Chemistry:Dopamine antagonist
| Dopamine receptor antagonist Dopaminergic blockers | |
|---|---|
| Drug class | |
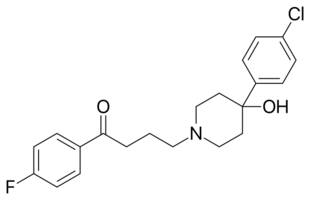 Skeletal structural formula of Haloperidol, a typical antipsychotic | |
| Class identifiers | |
| Use | Schizophrenia, bipolar disorder, nausea and vomiting, etc. |
| ATC code | N05A |
| Biological target | Dopamine receptors |
| External links | |
| MeSH | D012559 |
A dopamine antagonist, also known as an anti-dopaminergic and a dopamine receptor antagonist (DRA), is a type of drug which blocks dopamine receptors by receptor antagonism. Most antipsychotics are dopamine antagonists, and as such they have found use in treating schizophrenia, bipolar disorder, and stimulant psychosis.[1] Several other dopamine antagonists are antiemetics used in the treatment of nausea and vomiting.
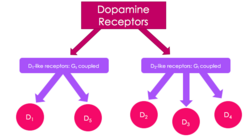
Receptor pharmacology
Dopamine receptors are all G protein–coupled receptors, and are divided into two classes based on which G-protein they are coupled to.[2] The D1-like class of dopamine receptors is coupled to Gαs/olf and stimulates adenylate cyclase production, whereas the D2-like class is coupled to Gαi/o and thus inhibits adenylate cyclase production.[2]
D1-like receptors: D1 and D5
D1-like receptors – D1 and D5 are always found post-synaptically. The genes coding these receptors lack introns, so there are no splice variants.
D1 receptors
- D1 receptors are found mainly on neurons in the nucleus accumbens[3] as well as substantia nigra,[2] striatum,[2] amygdala,[2] frontal cortex[2] and olfactory bulb and retina[2]
- Also found (in lower levels) in the hypothalamus, thalamus, cerebellum and hippocampus[2]
- Peripherally, these receptors have been found in the renal artery, mesenteric artery, and splenic artery where activation leads to vasodilation.[4] In addition, D1 receptors have been found in the kidney[4]
D5 receptors
- Low levels of D5 receptors have been found in the hypothalamus, prefrontal cortex and cingulate cortex; as well as memory areas such as hippocampus, dentate gyrus and entorhinal cortex.[2]
- In addition, D5 receptors have been found in the kidney[4]
D2-like receptors: D2, D3 and D4
D2-like receptors unlike the D1-like class, these receptors are found pre and post-synaptically. The genes that code these receptors have introns, leading to many alternately spliced variants.
D2 receptors
- D2 receptors are found in the striatum, substantia nigra, ventral tegmental area, hypothalamus, cortex, septum, amygdala, hippocampus, and olfactory tubercle.[2]
- These receptors have also been found in the retina and pituitary gland.[2]
- Peripherally, these receptors have been found in the renal, mesenteric, and splenic arteries as well as on the adrenal cortex and medulla and within the kidney.[4]
D3 receptors
- D3 receptors are highly expressed on neurons in islands of Calleja and nucleus accumbens shell and lowly expressed in areas such as the substantia nigra pars compacta, hippocampus, septal area, and ventral tegmental area.[2][3]
- Additional studies have found these receptors peripherally in the kidney[4]
D4 receptors
- D4 receptors are found in amygdala, hippocampus, hypothalamus, globus pallidus, substantia nigra pars reticula, the thalamus, the retina and the kidney[2][4]
Implications in disease
The dopaminergic system has been implicated in a variety of disorders. Parkinson's disease results from loss of dopaminergic neurons in the striatum.[5] Furthermore, most effective antipsychotics block D2 receptors, suggesting a role for dopamine in schizophrenia.[5][6][7] Additional studies hypothesize dopamine dysregulation is involved in Huntington's disease, ADHD, Tourette's syndrome, major depression, manic depression, addiction, hypertension and kidney dysfunction.[5][7][8] Dopamine receptor antagonists are used for some diseases such as schizophrenia, bipolar disorder, nausea and vomiting.[5]
- Melatonin suppresses dopamine activity[9] as part of normal circadian rhythm functions, although pathological imbalances have been implicated in Parkinson's disease[10]
Side effects
They may include one or more of the following and last indefinitely even after cessation of the dopamine antagonist, especially after long-term or high-dosage use:
