroxysuvorexant (inactive)[2] |
| Elimination half-life | 12.2 hours (8–19 hours) (40 mg)[2][5][7] |
| Excretion | Feces: 66%[2] Urine: 23%[2] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C23H23ClN6O2 |
| Molar mass | 450.93 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Suvorexant, sold under the brand name Belsomra, is an orexin antagonist medication which is used in the treatment of insomnia.[2][6] It is indicated specifically for the treatment of insomnia characterized by difficulties with sleep onset and/or maintenance in adults.[2][6] Suvorexant helps with falling asleep faster, sleeping longer, being awake less in the middle of the night, and having better quality of sleep.[2][8] Its effectiveness is modest,[9] and is similar to that of other orexin antagonists, but is lower than that of benzodiazepines and Z-drugs.[10] Suvorexant is taken by mouth.[2][11][6]
Side effects of suvorexant include somnolence, daytime sleepiness and sedation, headache, dizziness, abnormal dreams, dry mouth, and impaired next-day driving ability.[2][8][12] Rarely, sleep paralysis, sleep-related hallucinations, complex sleep behaviors like sleepwalking, and suicidal ideation may occur.[2][6][9] Tolerance, dependence, withdrawal, and rebound effects do not appear to occur significantly with the medication.[2][13][14] Suvorexant is a dual orexin receptor antagonist (DORA).[6] It acts as a selective dual antagonist of the orexin OX1 and OX2 receptors.[6] The medication has an intermediate elimination half-life of 12 hours and a time to peak of about 2 to 3 hours.[2][6] Unlike benzodiazepines and Z-drugs, suvorexant does not interact with GABA receptors, instead having a distinct mechanism of action.[6][15]
Clinical development of suvorexant began in 2006[16] and it was introduced for medical use in 2014.[2][17] The medication is a schedule IV controlled substance in the United States and may have a modest potential for misuse.[18][2][19] In other places, such as Australia, suvorexant is a prescription-only medicine and is not a controlled drug.[1] Suvorexant is not available in generic formulations.[11][20][21] Besides suvorexant, other orexin receptor antagonists like lemborexant and daridorexant have also been introduced.[22][23]
Medical uses
Suvorexant is used for the treatment of insomnia, characterized by difficulties with sleep onset and/or sleep maintenance, in adults.[2][6] At a dose of 15 to 20 mg and in terms of treatment–placebo difference, it reduces time to sleep onset by up to 10 minutes, reduces time awake after sleep onset by about 15 to 30 minutes, and increases total sleep time by about 10 to 20 minutes.[2] A 2017 systematic review and meta-analysis of randomized controlled trials of suvorexant for insomnia likewise found that the medication improved subjective sleep onset, subjective total sleep time, and subjective sleep quality when assessed at one to three months of treatment.[8] The effectiveness of approved doses of suvorexant (≤20 mg) in the treatment of insomnia is said to be modest.[9][24][13][25]
Network meta-analyses have assessed the sleep-promoting effects of suvorexant and have compared them to those of other orexin receptor antagonists like lemborexant and daridorexant as well as to other sleep aids including benzodiazepines, Z-drugs, antihistamines, sedative antidepressants (e.g., trazodone, doxepin, amitriptyline, mirtazapine), and melatonin receptor agonists.[10][26][27][28] A major systematic review and network meta-analysis of insomnia medications published in 2022 found that suvorexant had an effect size (standardized mean difference (SMD)) against placebo for treatment of insomnia at 4 weeks of 0.31 (95% CI 0.01 to 0.62).[10] Suvorexant appeared to be similarly effective at 4 weeks to lemborexant (SMD 0.36, 95% CI 0.08 to 0.63) and daridorexant (SMD 0.23, 95% CI –0.01 to 0.48), whereas benzodiazepines and Z-drugs generally showed larger effect sizes (e.g., SMDs of 0.45 to 0.83) and antihistamines (e.g., doxepin, doxylamine, trimipramine) showed more similar efficacy (SMDs of 0.30 to 0.55).[10]
Orexin receptor antagonists like suvorexant increase total sleep time predominantly by increasing rapid eye movement sleep (REM) sleep, whereas they have no effect on or even decrease non-rapid eye movement (NREM) sleep.[29] This is in contrast to most other hypnotics, which either do not affect REM sleep or decrease it.[22] The implications of these differences are not fully clear.[22] Unlike certain other hypnotics like benzodiazepines and Z-drugs, orexin receptor antagonists do not disrupt sleep architecture, and this might provide more restful sleep.[30][31][32][33]
It is unclear if suvorexant is safe among people with a history of substance addiction or alcoholism, as these individuals were excluded from clinical trials of suvorexant.[34] A Cochrane review found suvorexant to be effective in the short-term treatment of sleep disturbances in people with dementia with few adverse effects.[35] It is unknown if suvorexant is effective and safe for treatment of sleep problems in children and adolescents as suvorexant has not been studied in this context.[2]
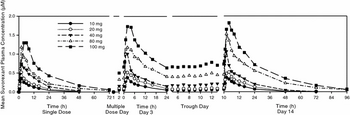
Suvorexant is approved for the treatment of insomnia by the United States Food and Drug Administration (FDA) at doses of 5 to 20 mg and by the Australian Therapeutic Goods Administration (TGA) and Japanese Pharmaceuticals and Medical Devices Agency (PMDA) at doses of 15 mg (in the elderly) and 20 mg (in younger adults).[2][6][1][8] In the United States, the recommended starting dose is 10 mg and the maximum recommended dose is 20 mg.[2][6] Higher doses of 30 and 40 mg were also submitted to regulatory agencies for approval but were not authorized due to lack of clearly superior efficacy to doses of 15 to 20 mg and concerns about next-day effects and associated impairment (e.g., driving).[6][34] In addition to the preceding doses, suvorexant has been assessed at higher doses of up to 100 mg in clinical trials.[6][34][36] These higher doses appeared to be more effective at promoting sleep than lower doses but produced greater next-day effects.[6][34][9][36] Lower approved doses of suvorexant in the United States in the range of 5 to 10 mg were not extensively evaluated in clinical trials.[24][25]
The American Academy of Sleep Medicine's 2017 clinical practice guidelines recommend the use of suvorexant in the treatment of sleep-onset and sleep-maintenance insomnia along with various other sleep medications.[37] Orexin receptor antagonists are not used as first-line treatments for insomnia due to their costs and concerns about possible misuse liability.[26] Generic formulations of orexin receptor antagonists including suvorexant are not yet available.[11][20][21]
Available forms
Suvorexant is available in the form of 5, 10, 15, and 20 mg oral film-coated tablets.[2][11][19] It is provided as 10- and 30-tablet blister packs as well as 3-tablet starter packs.[2][1] The availability of these different packs varies by country (all three available in Australia but only 30-tablet packs available in the United States).[2][1]
Contraindications
Suvorexant is contraindicated in people with narcolepsy as it may worsen their symptoms.[2][9] This is its only absolute contraindication.[2] Suvorexant has not been studied in people with severe hepatic impairment and is not recommended in these individuals due to the likelihood of increased suvorexant exposure.[2] On the other hand, suvorexant may be used in people with mild-to-moderate hepatic impairment as well as renal impairment of any severity and no dose adjustment is necessary in these situations.[2] Concomitant use of suvorexant with strong CYP3A4 inhibitors is not recommended due to potential for increased suvorexant exposure while concomitant use of suvorexant with strong CYP3A4 inducers may result in loss of suvorexant exposure and effectiveness.[2] Suvorexant should be used carefully in people with a history of drug misuse or alcoholism due to its drug-liking effects and possible misuse potential at doses higher than those approved for therapeutic use.[2][38] Similarly, suvorexant should be used carefully in people with a history of depression or suicidality as it may rarely increase suicidal ideation.[2][6][9] The medication is indicated for use in adults and the elderly but has not been studied in children and adolescents and hence is not recommended for these individuals.[2]
