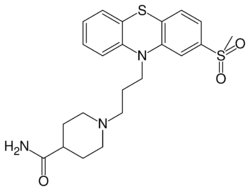
Chemistry:Metopimazine
 | |
| Clinical data | |
|---|---|
| Trade names | Vogalen, Vogalene |
| Other names | EXP-999; RP-9965; NG-101 |
| AHFS/Drugs.com | International Drug Names |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C22H27N3O3S2 |
| Molar mass | 445.60 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Metopimazine (INN, USAN, BAN), sold under the brand names Vogalen and Vogalene, is an antiemetic of the phenothiazine group which is used to treat nausea and vomiting.[1][2][3][4][5][6] It is marketed in Europe, Canada , and South America.[2][5] As of August 2020, metopimazine has been repurposed and is additionally under development for use in the United States for the treatment of gastroparesis.[6][5]
Metopimazine has antidopaminergic, antihistamine, and anticholinergic activity.[7] However, it has also been described as a highly potent and selective dopamine D2 and D3 receptor antagonist.[5] The D2 receptor antagonism of metopimazine is thought to underlie its antiemetic and gastroprokinetic effects.[5] It is said to not readily cross the blood–brain barrier and hence to have peripheral selectivity, in contrast to metoclopramide but similarly to domperidone.[5] Unlike domperidone however, metopimazine shows no hERG inhibition and hence is expected to have a more favorable cardiovascular profile.[5] In contrast to metoclopramide, metopimazine does not interact with serotonin 5-HT3 and 5-HT4 receptors.[5]
Medical uses
Metopimazine is an approved prescription drug in France under the brand name Vogalene® [8] that has been used for the treatment of nausea and vomiting.[9] Vogalene® is available under different forms, including 15 mg capsules, 7.5 mg orally disintegrating tablets, 5 mg suppository, 0.1% oral liquid, and a 10 mg/mL intravenous (IV) solution approved for the prevention of chemotherapy-induced nausea and vomiting.[10] Metopimazine is also an over-the-counter medication available in pharmacies in France (Vogalib®, 7.5 mg orally disintegrating tablets).[11] The approved dose is 30 mg per day. Most adult prescriptions are for seasonal gastroenteritis or acute nausea and vomiting of various etiologies. The IV formulation is almost exclusively used to treat chemotherapy-induced nausea and vomiting in adults and children.[12]
Adverse effects
Generally, studies in chemotherapy-induced nausea and vomiting suggest that doses of metopimazine higher than approved for common nausea and vomiting conditions tend to be more efficacious while remaining safe and well tolerated. Numerous open-label and randomized, placebo-controlled efficacy studies involving oral administration (ranging from 7.5 mg/day for 4 days, to up to 45 mg/day for ~7–30 days, to 120 mg/day for 4 days) or IV administration (10 mg to 40 mg) of metopimazine have concluded that metopimazine is safe and well tolerated with no report of severe adverse events.[13][14][15][16][17][18][19][20][21] In a dose-ranging, open-label study in patients undergoing chemotherapy, metopimazine administered orally at 20, 30, 40, 50, or 60 mg every 4 hours (q4h) for 48 hours was used to determine its safety and tolerability. Metopimazine was determined to be safe at a dose of 30 mg administered 6 times daily (180 mg/day). The dose-limiting toxicity to metopimazine was moderate-to-severe dizziness caused by orthostatic hypotension, which was observed beginning at 40 mg every 4 hours for 48 hours. Other side effects were few and mild in severity. A single possibly drug-related extrapyramidal adverse event was observed in a patient in the 60 mg q4h or 360 mg daily dose group.[22] In a randomized, double-blind comparison of ondansetron versus ondansetron plus metopimazine as an antiemetic prophylaxis during platinum-based chemotherapy, metopimazine was administered by IV (24-hour continuous infusion) at 35 mg/m2 followed by 30 mg per orally (PO) 4 times a day (120 mg/day) for 4 days. Metopimazine plus ondansetron was more efficacious than ondansetron alone, and adverse reactions were mild and without significant differences between the two treatment groups. However, there was an asymptomatic decrease in standing blood pressure when patients received the combination antiemetic therapy.[19] In a randomized, double-blind study assessing the efficacy and safety of sublingual metopimazine compared to ondansetron in chemotherapy-induced delayed emesis, patients received either 45 mg/day of metopimazine (7.5 mg x 2 every 8 hours) or 16 mg/day of ondansetron (8 mg every 12 hours). Results showed that metopimazine was comparable in efficacy to ondansetron; however, the incidence of gastrointestinal disorders was significantly lower in the metopimazine group, particularly abdominal pain and constipation.[23]
Mechanism of action
Metopimazine, a phenothiazine derivative, is a potent D2/D3 dopamine receptor antagonist. Metopimazine has also shown adrenergic alpha1, histamine H1, serotonin 5HT2a antagonism.[10]