- Cardiovascular disease[11][12]
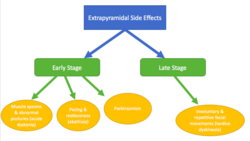
- Extrapyramidal symptoms (EPS) associated with typical antipsychotics:
- Early stage – occurs at onset of treatment or following increased dose, patients recover when dose is decreased[13]
- Acute dystonias[13] – muscle spasms and sustained abnormal postures and onset occurs within a few days; can be treated with anticholinergics
- risk factors include age, gender and family history[13]
- Akathisia[13][14] - pacing and restlessness and onset occurs within the first few months; can be treated with beta blockers and benzodiazepines
- Parkinsonism due to effects on the nigrostriatal pathway[13][14] - includes tremors, bradykinesia and muscle rigidity
- risk factors include age and gender[13]
- Acute dystonias[13] – muscle spasms and sustained abnormal postures and onset occurs within a few days; can be treated with anticholinergics
- Late stage – occurs after prolonged (months-years) treatment, symptoms persist even after dose is decreased[13]
- Tardive dyskinesia[13][14] - includes involuntary and repetitive facial movements
- risk factors include age, race and gender[13]
- Tardive dyskinesia[13][14] - includes involuntary and repetitive facial movements
- It is hypothesized that these effects are due to chronic blockade of the D2 receptor[14]
- Early stage – occurs at onset of treatment or following increased dose, patients recover when dose is decreased[13]
- Hyperprolactinaemia due to blockade of the D2 receptors in the anterior pituitary leading to increased prolactin release[11][15]
- Increased appetite including increased craving and binge eating that lead to weight gain[11][16][17]
- Increased risk for insulin resistance[16]
- Sexual dysfunction[11][12]
- Metabolic changes with increased risk of obesity and diabetes mellitus type 2[11][16]
- Sedation[11][12]
- Neuroleptic Malignant Syndrome[18] is a medical emergency caused by a decrease in dopaminergic activity, resulting in a central D2 receptor blockade.[18]
Examples
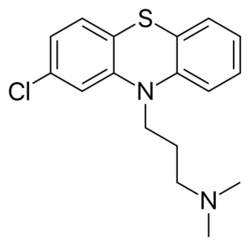
First-generation antipsychotics (typical)
First generation antipsychotics are used to treat schizophrenia and are often accompanied by extrapyramidal side effects.[19] They inhibit dopaminergic neurotransmission in the brain by blocking about 72% of the D2 dopamine receptors.[20] They can also block noradrenergic, cholinergic, and histaminergic activity.[20]
- Benperidol[19] binds D2 and some serotonin receptors.[21] It is absorbed very easily and has a high first pass effect.[21]
- Chlorpromazine binds D3 with the highest affinity, but also binds D1, D2, D4 and D5[22][23]
- Clopenthixol[19]
- Droperidol is used as an antipsychotic and antiemetic.[19]
- Haloperidol binds D2, D3 and D4 with the highest affinity, but also binds D1 and D5.[19][22][23] Haloperidol also has a risk for QTc prolongation. [24]
- Fluphenazine binds D2 and D3 with the highest affinity but D1 and D5 as well[19][22]
- Flupentixol binds D1, D2, D3, and D5[22] and is also used as an antidepressant.[19]
- Fluspirilene[19]
- Penfluridol[19]
- Perazine[19]
- Perphenazine[19]
- Pimozide binds D2 and D3 with high affinity, also binds D4 receptors[19][22]
- Sulpiride binds D2 and D3[19][22] and is also used as an antidepressant.[19]
- Thioridazine binds D2, D3 and D4 with high affinity; can also bind D1 and D5 at higher concentrations[22] Thioridazine has the highest associated risk of QTc prolongation among neuroleptics.[24]
Second-generation antipsychotics (atypical)
These drugs are not only dopamine antagonists at the receptor specified, but also act on serotonin receptor 5HT2A.[20][25] These drugs have less extrapyramidal side effects and are less likely to affect prolactin levels when compared to typical antipsychotics.[26]
- Amisulpride binds D2 and D3[27] and is used as an antipsychotic, antidepressant and also treats bipolar disorder.[25] It treats both the positive and negative symptoms of schizophrenia.[28]
- Asenapine binds D2, D3 and D4[29] and is used to treat bipolar disorder and schizophrenia.[30] Its side effects include weight gain but there is lower risk for orthostatic hypotension and hyperprolactinemia.