Suvorexant has shown teratogenic effects in animals such as decreased body weight at doses much higher than the equivalents of those approved for therapeutic use in humans.[2][39] Teratogenic effects with therapeutic doses of suvorexant in humans have not been established due to lack of research and available data.[2][39] Suvorexant is pregnancy category C in the United States.[39] It is unknown whether suvorexant is present in the breast milk, whether it affects lactation in breastfeeding women, or whether it affects breastfed infants.[2] However, suvorexant has been found to be present in mammary milk in rats and this is likely to be the case in humans as well.[2][39] Suvorexant should be used in pregnant and breastfeeding women only if the potential benefit justifies the potential for harm to the baby.[2][39]
Side effects
Side effects of suvorexant (at doses of 15–20 mg) include somnolence (7% vs. 3% for placebo) and headaches (7% vs. 6% for placebo).[2] Somnolence with suvorexant appears to be dose-dependent, with rates of 2% at 10 mg, 5% at 20 mg, 10–12% at 40 mg, and 11–12% at 80 mg, relative to 0.4% for placebo.[2][6] Less common side effects (at 15–20 mg) may include dizziness (3% vs. 2% for placebo), abnormal dreams (2% vs. 1% for placebo), diarrhea (2% vs. 1% for placebo), dry mouth (2% vs. 1% for placebo), upper respiratory tract infection (2% vs. 1% for placebo), and cough (2% vs. 1% for placebo).[2] High doses of suvorexant (80 mg) have also been found to produce greater incidence of dizziness (5% vs. 0% for placebo) and abnormal dreams (5% vs. 1% for placebo).[6]
Less commonly, suvorexant may cause sleep paralysis, hypnagogic and hypnopompic hallucinations, and complex sleep behaviors (0.2–0.6% vs. 0% for placebo).[2][9] Complex sleep behaviors include sleepwalking, sleep-driving, and engaging in other activities while not completely awake (e.g., making or eating food, making phone calls, and having sex).[2] Other narcoleptic-like symptoms such as cataplexy (sudden weakness or paralysis) may also rarely occur.[24][9] Suvorexant may sometimes cause worsening of depression or suicidal ideation.[2][6] A dose-dependent increase in suicidal ideation as assessed with the Columbia Suicide Severity Rating Scale was seen with suvorexant in clinical trials although rates were very low (0.2% (1/493) at low doses (15–20 mg) and 0.4% (5/1291) at high doses (30–40 mg) relative to 0.1% (1/1025) for placebo).[2][6] It has also been stated however that suicidal ideation was reported in 0% to 1.6% of people taking 10 to 20 mg and 3.4% to 8.2% taking 40 to 80 mg relative to 0% to 0.3% with placebo.[9] Suicidal ideation with suvorexant is considered to be mild.[6][9] In any case, caution is warranted in use of suvorexant in people with depression, and people with worsening depression or suicidal thoughts should be promptly evaluated.[9][2] Besides the clinical trial data, a case report of rapidly worsened depression and onset of suicidal ideation with suvorexant has been published.[40][41]
The next-day effects of suvorexant have been studied.[2] Besides the side effect of daytime somnolence, suvorexant may dose-dependently reduce alertness and motor coordination and impair driving ability.[2][8] It may also increase the risk of falling asleep while driving.[2] Driving ability was found to be impaired at doses of 20 and 40 mg in clinical studies.[2] Driving impairment may also occur with lower doses of suvorexant due to variations in individual sensitivity to the medication.[2] In three of four studies, 30 mg suvorexant had no influence on next-day memory or balance, whereas in the remaining study, there was a decrease in morning word recall with 40 mg and an increase in body sway with 20 and 40 mg doses.[2] In another study in elderly people who were awakened in the night, impaired balance was present at 1.5 hours after taking 30 mg suvorexant whereas memory was unaffected.[2]
A 2017 systematic review and meta-analysis of suvorexant for the treatment of insomnia found that the medication significantly increased the rate of somnolence by 3.5-fold, daytime sleepiness/sedation by 3.1-fold, fatigue by 2.1-fold, abnormal dreams by 2.1-fold, and dry mouth by 2.0-fold.[8][30] Conversely, suvorexant did not significantly differ from placebo in the rates of any other assessed adverse effects.[8][30] This included back pain, diarrhea, dizziness, falls, headache, car accidents/traffic violations, nasopharyngitis, nausea, potential drug misuse, suicidal ideation, complex sleep behaviors, hypnagogic or hypnopompic hallucinations, and sleep paralysis.[8] The overall risk of any adverse event was increased 1.07-fold while discontinuation due to adverse events was unchanged (RR = 0.93, 95% CI 0.60 to 1.44).[8]
Tolerance, dependence, withdrawal, and rebound effects do not appear to occur with suvorexant in the treatment of insomnia at studied doses.[2][13][14] In three-month clinical studies, no rebound insomnia as assessed by measures of sleep onset or maintenance was observed with discontinuation of suvorexant at doses of 15 to 40 mg.[2] Similarly, no withdrawal effects were observed with discontinuation of suvorexant at these doses.[2] However, in other reports, some tolerance as assessed by diminishing somnolence and rebound insomnia upon discontinuation has been noted.[42][12][13]
The orexin neuropeptides augment the signaling of the mesolimbic dopamine reward pathway and are thought to potentiate hedonic tone.[43][44][22][45] Conversely, low orexin signaling may result in low hedonic tone and orexin receptor antagonists are of interest for the potential treatment of addiction.[43][44][22][45] In line with these findings, suvorexant and other orexin receptor antagonists have not shown misuse liability in animal studies in rats and non-human primates.[19][46][47][48] Paradoxically however, orexin receptor antagonists, including suvorexant, lemborexant, and daridorexant, have consistently shown drug-liking responses in human studies of recreational sedative users.[2][49][50][38] Suvorexant at higher-than-approved doses (40, 80, and 150 mg vs. 20 mg maximum recommended dose) showed similar drug liking to the Z-drug zolpidem (15 and 30 mg) in such individuals.[2][34][19][38][51] On the other hand, it showed lower misuse potential on all other measures (including an overall rate of misuse potential adverse event of 58% for zolpidem and 31% for suvorexant).[34][19] In another study, suvorexant at a dose of 150 mg showed greater drug liking than daridorexant (50 mg) but similar drug liking to zolpidem (30 mg) and higher doses of daridorexant (100–150 mg) in recreational sedative users.[49][38] There was no apparent dose–response relationship for positive measures of misuse potential with suvorexant, in contrast to zolpidem.[19][51] In the phase III clinical trials, misuse potential adverse events were reported in 3.0% with placebo, 4.1% with 15 or 20 mg suvorexant, and 2.6% with 30 or 40 mg suvorexant.[19] The misuse liability of suvorexant is considered to be at most modest, and further research is needed to characterize the misuse potential of orexin receptor antagonists.[2][19][46] In any case, suvorexant is a controlled substance in the United States due to concerns about the possibility of misuse.[2][6][19]
Besides its subjective side effects, suvorexant has been found to cause dose-dependent increases in serum cholesterol levels in clinical trials.[2][25] These changes in cholesterol levels were +1.2 mg/dL at 10 mg, +2.3 mg/dL at 20 mg, +3.1 mg/dL at 40 mg, and +6.0 mg/dL at 80 mg relative to –3.7 mg/dL for placebo.[2][25] Although the increases in cholesterol levels with approved doses of suvorexant (10–20 mg) are small, they could be important over a long duration of treatment.[25]
