Chemistry:Glipizide
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Glucotrol, Glucotrol XL, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a684060 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth |
| Drug class | Sulfonylurea |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 100% (regular formulation) 90% (extended release) |
| Protein binding | 98 to 99% |
| Metabolism | Liver hydroxylation |
| Elimination half-life | 2 to 5 hours |
| Excretion | Kidney and fecal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
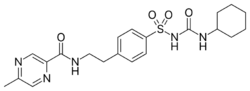
| Formula | C21H27N5O4S |
| Molar mass | 445.54 g·mol−1 |
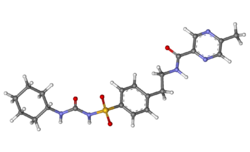
| 3D model (JSmol) | |
| Melting point | 208 to 209 °C (406 to 408 °F) |
| |
| |
| | |
Glipizide, sold under the brand name Glucotrol among others, is an anti-diabetic medication of the sulfonylurea class used to treat type 2 diabetes.[1][2] It is used together with a diabetic diet and exercise.[1][2] It is not indicated for use by itself in type 1 diabetes.[1][2] It is taken by mouth.[1][2] Effects generally begin within half an hour and can last for up to a day.[1]
Common side effects include nausea, diarrhea, low blood sugar, and headache.[1] Other side effects include sleepiness, skin rash, and shakiness.[3] The dose may need to be adjusted in those with liver or kidney disease.[1] Use during pregnancy or breastfeeding is not recommended.[3] It works by stimulating the pancreas to release insulin and increases tissue sensitivity to insulin.[1]
Glipizide was approved for medical use in the United States in 1984.[1] It is available as a generic medication.[1] In 2021, it was the 48th most commonly prescribed medication in the United States, with more than 13 million prescriptions.[4][5]
Mechanism of action
Glipizide sensitizes the beta cells of pancreatic islets of Langerhans insulin response, meaning that more insulin is released in response to glucose than would be without glipizide ingestion.[2] Glipizide acts by partially blocking potassium channels among beta cells of pancreatic islets of Langerhans. By blocking potassium channels, the cell depolarizes, which results in the opening of voltage-gated calcium channels. The resulting calcium influx encourages insulin release from beta cells.[6]
History
It was patented in 1969, and approved for medical use in 1971.[7] Glipizide was approved for medical use in the United States in 1984.[1]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 "Glipizide Monograph for Professionals". Drugs.com. AHFS. https://www.drugs.com/monograph/glipizide.html.
- ↑ 2.0 2.1 2.2 2.3 2.4 "Glucotrol XL- glipizide tablet, extended release". 17 August 2018. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=eed99b60-d043-4249-9b2a-f05e46fb588d.
- ↑ 3.0 3.1 British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 693. ISBN 9780857113382.
- ↑ "The Top 300 of 2021". https://clincalc.com/DrugStats/Top300Drugs.aspx.
- ↑ "Glipizide - Drug Usage Statistics". ClinCalc. https://clincalc.com/DrugStats/Drugs/Glipizide.
- ↑ "The mechanism of action of oral antidiabetic drugs: a review of recent literature.". Journal of Endocrinology, Metabolism and Diabetes of South Africa 13 (3): 80–8. December 2008. doi:10.1080/22201009.2008.10872177.
- ↑ Analogue-based Drug Discovery. John Wiley & Sons. 2006. p. 449. ISBN 9783527607495. https://books.google.com/books?id=FjKfqkaKkAAC&pg=PA449.
 |