- Aripiprazole binds D2 as a partial agonist but antagonizes D3.[31] In addition, aripiprazole treats schizophrenia, bipolar disorder (mania),[32] depression,[25] and tic disorders[31]
- Clozapine binds D1 and D4 with the highest affinity but still binds D2 and D3.[33] Clozapine is unique because it is only prescribed when treatment with at least two other antipsychotics has failed due to its very harsh side effects.[34] It also requires weekly white blood cell counts to monitor potential neutropenia.[34]
- Loxapine binds D2, D3 and D4 with high affinity; can also bind D1.[35] Loxapine is often used to treat agitated and violent patients with neuropsychiatric disorders such as bipolar disorder and schizophrenia.[36]
- Nemonapride binds D3, D4 and D5.[37]
- Olanzapine binds all receptors[38] and is used to treat the positive and negative symptoms of schizophrenia as well as bipolar disorder and depression.[39] It has been associated with significant weight gain.[40]
- Quetiapine binds D1, D2 and D3 and can bind D4 at high concentrations.[38] It is used to treat the positive symptoms of schizophrenia,[40] bipolar disorder and depression.[39] Of the second generation antipsychotics, quetiapine may produce fewer parkinsonian side effects.[41]
- Paliperidone binds D2, D3 and D4 with high affinity; can also bind D1 and D5.[42]
- Remoxipride binds D2 receptors with relatively low affinity.[38][43][39]
- Risperidone binds D2, D3 and D4 receptors.[39][38][42] Risperidone not only treats the positive and negative symptoms of schizophrenia[40] but also treats bipolar disorder.[39]
- Tiapride blocks D2 and D3 and is used as an antipsychotic.[39] It is also often used to treat dyskinesias, psychomotor agitations, tics, Huntington's chorea and alcohol dependence.[44]
- Ziprasidone blocks the D2 receptor[45] and is used to treat schizophrenia, depression and bipolar disorder.[39] There is controversy on whether Ziprasidone treats negative symptoms and it has well documented gastrointestinal side effects.[40] Ziprasidone can also cause QTc prolongation.[24]
Dopamine antagonists used to treat nausea and vomiting
- Domperidone is a peripherally selective dopamine D2 receptor antagonist used as an antiemetic, gastroprokinetic agent and galactagogue.
- Bromopride binds enteric D2 receptors[46] and also treats gastroparesis.[47]
- Metoclopramide also treats gastroparesis[47]
Antagonists used only in research settings
- Eticlopride binds D2 and D3 with high affinity but also binds D4[48][49][50]
- Nafadotride binds D2 and D3[47][48][49]
- Raclopride binds D2 and D3[47][48] and can be radiolabeled and used in PET imaging to identify disease progression in Huntington's Disease[51]
References
- ↑ "The physiology, signaling, and pharmacology of dopamine receptors". Pharmacological Reviews 63 (1): 182–217. March 2011. doi:10.1124/pr.110.002642. PMID 21303898.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 "The physiology, signaling, and pharmacology of dopamine receptors". Pharmacological Reviews 63 (1): 182–217. March 2011. doi:10.1124/pr.110.002642. PMID 21303898.
- ↑ 3.0 3.1 "The dopamine D3 receptor: a therapeutic target for the treatment of neuropsychiatric disorders". CNS & Neurological Disorders Drug Targets 5 (1): 25–43. February 2006. doi:10.2174/187152706784111551. PMID 16613552.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 "Dopamine receptors: from structure to function". Physiological Reviews 78 (1): 189–225. January 1998. doi:10.1152/physrev.1998.78.1.189. PMID 9457173.