Early studies in rodents found that orexins (derived from Greek "orexis" meaning "appetite") stimulate appetite, feeding behavior, and weight gain while orexin receptor antagonists block these effects.[52][53][6] However, subsequent animal studies were more mixed, with the effects being limited and depending on the animal strain.[52][53][6] In humans, orexin receptor antagonists including suvorexant have not been found to affect body weight in rigorous clinical trials that lasted up to 12 to 14 months.[53][6]
Overdose
There is limited experience with overdose of suvorexant.[2] Suvorexant has been assessed in single doses of as high as 240 mg in clinical studies.[2][7][6][19] The medication dose-dependently produces somnolence.[2] High doses of suvorexant may also cause sleep-onset paralysis in some individuals (2% incidence at doses of 40–240 mg).[6] Treatment of suvorexant overdose is based on symptoms and is supportive.[2] Gastric lavage may be used where appropriate whereas the value of dialysis has not been determined.[2] Because suvorexant has high plasma protein binding, hemodialysis is not expected to enhance elimination of suvorexant.[2]
Interactions
CYP3A4 inhibitors can increase exposure to suvorexant while CYP3A4 inducers can decrease exposure to suvorexant.[2][14][54] Combination of suvorexant with the strong CYP3A4 inhibitor ketoconazole increased suvorexant overall exposure by 2.79-fold and peak levels by about 1.25-fold, combination with the moderate CYP3A4 inhibitor diltiazem increased suvorexant overall exposure by 2.05-fold and peak levels by about 1.25-fold, and combination with the strong CYP3A4 inducer rifampin decreased suvorexant overall exposure by 88% and peak levels by about 65%.[2][5][54] The elimination half-life of suvorexant (about 12 hours for suvorexant alone) was increased to 19.4 hours with ketoconazole and to 16.1 hours with diltiazem while it was decreased to 7.7 hours with rifampin.[55][54] Concomitant use of suvorexant with strong CYP3A4 inhibitors is not recommended, while lower doses of suvorexant are recommended with moderate CYP3A4 inhibitors (5 mg starting dose and 10 mg maximum dose generally).[2] The substantial decrease in suvorexant exposure with strong CYP3A4 inducers may result in loss of effectiveness.[2] Suvorexant does not appear to have been assessed in combination with moderate CYP3A4 inducers (e.g., modafinil).[2][5][54]
Examples of important CYP3A4 modulators which are expected to interact with suvorexant include the strong CYP3A4 inhibitors boceprevir, clarithromycin, conivaptan, indinavir, itraconazole, ketoconazole, lopinavir, nefazodone, nelfinavir, posaconazole, ritonavir, saquinavir, telaprevir, and telithromycin (concomitant use not recommended); the moderate CYP3A4 inhibitors amprenavir, aprepitant, atazanavir, ciprofloxacin, diltiazem, dronedarone, erythromycin, fluconazole, fluvoxamine, fosamprenavir, grapefruit juice, imatinib, and verapamil (lower doses of suvorexant recommended); and the strong CYP3A4 inducers apalutamide, carbamazepine, efavirenz, enzalutamide, phenytoin, rifampin, and St. John's wort (expected to decrease suvorexant effectiveness).[2][56][14]
Coadministration of suvorexant with other CNS depressants such as alcohol, benzodiazepines, opioids, and tricyclic antidepressants may increase the risk of CNS depression and daytime impairment.[2] Alcohol and suvorexant do not appear to interact in terms of pharmacokinetics but consumption of alcohol in combination with suvorexant is not advised due to additive CNS depression.[2] Dosage adjustment may be necessary when suvorexant is combined with other CNS depressants.[2] Use of suvorexant in combination with other medications used in the treatment of insomnia is not recommended.[2]
Suvorexant is not expected to cause clinically meaningful inhibition or induction of various cytochrome P450 enzymes and drug transporters.[2] It has been found to not substantially influence the pharmacokinetics of midazolam (CYP3A4 substrate), warfarin (CYP2C9 substrate), digoxin (P-glycoprotein substrate), or combined birth control pills.[2] However, coadministration of suvorexant with digoxin may result in slightly increased digoxin exposure due to inhibition of intestinal P-glycoprotein by suvorexant.[2] Concentrations of digoxin should be monitored during coadministration of suvorexant and digoxin.[2]
Pharmacology
Pharmacodynamics
Suvorexant acts as a selective dual antagonist of the orexin (hypocretin) receptors OX1 and OX2.[14][57] These receptors are the biological targets of the endogenous wakefulness-promoting orexin neuropeptides orexin-A and orexin-B.[22] The binding affinities (Ki) of suvorexant at the human orexin receptors are 0.55 nM for the OX1 receptor and 0.35 nM for the OX2 receptor.[57][2][5] The antagonistic potencies or functional inhibition (Kb) of suvorexant at the human orexin receptors are 65 nM for the OX1 receptor and 41 nM for the OX2 receptor.[57] Hence, suvorexant shows similar affinities and antagonistic activities at the OX1 and OX2 receptors in vitro.[14][57] Suvorexant is highly selective for the orexin receptors over a large number of other targets (170 screened off-target receptors, enzymes, and transporters).[6][58] In contrast to certain other sedatives and hypnotics, suvorexant is not a benzodiazepine or Z-drug and does not interact with GABA receptors.[6][15][5]
Mechanism of action
Suvorexant is thought to exert its therapeutic effects in the treatment of insomnia by blocking the orexin receptors and thereby inhibiting the effects of the endogenous wakefulness-promoting orexin neuropeptides orexin-A and orexin-B.[2][57] The orexin neuropeptides are produced exclusively by a relatively small population of 20,000 to 80,000 neurons located in the lateral hypothalamus in the brain.[59][60] These neurons project widely throughout the brain and mediate excitatory signaling to key centers involved in sleep–wake regulation, including the noradrenergic locus coeruleus, histaminergic tuberomammillary nucleus, serotonergic raphe nucleus, and dopaminergic ventral tegmental area.[59][61][62][60][63] The orexin system shows circadian rhythmicity in its activity, with high activity during waking and low to no activity during sleep or at night.[59][5][64] Orexin system activity during wakefulness is also higher with behavioral activation and with high-intensity emotions.[65][59]
Narcolepsy is a chronic sleep disorder characterized by excessive daytime sleepiness, cataplexy, sleep paralysis, and hypnagogic hallucinations, as well as sleep attacks and fragmented sleep.[66][62] Narcolepsy with cataplexy, also known as type 1 narcolepsy, is thought to be caused by loss of orexin-producing neurons in the lateral hypothalamus, possibly mediated by autoimmune mechanisms related to environmental triggers in genetically susceptible individuals.[66][65] There is an 80 to 100% loss of orexin-producing neurons in the lateral hypothalamus and very low or undetectable levels of orexin-A in cerebrospinal fluid in people with narcolepsy.[61][66][65] Similarly, narcolepsy with cataplexy in dogs is caused by a mutation in the gene encoding the OX2 receptor, and knockout mice for genes encoding orexin system proteins such as prepro-orexin or the OX2 receptor show a narcolepsy-like phenotype.[61][66] Although there is hypersomnolence in narcolepsy, people with the condition do not sleep more overall than normal individuals but instead experience more sleepiness and sleep during daytime in tandem with disturbed sleep at night.[62][24] They do not usually feel well-rested during the day.[24] Besides narcolepsy, the orexin system may also be involved in the etiology of insomnia.[67][59] In addition, orexin signaling appears to change with age, and this may be involved in age-related sleep disturbances.[67][68]
Orexin receptor antagonists may be expected to produce effects similar to those in narcolepsy.[24][52][59] However, the effects of acute transient pharmacological antagonism of the orexin receptors are not necessarily the same as in the chronic and severe orexin deficiency in narcolepsy.[57][52][59][69] Modulation of orexin signaling with orexin receptor antagonists produces effects that occur more at night when drug levels are high and less during the day when levels are low.[24][59] In addition, long-term neural changes may develop in narcolepsy to compensate for the orexin deficiency in the condition.[57][52][59][69] In animals and humans, orexin receptor agonists such as orexin-A and danavorexton dose-dependently produce wakefulness and locomotor activity[62][22][64] while orexin receptor antagonists like suvorexant transiently reduce locomotor activity and dose-dependently promote sleep.[30][31] Acute orexin receptor antagonists can promote sleep in animals to a greater extent than what occurs in narcolepsy-like orexin system loss.[52] In addition, little to no cataplexy has been observed even with high doses of orexin receptor antagonists in animals and humans.[57][52][59][70] It is unknown if long-term use of orexin receptor antagonists may produce compensatory neural changes or narcolepsy-like symptoms.[57] An animal study of chronic high-dose suvorexant administration that showed development of narcolepsy-like changes suggests that this may be possible however.[71]
Endogenous orexinergic tone is expected to play an important moderating influence in terms of the effects of orexin receptor modulators.[5] As an example, rising orexin levels during the day may help to competitively offset the next-day residual effects of nightly-dosed orexin receptor antagonists.[5]
Pharmacokinetics
Absorption
The absolute bioavailability of suvorexant is 82% at a dose of 10 mg.[2] Suvorexant exposure does not increase dose-proportionally over a dose range of 10 to 100 mg, which is likely due to decreased absorption at higher doses.[2][5][72] Exposure to suvorexant increases by about 75% with a doubling of dose from 20 mg to 40 mg.[5] The time to peak levels of suvorexant is 2 to 3 hours regardless of dose but with wide variation (range 30 minutes to 8 hours).[2][6] Taking suvorexant with food does not modify suvorexant peak levels or area-under-the-curve levels (overall exposure) but does delay the time to peak concentrations by about 1.5 hours.[2] Steady-state levels of suvorexant with once-daily continuous administration are reached within 3 days.[2][5] Levels of suvorexant accumulate minimally, by about 1.2- to 1.6-fold, with repeated once-daily administration.[5][2]
Distribution
The volume of distribution of suvorexant is approximately 49 L.[2] It crosses the blood–brain barrier and distributes into the central nervous system.[57]
Suvorexant has high plasma protein binding (99.5%).[6][2] It is bound to albumin and α1-acid glycoprotein (orosomucoid).[2]
Metabolism
Suvorexant is metabolized primarily by hydroxylation via CYP3A enzymes.[2][7] CYP2C19 also contributes to suvorexant metabolism to a minor extent.[2] The major circulating forms are suvorexant and its metabolite hydroxysuvorexant.[2] The hydroxysuvorexant (M9) metabolite is not expected to be pharmacologically active.[2][7] It showed 10-fold lower affinity for the orexin receptors than suvorexant in vitro, was a substrate for P-glycoprotein making it unlikely to cross the blood–brain barrier, and did not show sedative effects in animal studies.[7] Suvorexant also has several other minor metabolites.[7]
Elimination
Suvorexant is eliminated mainly via metabolism.[2] It is excreted primarily in feces (66%) predominantly as metabolites and to a lesser extent in urine (23%).[2][5]
The elimination half-life of suvorexant at a dose of 40 mg is 12.2 hours, with a range of 8 to 19 hours.[2][5][7][6] In another study, the half-life of suvorexant was 15 hours with a range of 10 to 22 hours.[2] In one study, the half-lives of suvorexant (mean ± SD) were 9.0 ± 7.2 hours at 10 mg, 10.8 ± 3.6 hours at 50 mg, and 13.1 ± 5.8 hours at 100 mg.[6] With doses of 120 to 240 mg, the half-lives of suvorexant were 12.1 to 14.5 hours in healthy young males and 14.4 to 15.8 hours in healthy young females.[7] The half-life of suvorexant's inactive metabolite hydroxysuvorexant is similar to that of suvorexant.[7]
Specific populations
Age and race do not influence the pharmacokinetics of suvorexant in a clinically meaningfully way.[2] Exposure to suvorexant is slightly higher in women compared to men (Cmax 9% higher, AUC 17% higher), however dose adjustments based on gender are generally unnecessary.[2] Suvorexant exposure is greater in people with higher body mass index, such as obese people (Cmax 17% higher, AUC 31% higher).[2] This is particularly the case in obese women relative to non-obese women (Cmax 25% higher, AUC 46% higher).[2] Suvorexant exposure with a single dose is not greater in people with moderate hepatic insufficiency compared to healthy individuals.[2] However, the half-life of suvorexant at a dose of 20 mg was prolonged from 14.7 hours (range 10–22 hours) to 19.1 hours (range 11–49 hours) in these individuals.[2][7] Suvorexant exposure is unchanged in people with severe renal impairment and no dosage adjustment is necessary in these individuals.[2] Similarly to hepatic impairment, the half-life of suvorexant was increased to 19.4 hours when used in combination with the strong CYP3A4 inhibitor ketoconazole and to 16.1 hours with the moderate CYP3A4 inhibitor diltiazem while it was decreased to 7.7 hours with the strong CYP3A4 inducer rifampin.[55][54]
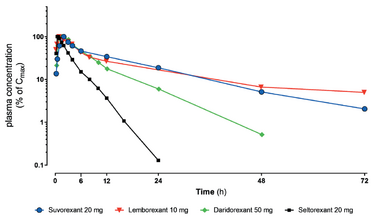
Miscellaneous

The delayed time to peak levels (2–3 hours) and long elimination half-life (12 hours) of suvorexant are less than ideal for an insomnia medication as they result in a delayed onset of effect and significant next-day side effects such as daytime sedation.[6][9] Orexin receptor antagonists with shorter half-lives and faster onsets of action are theoretically more optimal for therapeutic use as sleep aids.[6][14] The ideal insomnia medication would not have a duration of action extending beyond about 8 hours.[53] Relative to suvorexant, daridorexant has a shorter half-life (8 hours) while lemborexant has a longer half-life (17–55 hours).[14] However, although lemborexant has a longer terminal elimination half-life than suvorexant, it appears to be more rapidly cleared in the earlier phases of elimination.[73][14] The investigational agents seltorexant and vornorexant, which are still in clinical trials, have comparatively very short half-lives in the range of 1.5 to 3 hours.[14][74]
Suvorexant dissociates from the orexin receptors slowly.[6][57] As a result, its duration may be longer than that suggested by its circulating concentrations and half-life.[6][57]
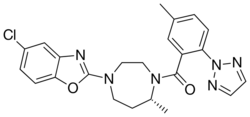
Chemistry
Suvorexant is a small-molecule compound.[75] The chemical name of suvorexant is [(7R)-4-(5-chloro-2-benzoxazolyl)hexahydro-7-methyl-1H-1,4-diazepin-1-yl][5-methyl-2-(2H-1,2,3-triazol-2-yl)phenyl]methanone.[2] Its molecular formula is C23H23N6O2Cl and its molecular weight is 450.92 g/mol.[2] Suvorexant is a white to off-white powder and is lipophilic and insoluble in water.[2][14] It is structurally related to other orexin receptor antagonists like lemborexant, daridorexant, and seltorexant.[14][75]
History
The orexin neuropeptides were discovered in 1998[22][16] and the role of the orexin system in the etiology of narcolepsy was identified between 1999 and 2000.[70] Subsequent research further established the role of the orexin system in sleep–wake regulation.[22][16][64] Due to the promising potential of orexin system modulation in the treatment of sleep disorders, these findings led to translational efforts to bring orexin receptor modulators to medicine as therapeutic agents.[22][16][64][70][69]