- ↑ 5.0 5.1 5.2 5.3 "The physiology, signaling, and pharmacology of dopamine receptors". Pharmacological Reviews 63 (1): 182–217. March 2011. doi:10.1124/pr.110.002642. PMID 21303898.
- ↑ "Targeting the dopamine D2 receptor in schizophrenia". Expert Opinion on Therapeutic Targets 10 (4): 515–31. August 2006. doi:10.1517/14728222.10.4.515. PMID 16848689.
- ↑ 7.0 7.1 "Dopamine receptors: from structure to function". Physiological Reviews 78 (1): 189–225. January 1998. doi:10.1152/physrev.1998.78.1.189. PMID 9457173.
- ↑ "Dopamine: 50 years in perspective". Trends in Neurosciences 30 (5): 188–93. May 2007. doi:10.1016/j.tins.2007.03.002. PMID 17368565.
- ↑ "Melatonin-dopamine interactions: from basic neurochemistry to a clinical setting". Cellular and Molecular Neurobiology 21 (6): 605–16. December 2001. doi:10.1023/A:1015187601628. PMID 12043836.
- ↑ "Parkinson's disease as a neuroendocrine disorder of circadian function: dopamine-melatonin imbalance and the visual system in the genesis and progression of the degenerative process". Reviews in the Neurosciences 19 (4–5): 245–316. 2008. doi:10.1515/revneuro.2008.19.4-5.245. PMID 19145986.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 ""First do no harm." A systematic review of the prevalence and management of antipsychotic adverse effects". Journal of Psychopharmacology 29 (4): 353–62. April 2015. doi:10.1177/0269881114562090. PMID 25516373.
- ↑ 12.0 12.1 12.2 "An overview of side effects caused by typical antipsychotics". The Journal of Clinical Psychiatry 61 (Suppl 8): 5–11; discussion 12–3. 2000. PMID 10811237.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 13.8 "Second-generation antipsychotics and extrapyramidal adverse effects". BioMed Research International 2014: 656370. 2014. doi:10.1155/2014/656370. PMID 24995318.
- ↑ 14.0 14.1 14.2 14.3 "Dopamine receptors: from structure to function". Physiological Reviews 78 (1): 189–225. January 1998. doi:10.1152/physrev.1998.78.1.189. PMID 9457173.
- ↑ "Pharmacology of the atypical antipsychotic remoxipride, a dopamine D2 receptor antagonist". CNS Drug Reviews 7 (3): 265–82. 2001. doi:10.1111/j.1527-3458.2001.tb00199.x. PMID 11607043.
- ↑ 16.0 16.1 16.2 "Effects of antipsychotic medications on appetite, weight, and insulin resistance". Endocrinology and Metabolism Clinics of North America 42 (3): 545–63. September 2013. doi:10.1016/j.ecl.2013.05.006. PMID 24011886. https://ro.uow.edu.au/cgi/viewcontent.cgi?article=1371&context=ihmri.
- ↑ "How do we choose between atypical antipsychotics? The advantages of amisulpride". The International Journal of Neuropsychopharmacology 7 Suppl 1 (5): S21-5. March 2004. doi:10.1017/S1461145704004134. PMID 14972081.
- ↑ 18.0 18.1 Berman, Brian (January 2011). "Neuroleptic Malignant Syndrome". The Neuro Hospitalists 1 (1): 41–47. doi:10.1177/1941875210386491. PMID 23983836.
- ↑ 19.00 19.01 19.02 19.03 19.04 19.05 19.06 19.07 19.08 19.09 19.10 19.11 19.12 19.13 19.14 "The physiology, signaling, and pharmacology of dopamine receptors". Pharmacological Reviews 63 (1): 182–217. March 2011. doi:10.1124/pr.110.002642. PMID 21303898.