Suvorexant was developed by Merck.[22][16] It entered clinical development in 2006[16] and was first described in the medical literature in 2010.[76] The medication was approved by the FDA for the treatment of insomnia in the United States on 13 August 2014.[2][11][77] Suvorexant was initially released November 2014 in Japan ,[17] then later reached the United States in February 2015,[78] Australia in November 2016, and Canada in November 2018.[79] It was the first orexin receptor antagonist to be introduced for medical use, and was followed by lemborexant in 2019 and daridorexant in 2022.[57][14][23] Development of almorexant (ACT-078573) and filorexant (MK-6096) was discontinued, while seltorexant (MIN-202, JNJ-42847922) and vornorexant (ORN-0829, TS-142) are still in clinical trials.[14][22]
Suvorexant marketing exclusivity in the United States was set to expire in January 2023 and patent protection is set to expire in 2029 to 2033.[11]
Society and culture
Names
Suvorexant is the generic name of the drug and its INN, USAN, and JAN.[80][81] The medication was developed by Merck under the code name MK-4305 and is marketed under the brand name Belsomra.[34]
Availability
Suvorexant has been marketed in the United States, Canada, Australia, Russia, and Japan.[82][78][79][17] Although previously available, suvorexant appears to have been discontinued in Canada.[83][82] It does not appear to be available in the United Kingdom or other European countries besides Russia.[84][85][82]
Legal status
Suvorexant is a schedule IV controlled substance under the Controlled Substances Act in the United States.[18][86][87] It is not a controlled drug in Australia, instead being classed as a prescription-only medicine (Schedule 4 (S4)) in this country.[1]
Controversy
Public Citizen, a progressive consumer rights advocacy group, issued a letter in June 2013 urging the FDA not to approve suvorexant.[25] In its reasoning, it cited marginal benefits and excessive potential for harm, including next-day effects like driving impairment and possible accidents.[25] Consumer Reports also published articles encouraging consumers to avoid suvorexant due to it being expensive, having limited effectiveness, and posing safety concerns.[88][89]
Research
Delirium
Suvorexant is under development for the treatment of delirium.[90] As of October 2021, it is in phase III clinical trials for this indication.[90]
Psychiatry
Suvorexant has been studied in the treatment of insomnia in people with psychiatric disorders such as depression and anxiety.[30][91][92] It was reported to improve psychiatric symptoms and to decrease cortisol levels in these individuals.[91][30] A phase IV clinical trial of suvorexant as an adjunct to antidepressant therapy in people with major depressive disorder and residual insomnia was underway as of 2019.[30][93] Although orexin receptor antagonists including suvorexant could be useful for treatment of depression and anxiety, there is also indication that they could have harmful effects in these conditions (e.g., animal studies and suicidal ideation in clinical trials).[40][46][59] More clinical research is needed to determine the place of orexin receptor antagonists in the treatment of people with depression and anxiety.[40]
There is interest in suvorexant and other orexin receptor antagonists in the potential treatment of substance use disorders,[94][95][44][46][53][22][92] including alcohol use disorder,[96][97][98] cocaine use disorder,[58] and opioid use disorder.[99]
Alzheimer's disease
Suvorexant and other orexin receptor modulators are of interest for possible use in the prevention of Alzheimer's disease.[92][100]
Diabetes
Suvorexant has been studied in people with type 2 diabetes and insomnia and has been reported to improve sleep and metabolic parameters in these individuals.[101][102] The improvement in metabolic parameters appeared to be related to improved sleep.[101][102]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 "Belsomra (suvorexant)". Australian Product Information. https://www.guildlink.com.au/gc/ws/msd/pi.cfm?product=mkpbelso.
- ↑ 2.000 2.001 2.002 2.003 2.004 2.005 2.006 2.007 2.008 2.009 2.010 2.011 2.012 2.013 2.014 2.015 2.016 2.017 2.018 2.019 2.020 2.021 2.022 2.023 2.024 2.025 2.026 2.027 2.028 2.029 2.030 2.031 2.032 2.033 2.034 2.035 2.036 2.037 2.038 2.039 2.040 2.041 2.042 2.043 2.044 2.045 2.046 2.047 2.048 2.049 2.050 2.051 2.052 2.053 2.054 2.055 2.056 2.057 2.058 2.059 2.060 2.061 2.062 2.063 2.064 2.065 2.066 2.067 2.068 2.069 2.070 2.071 2.072 2.073 2.074 2.075 2.076 2.077 2.078 2.079 2.080 2.081 2.082 2.083 2.084 2.085 2.086 2.087 2.088 2.089 2.090 2.091 2.092 2.093 2.094 2.095 2.096 2.097 2.098 2.099 2.100 2.101 2.102 2.103 2.104 2.105 2.106 2.107 2.108 2.109 2.110 2.111 2.112 2.113 "Belsomra- suvorexant tablet, film coated". https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=e5b72731-1acb-45b7-9c13-290ad12d3951.
- ↑ "Prescription medicines: registration of new chemical entities in Australia, 2016". 21 June 2022. https://www.tga.gov.au/prescription-medicines-registration-new-chemical-entities-australia-2016.
- ↑ "Search Page - Drug and Health Product Register". 23 October 2014. https://hpr-rps.hres.ca/reg-content/regulatory-decision-summary-detail.php?lang=en&linkID=RDS00475.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 Merck Sharp and Dohme Corporation (22 May 2013). "Suvorexant Advisory Committee Meeting Briefing Document: Peripheral & Central Nervous System Drugs Advisory Committee Meeting". https://www.fda.gov/downloads/advisorycommittees/committeesmeetingmaterials/drugs/peripheralandcentralnervoussystemdrugsadvisorycommittee/ucm352970.pdf.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 6.17 6.18 6.19 6.20 6.21 6.22 6.23 6.24 6.25 6.26 6.27 6.28 6.29 6.30 6.31 6.32 6.33 6.34 6.35 6.36 6.37 6.38 "Suvorexant for the treatment of insomnia". Expert Review of Clinical Pharmacology 7 (6): 711–730. November 2014. doi:10.1586/17512433.2014.966813. PMID 25318834.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 7.9 "Application Number: 204569Orig1s000. Clinical Pharmacology/Biopharmaceutics Review. Suvorexant (MK-4305).". Center for Drug Evaluation and Research (Food and Drug Administration). 2014. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/204569Orig1s000ClinPharmR.pdf.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 "Suvorexant for the treatment of primary insomnia: A systematic review and meta-analysis". Sleep Medicine Reviews 35: 1–7. October 2017. doi:10.1016/j.smrv.2016.09.004. PMID 28365447.
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 "Profile of suvorexant in the management of insomnia". Drug Design, Development and Therapy 9: 6035–6042. 2015. doi:10.2147/DDDT.S73224. PMID 26648692.
- ↑ 10.0 10.1 10.2 10.3 "Comparative effects of pharmacological interventions for the acute and long-term management of insomnia disorder in adults: a systematic review and network meta-analysis". Lancet 400 (10347): 170–184. July 2022. doi:10.1016/S0140-6736(22)00878-9. PMID 35843245.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 "Belsomra Generic Belsomra Availability". Drugs.com. https://www.drugs.com/availability/generic-belsomra.html.
- ↑ 12.0 12.1 "Suvorexant for Primary Insomnia: A Systematic Review and Meta-Analysis of Randomized Placebo-Controlled Trials". PLOS ONE 10 (8): e0136910. 2015. doi:10.1371/journal.pone.0136910. PMID 26317363. Bibcode: 2015PLoSO..1036910K.
- ↑ 13.0 13.1 13.2 13.3 "Suvorexant: scientifically interesting, utility uncertain". Australasian Psychiatry 25 (6): 622–624. December 2017. doi:10.1177/1039856217734677. PMID 28994603.
- ↑ 14.00 14.01 14.02 14.03 14.04 14.05 14.06 14.07 14.08 14.09 14.10 14.11 14.12 14.13 14.14 14.15 "Clinical pharmacology, efficacy, and safety of orexin receptor antagonists for the treatment of insomnia disorders". Expert Opinion on Drug Metabolism & Toxicology 16 (11): 1063–1078. November 2020. doi:10.1080/17425255.2020.1817380. PMID 32901578.