- ↑ 20.0 20.1 20.2 Chokhawala, Krutika (2 October 2021). "Antipsychotic Medications". StatPearls. PMID 30137788. https://www.ncbi.nlm.nih.gov/books/NBK519503/#:~:text=Go%20to%3A-,Mechanism%20of%20Action,cholinergic%2C%20and%20histaminergic%20blocking%20action..
- ↑ 21.0 21.1 "Benperidol for schizophrenia". The Cochrane Database of Systematic Reviews 2005 (2): CD003083. April 2005. doi:10.1002/14651858.CD003083.pub2. PMID 15846648.
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 22.6 22.7 "The dopamine D3 receptor: a therapeutic target for the treatment of neuropsychiatric disorders". CNS & Neurological Disorders Drug Targets 5 (1): 25–43. February 2006. doi:10.2174/187152706784111551. PMID 16613552.
- ↑ 23.0 23.1 "Dopamine receptors: from structure to function". Physiological Reviews 78 (1): 189–225. January 1998. doi:10.1152/physrev.1998.78.1.189. PMID 9457173.
- ↑ 24.0 24.1 24.2 Beach, Scott (2013). "QTc prolongation, torsades de pointes, and psychotropic medications". The Academy of Psychosomatic Medicine 54 (1): 1–13. doi:10.1016/j.psym.2012.11.001. PMID 23295003.
- ↑ 25.0 25.1 25.2 "The physiology, signaling, and pharmacology of dopamine receptors". Pharmacological Reviews 63 (1): 182–217. March 2011. doi:10.1124/pr.110.002642. PMID 21303898.
- ↑ "Pharmacology of the atypical antipsychotic remoxipride, a dopamine D2 receptor antagonist". CNS Drug Reviews 7 (3): 265–82. 2001. doi:10.1111/j.1527-3458.2001.tb00199.x. PMID 11607043.
- ↑ "The dopamine D3 receptor: a therapeutic target for the treatment of neuropsychiatric disorders". CNS & Neurological Disorders Drug Targets 5 (1): 25–43. February 2006. doi:10.2174/187152706784111551. PMID 16613552.
- ↑ "How do we choose between atypical antipsychotics? The advantages of amisulpride". The International Journal of Neuropsychopharmacology 7 Suppl 1 (5): S21-5. March 2004. doi:10.1017/S1461145704004134. PMID 14972081.
- ↑ "Asenapine: a clinical review of a second-generation antipsychotic". Clinical Therapeutics 34 (5): 1023–40. May 2012. doi:10.1016/j.clinthera.2012.03.002. PMID 22494521.
- ↑ "Asenapine for bipolar disorder". Neuropsychiatric Disease and Treatment 11: 3007–17. 2015-12-04. doi:10.2147/NDT.S78043. PMID 26674884.
- ↑ 31.0 31.1 "Aripiprazole for the treatment of tic disorders in children: a systematic review and meta-analysis". BMC Psychiatry 15: 179. July 2015. doi:10.1186/s12888-015-0504-z. PMID 26220447.
- ↑ "Aripiprazole alone or in combination for acute mania". The Cochrane Database of Systematic Reviews (12): CD005000. December 2013. doi:10.1002/14651858.CD005000.pub2. PMID 24346956. https://kclpure.kcl.ac.uk/portal/files/32075532/2013_brown_taylor_geddes_aripiprazole_mania_cochrane.pdf.
- ↑ "The dopamine D3 receptor: a therapeutic target for the treatment of neuropsychiatric disorders". CNS & Neurological Disorders Drug Targets 5 (1): 25–43. February 2006. doi:10.2174/187152706784111551. PMID 16613552.
- ↑ 34.0 34.1 "How do we choose between atypical antipsychotics? The advantages of amisulpride". The International Journal of Neuropsychopharmacology 7 Suppl 1 (5): S21-5. March 2004. doi:10.1017/S1461145704004134. PMID 14972081.
- ↑ "Revisiting loxapine: a systematic review". Annals of General Psychiatry 14: 15. 2015-04-01. doi:10.1186/s12991-015-0053-3. PMID 25859275.
- ↑ "Inhaled loxapine for the urgent treatment of acute agitation associated with schizophrenia or bipolar disorder". Current Medical Research and Opinion 32 (7): 1253–60. July 2016. doi:10.1185/03007995.2016.1170004. PMID 27121764.
- ↑ "Dopamine receptors: from structure to function". Physiological Reviews 78 (1): 189–225. January 1998. doi:10.1152/physrev.1998.78.1.189. PMID 9457173.
- ↑ 38.0 38.1 38.2 38.3 "The dopamine D3 receptor: a therapeutic target for the treatment of neuropsychiatric disorders". CNS & Neurological Disorders Drug Targets 5 (1): 25–43. February 2006. doi:10.2174/187152706784111551. PMID 16613552.
- ↑ 39.0 39.1 39.2 39.3 39.4 39.5 39.6 "The physiology, signaling, and pharmacology of dopamine receptors". Pharmacological Reviews 63 (1): 182–217. March 2011. doi:10.1124/pr.110.002642. PMID 21303898.
- ↑ 40.0 40.1 40.2 40.3 "How do we choose between atypical antipsychotics? The advantages of amisulpride". The International Journal of Neuropsychopharmacology 7 Suppl 1 (5): S21-5. March 2004. doi:10.1017/S1461145704004134. PMID 14972081.
- ↑ Asmal, Laila (2013). "Quetiapine versus other atypical antipsychotics for schizophrenia". Cochrane Database of Systematic Reviews (11): CD006625. doi:10.1002/14651858.CD006625.pub3. PMID 24249315. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006625.pub3/full.
- ↑ 42.0 42.1 "Comparative Pharmacology of Risperidone and Paliperidone". Drugs in R&D 15 (2): 163–74. June 2015. doi:10.1007/s40268-015-0092-x. PMID 25943458.
- ↑ "Pharmacology of the atypical antipsychotic remoxipride, a dopamine D2 receptor antagonist". CNS Drug Reviews 7 (3): 265–82. 2001. doi:10.1111/j.1527-3458.2001.tb00199.x. PMID 11607043.
- ↑ "The benzamide tiapride: treatment of extrapyramidal motor and other clinical syndromes". Pharmacopsychiatry 33 (1): 19–27. January 2000. doi:10.1055/s-2000-7964. PMID 10721880.
- ↑ "The psychopharmacology of ziprasidone: receptor-binding properties and real-world psychiatric practice". The Journal of Clinical Psychiatry 64 (Suppl 19): 6–12. 2003. PMID 14728084.
- ↑ "Review article: clinical implications of enteric and central D2 receptor blockade by antidopaminergic gastrointestinal prokinetics". Alimentary Pharmacology & Therapeutics 19 (4): 379–90. February 2004. doi:10.1111/j.1365-2036.2004.01867.x. PMID 14871277.
- ↑ 47.0 47.1 47.2 47.3 "The physiology, signaling, and pharmacology of dopamine receptors". Pharmacological Reviews 63 (1): 182–217. March 2011. doi:10.1124/pr.110.002642. PMID 21303898.
- ↑ 48.0 48.1 48.2 "The dopamine D3 receptor: a therapeutic target for the treatment of neuropsychiatric disorders". CNS & Neurological Disorders Drug Targets 5 (1): 25–43. February 2006. doi:10.2174/187152706784111551. PMID 16613552.
- ↑ 49.0 49.1 "Dopamine receptors: from structure to function". Physiological Reviews 78 (1): 189–225. January 1998. doi:10.1152/physrev.1998.78.1.189. PMID 9457173.
- ↑ "A review of the discovery, pharmacological characterization, and behavioral effects of the dopamine D2-like receptor antagonist eticlopride". CNS Neuroscience & Therapeutics 14 (3): 248–62. 2008. doi:10.1111/j.1755-5949.2008.00047.x. PMID 18801115.
- ↑ "Current status of PET imaging in Huntington's disease". European Journal of Nuclear Medicine and Molecular Imaging 43 (6): 1171–82. June 2016. doi:10.1007/s00259-016-3324-6. PMID 26899245.
External links
- Dopamine+antagonists at the US National Library of Medicine Medical Subject Headings (MeSH)
 |