- ↑ 15.0 15.1 "Drugs for Insomnia beyond Benzodiazepines: Pharmacology, Clinical Applications, and Discovery". Pharmacological Reviews 70 (2): 197–245. April 2018. doi:10.1124/pr.117.014381. PMID 29487083.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 "CNS drug development: lessons from the development of ondansetron, aprepitant, ramelteon, varenicline, lorcaserin, and suvorexant. Part I". Journal of Psychiatric Practice 20 (6): 460–465. November 2014. doi:10.1097/01.pra.0000456594.66363.6f. PMID 25406050.
- ↑ 17.0 17.1 17.2 "New hypnotic drug without addiction to be released in Japan first". http://en.apdnews.com/news/7ff7b8a890574d1cbb50675732d6873a.html.
- ↑ 18.0 18.1 "Schedules of Controlled Substances: Placement of Suvorexant into Schedule IV". Federal Register. 13 February 2014. https://www.federalregister.gov/articles/2014/02/13/2014-03124/schedules-of-controlled-substances-placement-of-suvorexant-into-schedule-iv. "A Proposed Rule by the Drug Enforcement Administration on 02/13/2014"
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 19.7 19.8 19.9 "Suvorexant for insomnia: a systematic review of the efficacy and safety profile for this newly approved hypnotic - what is the number needed to treat, number needed to harm and likelihood to be helped or harmed?". International Journal of Clinical Practice 68 (12): 1429–1441. December 2014. doi:10.1111/ijcp.12568. PMID 25231363.
- ↑ 20.0 20.1 "An Update on Dual Orexin Receptor Antagonists and Their Potential Role in Insomnia Therapeutics". Journal of Clinical Sleep Medicine 14 (8): 1399–1408. August 2018. doi:10.5664/jcsm.7282. PMID 30092886.
- ↑ 21.0 21.1 "Suvorexant: a promising, novel treatment for insomnia". Neuropsychiatric Disease and Treatment 12: 491–495. 2016. doi:10.2147/NDT.S31495. PMID 26955275.
- ↑ 22.00 22.01 22.02 22.03 22.04 22.05 22.06 22.07 22.08 22.09 22.10 22.11 22.12 "Hypocretins (orexins): The ultimate translational neuropeptides". Journal of Internal Medicine 291 (5): 533–556. May 2022. doi:10.1111/joim.13406. PMID 35043499.
- ↑ 23.0 23.1 "Daridorexant: First Approval". Drugs 82 (5): 601–607. April 2022. doi:10.1007/s40265-022-01699-y. PMID 35298826.
- ↑ 24.0 24.1 24.2 24.3 24.4 24.5 24.6 "Is suvorexant a better choice than alternative hypnotics?". F1000Research 4: 456. 2015. doi:10.12688/f1000research.6845.1. PMID 26594338.
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 25.6 "Letter to the FDA Opposing Approval of the Sleep Medicine Suvorexant". Public Citizen Inc.. 14 June 2013. https://www.citizen.org/article/letter-to-the-fda-opposing-approval-of-the-sleep-medicine-suvorexant/.
- ↑ 26.0 26.1 "A network meta-analysis of the long- and short-term efficacy of sleep medicines in adults and older adults". Neuroscience and Biobehavioral Reviews 131: 489–496. December 2021. doi:10.1016/j.neubiorev.2021.09.035. PMID 34560134.
- ↑ "Comparative efficacy of lemborexant and other insomnia treatments: a network meta-analysis". Journal of Managed Care & Specialty Pharmacy 27 (9): 1296–1308. September 2021. doi:10.18553/jmcp.2021.21011. PMID 34121443.
- ↑ "The efficacy and safety of dual orexin receptor antagonists in primary insomnia: A systematic review and network meta-analysis". Sleep Medicine Reviews 61: 101573. February 2022. doi:10.1016/j.smrv.2021.101573. PMID 34902823.
- ↑ "Effects of orexin receptor antagonism on human sleep architecture: A systematic review". Sleep Medicine Reviews 53: 101332. October 2020. doi:10.1016/j.smrv.2020.101332. PMID 32505969.
- ↑ 30.0 30.1 30.2 30.3 30.4 30.5 30.6 "Evaluating the role of orexins in the pathophysiology and treatment of depression: A comprehensive review". Progress in Neuro-Psychopharmacology & Biological Psychiatry 92: 1–7. June 2019. doi:10.1016/j.pnpbp.2018.12.008. PMID 30576764.
- ↑ 31.0 31.1 "Dual orexin receptor antagonists - promising agents in the treatment of sleep disorders". The International Journal of Neuropsychopharmacology 17 (1): 157–168. January 2014. doi:10.1017/S1461145713000552. PMID 23702225.
- ↑ "Suvorexant in the Treatment of Difficulty Falling and Staying Asleep (Insomnia)". Psychopharmacology Bulletin 52 (1): 68–90. February 2022. PMID 35342199.
- ↑ "Orexin receptor antagonists for the treatment of insomnia and potential treatment of other neuropsychiatric indications". Journal of Sleep Research 28 (2): e12782. April 2019. doi:10.1111/jsr.12782. PMID 30338596.
- ↑ 34.0 34.1 34.2 34.3 34.4 34.5 34.6 "Suvorexant: a dual orexin receptor antagonist for the treatment of sleep onset and sleep maintenance insomnia". The Annals of Pharmacotherapy 49 (4): 477–483. April 2015. doi:10.1177/1060028015570467. PMID 25667197.
- ↑ "Pharmacotherapies for sleep disturbances in dementia". The Cochrane Database of Systematic Reviews 2020 (11): CD009178. November 2020. doi:10.1002/14651858.CD009178.pub4. PMID 33189083.
- ↑ 36.0 36.1 36.2 36.3 "Effects of suvorexant, an orexin receptor antagonist, on sleep parameters as measured by polysomnography in healthy men". Sleep 36 (2): 259–267. February 2013. doi:10.5665/sleep.2386. PMID 23372274.
- ↑ "Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline". Journal of Clinical Sleep Medicine 13 (2): 307–349. February 2017. doi:10.5664/jcsm.6470. PMID 27998379.
- ↑ 38.0 38.1 38.2 38.3 "Abuse potential assessment of the new dual orexin receptor antagonist daridorexant in recreational sedative drug users as compared to suvorexant and zolpidem". Sleep 45 (3). March 2022. doi:10.1093/sleep/zsab224. PMID 34480579.
- ↑ 39.0 39.1 39.2 39.3 39.4 "Suvorexant Pregnancy and Breastfeeding Warnings". Drugs.com. https://www.drugs.com/pregnancy/suvorexant.html.
- ↑ 40.0 40.1 40.2 "Orexin/hypocretin receptor modulation of anxiolytic and antidepressive responses during social stress and decision-making: Potential for therapy". Brain Research 1731: 146085. March 2020. doi:10.1016/j.brainres.2018.12.036. PMID 30590027.
- ↑ "Adverse reaction with suvorexant for insomnia: acute worsening of depression with emergence of suicidal thoughts". BMJ Case Reports 2017. October 2017. doi:10.1136/bcr-2017-222037. PMID 29066641.
- ↑ "Novel class of medications, orexin receptor antagonists, in the treatment of insomnia - critical appraisal of suvorexant". Nature and Science of Sleep 8: 239–247. 2016. doi:10.2147/NSS.S76910. PMID 27471419.
- ↑ 43.0 43.1 "Neurobiology of the Orexin System and Its Potential Role in the Regulation of Hedonic Tone". Brain Sciences 12 (2): 150. January 2022. doi:10.3390/brainsci12020150. PMID 35203914.
- ↑ 44.0 44.1 44.2 "Hypocretin/orexin regulation of dopamine signaling: implications for reward and reinforcement mechanisms". Frontiers in Behavioral Neuroscience 6: 54. 2012. doi:10.3389/fnbeh.2012.00054. PMID 22933994.
- ↑ 45.0 45.1 "Motivational activation: a unifying hypothesis of orexin/hypocretin function". Nature Neuroscience 17 (10): 1298–1303. October 2014. doi:10.1038/nn.3810. PMID 25254979.
- ↑ 46.0 46.1 46.2 46.3 "The Insomnia-Addiction Positive Feedback Loop: Role of the Orexin System". Frontiers of Neurology and Neuroscience 45: 117–127. 2021. doi:10.1159/000514965. ISBN 978-3-318-06843-6. PMID 34052815.
- ↑ "Preclinical assessment of the abuse potential of the orexin receptor antagonist, suvorexant". Regulatory Toxicology and Pharmacology 86: 181–192. June 2017. doi:10.1016/j.yrtph.2017.03.006. PMID 28279667.
- ↑ "Nonclinical evaluation of abuse liability of the dual orexin receptor antagonist lemborexant". Regulatory Toxicology and Pharmacology 127: 105053. December 2021. doi:10.1016/j.yrtph.2021.105053. PMID 34619288.
- ↑ 49.0 49.1 "Quviviq (daridorexant) tablets, for oral use, [controlled substance schedule pending"]. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/214985s000lbl.pdf.
- ↑ "Dayvigo - lemborexant tablet, film coated". https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=7074cb65-77b3-45d2-8e8d-da8dc0f70bfd.
- ↑ 51.0 51.1 "Assessment of the Abuse Potential of the Orexin Receptor Antagonist, Suvorexant, Compared With Zolpidem in a Randomized Crossover Study". Journal of Clinical Psychopharmacology 36 (4): 314–323. August 2016. doi:10.1097/JCP.0000000000000516. PMID 27253658.
- ↑ 52.0 52.1 52.2 52.3 52.4 52.5 52.6 "International Union of Basic and Clinical Pharmacology. LXXXVI. Orexin receptor function, nomenclature and pharmacology". Pharmacological Reviews 64 (3): 389–420. July 2012. doi:10.1124/pr.111.005546. PMID 22759794.
- ↑ 53.0 53.1 53.2 53.3 53.4 "Orexin in sleep, addiction and more: is the perfect insomnia drug at hand?". Neuropeptides 47 (6): 477–488. December 2013. doi:10.1016/j.npep.2013.10.009. PMID 24215799.
- ↑ 54.0 54.1 54.2 54.3 54.4 "Effect of CYP3A Inhibition and Induction on the Pharmacokinetics of Suvorexant: Two Phase I, Open-Label, Fixed-Sequence Trials in Healthy Subjects". Clinical Drug Investigation 39 (5): 441–451. May 2019. doi:10.1007/s40261-019-00764-x. PMID 30810914.
- ↑ 55.0 55.1 "Sedatives and hypnotics". Side Effects of Drugs Annual. 42. Elsevier. 2020. pp. 67–79. doi:10.1016/bs.seda.2020.08.008. ISBN 9780128203309.
- ↑ "Drug Development and Drug Interactions | Table of Substrates, Inhibitors and Inducers". U.S. Food and Drug Administration. 10 March 2020. https://www.fda.gov/drugs/drug-interactions-labeling/drug-development-and-drug-interactions-table-substrates-inhibitors-and-inducers.
- ↑ 57.00 57.01 57.02 57.03 57.04 57.05 57.06 57.07 57.08 57.09 57.10 57.11 57.12 "The Discovery of Suvorexant, the First Orexin Receptor Drug for Insomnia". Annual Review of Pharmacology and Toxicology 57: 509–533. January 2017. doi:10.1146/annurev-pharmtox-010716-104837. PMID 27860547.
- ↑ 58.0 58.1 "Cocaine abuse and midbrain circuits: Functional anatomy of hypocretin/orexin transmission and therapeutic prospect". Brain Research 1731: 146164. March 2020. doi:10.1016/j.brainres.2019.02.026. PMID 30796894.
- ↑ 59.00 59.01 59.02 59.03 59.04 59.05 59.06 59.07 59.08 59.09 59.10 "Orexin receptors: pharmacology and therapeutic opportunities". Annual Review of Pharmacology and Toxicology 51: 243–266. 2011. doi:10.1146/annurev-pharmtox-010510-100528. PMID 21034217.
- ↑ 60.0 60.1 "Hypocretins (Orexins): Twenty Years of Dissecting Arousal Circuits". The Orexin/Hypocretin System: Functional Roles and Therapeutic Potential. Elsevier. 2019. pp. 1–29. doi:10.1016/B978-0-12-813751-2.00001-2. ISBN 9780128137512.
- ↑ 61.0 61.1 61.2 "Orexin receptor antagonists: a new concept in CNS disorders?". ChemMedChem 5 (8): 1197–1214. August 2010. doi:10.1002/cmdc.201000132. PMID 20544785.
- ↑ 62.0 62.1 62.2 62.3 "The role of hypocretins (orexins) in sleep regulation and narcolepsy". Annual Review of Neuroscience 25: 283–313. 2002. doi:10.1146/annurev.neuro.25.112701.142826. PMID 12052911.
- ↑ "Orexins/hypocretins and aminergic systems". Acta Physiologica 198 (3): 263–275. March 2010. doi:10.1111/j.1748-1716.2009.02015.x. PMID 19566795.
- ↑ 64.0 64.1 64.2 64.3 "Orexin (hypocretin) receptor agonists and antagonists for treatment of sleep disorders. Rationale for development and current status". CNS Drugs 27 (2): 83–90. February 2013. doi:10.1007/s40263-012-0036-8. PMID 23359095.
- ↑ 65.0 65.1 65.2 "Hypocretin (orexin) biology and the pathophysiology of narcolepsy with cataplexy". The Lancet. Neurology 14 (3): 318–328. March 2015. doi:10.1016/S1474-4422(14)70218-2. PMID 25728441.
- ↑ 66.0 66.1 66.2 66.3 "Hypocretin/orexin and narcolepsy: new basic and clinical insights". Acta Physiologica 198 (3): 209–222. March 2010. doi:10.1111/j.1748-1716.2009.02012.x. PMID 19555382.
- ↑ 67.0 67.1 "Sleep disorders, obesity, and aging: the role of orexin". Ageing Research Reviews 20: 63–73. March 2015. doi:10.1016/j.arr.2014.11.001. PMID 25462194.
- ↑ "Roles of aging in sleep". Neuroscience and Biobehavioral Reviews 98: 177–184. March 2019. doi:10.1016/j.neubiorev.2019.01.013. PMID 30648559.
- ↑ 69.0 69.1 69.2 "Orexin OX2 Receptor Antagonists as Sleep Aids". Current Topics in Behavioral Neurosciences (Springer International Publishing) 33: 105–136. 2016. doi:10.1007/7854_2016_47. ISBN 978-3-319-57534-6. PMID 27909987.
- ↑ 70.0 70.1 70.2 "Orexin Receptor Antagonists: New Therapeutic Agents for the Treatment of Insomnia". Journal of Medicinal Chemistry 59 (2): 504–530. January 2016. doi:10.1021/acs.jmedchem.5b00832. PMID 26317591.
- ↑ "Induction of narcolepsy-like symptoms by orexin receptor antagonists in mice". Sleep 44 (8). August 2021. doi:10.1093/sleep/zsab043. PMID 33609365.
- ↑ 72.0 72.1 "Safety, Tolerability, and Pharmacokinetics of Suvorexant: A Randomized Rising-Dose Trial in Healthy Men". Clinical Drug Investigation 38 (7): 631–638. July 2018. doi:10.1007/s40261-018-0650-4. PMID 29705869.
- ↑ 73.0 73.1 "Evidence-based insomnia treatment strategy using novel orexin antagonists: A review". Neuropsychopharmacol Rep 41 (4): 450–458. December 2021. doi:10.1002/npr2.12205. PMID 34553844.
- ↑ "Effects of TS-142, a novel dual orexin receptor antagonist, on sleep in patients with insomnia: a randomized, double-blind, placebo-controlled phase 2 study". Psychopharmacology 239 (7): 2143–2154. March 2022. doi:10.1007/s00213-022-06089-6. PMID 35296912.
- ↑ 75.0 75.1 "Small-molecule antagonists of the orexin receptors". Pharmaceutical Patent Analyst 3 (6): 625–638. 2014. doi:10.4155/ppa.14.46. PMID 25489915.
- ↑ "Discovery of the dual orexin receptor antagonist [(7R)-4-(5-chloro-1,3-benzoxazol-2-yl)-7-methyl-1,4-diazepan-1-yl][5-methyl-2-(2H-1,2,3-triazol-2-yl)phenyl]methanone (MK-4305) for the treatment of insomnia". Journal of Medicinal Chemistry 53 (14): 5320–5332. July 2010. doi:10.1021/jm100541c. PMID 20565075.
- ↑ "FDA approves new type of sleep drug, Belsomra". U.S. Food and Drug Administration (FDA) (Press release). 13 August 2014. Archived from the original on 14 February 2017. Retrieved 30 January 2020.
- ↑ 78.0 78.1 "Merck's Insomnia Medicine Belsomra C-IV Now Available in US". Sleep Review. 3 February 2015. http://www.sleepreviewmag.com/2015/02/mercks-insomnia-medicine-belsomra-c-iv-now-available-us/.
- ↑ 79.0 79.1 "Regulatory Decision Summary - Belsomra - Health Canada". Government of Canada. 23 October 2014. https://hpr-rps.hres.ca/reg-content/regulatory-decision-summary-detail.php?lang=en&linkID=RDS00475.
- ↑ "Suvorexant [USAN:INN"]. ChemIDplus. U.S. National Library of Medicine. https://chem.nlm.nih.gov/chemidplus/name/suvorexant%20%5Busan%3Ainn%5D.
- ↑ "Suvorexant". KEGG DRUG Database. https://www.kegg.jp/entry/D10082.
- ↑ 82.0 82.1 82.2 "Availability". IBM Micromedex. https://www.micromedexsolutions.com/micromedex2/librarian/.
- ↑ "Drug Product Database online query". Government of Canada. 25 April 2012. https://health-products.canada.ca/dpd-bdpp/.
- ↑ "No search results for suvorexant". Datapharm. Electronic Medicines Compendium (EMC). https://www.medicines.org.uk/emc/search?q=suvorexant.
- ↑ "Search for Suvorexant: 0 results". European Medicines Agency. https://www.ema.europa.eu/en/medicines?search_api_views_fulltext=Suvorexant.
- ↑ Drug Enforcement Administration, Department of Justice (August 2014). "Schedules of controlled substances: placement of suvorexant into Schedule IV. Final rule". Federal Register 79 (167): 51243–51247. PMID 25167596. http://www.gpo.gov/fdsys/pkg/FR-2014-08-28/pdf/2014-20515.pdf.
- ↑ "Rules - 2014 - Final Rule: Placement of Suvorexant into Schedule IV". http://www.deadiversion.usdoj.gov/fed_regs/rules/2014/fr0828.htm.
- ↑ "Here's why you can skip the new insomnia drug, Belsomra: It's expensive, barely helps, and poses safety concerns". Consumer Report. 12 July 2015. https://www.consumerreports.org/cro/news/2015/07/skip-new-insomnia-drug-belsomra/index.htm.
- ↑ "FDA Fields Complaints on Sleeping Pill Suvorexant: A recent analysis looks into reports of problems with the prescription sleep drug Belsomra". Consumer Reports. 5 February 2016. https://www.consumerreports.org/drugs/fda-fields-complaints-on-sleeping-pill-suvorexant-belsomra/.
- ↑ 90.0 90.1 "Suvorexant - Merck & Co". AdisInsight. Springer Nature Switzerland AG. https://adisinsight.springer.com/drugs/800027707.
- ↑ 91.0 91.1 "Neuroendocrine, Autonomic, and Metabolic Responses to an Orexin Antagonist, Suvorexant, in Psychiatric Patients with Insomnia". Innovations in Clinical Neuroscience 14 (3–4): 30–37. 2017. PMID 28584695.
- ↑ 92.0 92.1 92.2 "Targeting the orexin/hypocretin system for the treatment of neuropsychiatric and neurodegenerative diseases: From animal to clinical studies". Front Neuroendocrinol 69: 101066. April 2023. doi:10.1016/j.yfrne.2023.101066. PMID 37015302.
- ↑ Clinical trial number NCT02669030 for "A Six Week, Randomized, Double-Blind Placebo-Controlled, Suvorexant Augmentation Study of Antidepressant Treatment of Major Depressive Disorder With Residual Insomnia" at ClinicalTrials.gov
- ↑ "Orexin Receptor Antagonists as Emerging Treatments for Psychiatric Disorders". Neuroscience Bulletin 36 (4): 432–448. April 2020. doi:10.1007/s12264-019-00447-9. PMID 31782044.
- ↑ "A Decade of Orexin/Hypocretin and Addiction: Where Are We Now?". Current Topics in Behavioral Neurosciences 33: 247–281. 2017. doi:10.1007/7854_2016_57. ISBN 978-3-319-57534-6. PMID 28012090.
- ↑ "Suvorexant to treat alcohol use disorder and comorbid insomnia: Plan for a phase II trial". Brain Research 1728: 146597. February 2020. doi:10.1016/j.brainres.2019.146597. PMID 31837287.
- ↑ "The Role of Orexins/Hypocretins in Alcohol Use and Abuse". Current Topics in Behavioral Neurosciences 33: 221–246. 2017. doi:10.1007/7854_2016_55. ISBN 978-3-319-57534-6. PMID 27909991.
- ↑ "A sleeping giant: Suvorexant for the treatment of alcohol use disorder?". Brain Research 1731: 145902. March 2020. doi:10.1016/j.brainres.2018.08.005. PMID 30081035.
- ↑ "Repurposing the dual orexin receptor antagonist suvorexant for the treatment of opioid use disorder: why sleep on this any longer?". Neuropsychopharmacology 45 (5): 717–719. April 2020. doi:10.1038/s41386-020-0619-x. PMID 31986520.
- ↑ "Suvorexant Acutely Decreases Tau Phosphorylation and Aβ in the Human CNS". Ann Neurol 94 (1): 27–40. March 2023. doi:10.1002/ana.26641. PMID 36897120.
- ↑ 101.0 101.1 "Sleep disorders in people with type 2 diabetes and associated health outcomes: a review of the literature". Diabetologia 64 (11): 2367–2377. November 2021. doi:10.1007/s00125-021-05541-0. PMID 34401953.
- ↑ 102.0 102.1 "Chronotherapeutic efficacy of suvorexant on sleep quality and metabolic parameters in patients with type 2 diabetes and insomnia". Diabetes Research and Clinical Practice 169: 108412. November 2020. doi:10.1016/j.diabres.2020.108412. PMID 32911037.
Further reading
- Merck Sharp and Dohme Corporation (22 May 2013). "Suvorexant Advisory Committee Meeting Briefing Document: Peripheral & Central Nervous System Drugs Advisory Committee Meeting". https://www.fda.gov/downloads/advisorycommittees/committeesmeetingmaterials/drugs/peripheralandcentralnervoussystemdrugsadvisorycommittee/ucm352970.pdf.
- "Application Number: 204569Orig1s000. Clinical Pharmacology/Biopharmaceutics Review. Suvorexant (MK-4305).". Center for Drug Evaluation and Research (Food and Drug Administration). 2014. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/204569Orig1s000ClinPharmR.pdf.
External links
- "The Big Sleep". The New Yorker. 9 December 2013. https://www.newyorker.com/magazine/2013/12/09/the-big-sleep-2.
 |