Pharmacokinetics
The pharmacokinetics (PK) profile of metopimazine has been reported as comparable between adults and children. The maximum plasma concentration (Cmax) of metopimazine is reached approximately 60 minutes after oral administration, and the elimination half-life is approximately two hours.[24] Metopimazine is rapidly metabolized to metopimazine acid (Tmax ~2 hours), its major metabolite in humans. Metopimazine is primarily metabolized by a liver amidase in humans and therefore present a low risk on drug-drug interaction.[25] Exposure is reduced by ~30% and 50% (area under the curve (AUC) and Cmax, respectively) when metopimazine is administered with food.[26][10]
The bioavailability of metopimazine in humans is low. A 10 mg dose of metopimazine was reported to have an absolute bioavailability under 20%.[26]
Research
Metopimazine mesylate (NG101), a novel formulation of metopimazine, is under clinical development for idiopathic gastroparesis in the United States.[27] Gastroparesis is a debilitating chronic gastrointestinal disorder characterized by delayed gastric emptying without evidence of mechanical obstruction. Symptoms include nausea, vomiting, early satiety, postprandial fullness, bloating, and upper abdominal pain.[28][29][30]
Synthesis

For the first step, 2-Methylthiophenothiazine [7643-08-5] (1) is protected by sequential reaction with sodium amide and acetic anhydride to give 1-[2-(Methylthio)-10H-phenothiazin-10-yl]ethanone [23503-69-7] (2). Oxidation with peracid proceeds preferentially on the more electron-rich alkyl thioether to give the sulfone. Upon hydrolysis of the acetate this affords 2-(methylsulfonyl)-10h-phenothiazine [23503-68-6] (3). Alkylation with 1-Bromo-3-chloropropane (4) gives 10-(3-chloropropyl)-2-methylsulfonylphenothiazine [40051-30-7] (5). Alkylation with piperidine-4-carboxamide (Isonipecotamide) [39546-32-2] (6) affords metopimazine (7).
References
- ↑ J. Elks, ed (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 817–. ISBN 978-1-4757-2085-3. OCLC 1058412474. https://books.google.com/books?id=0vXTBwAAQBAJ&pg=PA817.
- ↑ 2.0 2.1 Swiss Pharmaceutical Society (2000). Swiss Pharmaceutical Society. ed. Index Nominum 2000: International Drug Directory. Taylor & Francis. pp. 683–. ISBN 978-3-88763-075-1. https://books.google.com/books?id=5GpcTQD_L2oC&pg=PA683.
- ↑ Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. 6 December 2012. pp. 180–. ISBN 9789401144391. OCLC 1243535030. https://books.google.com/books?id=tsjrCAAAQBAJ&pg=PA180.
- ↑ "Chemotherapy-induced nausea and vomiting with special emphasis on metopimazine". Danish Medical Bulletin 45 (4): 412–422. September 1998. PMID 9777292.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 "Nausea and Vomiting in 2021: A Comprehensive Update". Journal of Clinical Gastroenterology 55 (4): 279–299. April 2021. doi:10.1097/MCG.0000000000001485. PMID 33471485.
- ↑ 6.0 6.1 "Metopimazine - Neurogastrx - AdisInsight". https://adisinsight.springer.com/drugs/800043679.
- ↑ "Antidopaminergic antiemetics and trauma-related hospitalization: A population-based self-controlled case series study". British Journal of Clinical Pharmacology 87 (3): 1303–1309. March 2021. doi:10.1111/bcp.14510. PMID 32737898.
- ↑ "Vogalene®" (in en). https://www.rxreasoner.com/drugs/vogalene.
- ↑ "Accueil - ANSM" (in fr). https://ansm.sante.fr/.
- ↑ 10.0 10.1 10.2 "Metopimazine" (in en). American Journal of Cancer 5 (2): 123–136. March 2006. doi:10.2165/00024669-200605020-00006. ISSN 1175-6357. https://link.springer.com/article/10.2165/00024669-200605020-00006.
- ↑ "Vogalib" (in en). https://www.rxreasoner.com/drugs/vogalib.
- ↑ Shirley, Matt (July 2021). "Netupitant/Palonosetron: A Review in Chemotherapy-Induced Nausea and Vomiting". Drugs 81 (11): 1331–1342. doi:10.1007/s40265-021-01558-2. ISSN 1179-1950. PMID 34292534.
- ↑ "[A new antiemetic: vogalen (metopimazine or 9965 RP)]". Laval Medical 38 (10): 901–907. December 1967. PMID 5596819.
- ↑ "[Therapeutic value of metopimazine as an antiemetic in cancerology]". La Presse Médicale 77 (24): 893. May 1969. PMID 5797645.
- ↑ "[Use of metopimazine in certain vomitings from central origin]". Therapeutique 47 (5): 469–471. May 1971. PMID 5314918.
- ↑ "The prevention of radiation sickness. Report of a double blind random clinical trial using prochlorperazine and metopimazine". Clinical Radiology 22 (4): 534–537. October 1971. doi:10.1016/s0009-9260(71)80130-7. PMID 4944444.
- ↑ "[Value of metopimazine (Vogalene) in the prevention and treatment of postoperative vomiting in ocular surgery. (Apropos of 100 cases)]". Archives d'Ophtalmologie et Revue Generale d'Ophtalmologie 32 (1): 63–68. January 1972. PMID 4261213.
- ↑ "[Double blind randomized trial of metopimazine: for postoperative nausea and vomiting after cholecystectomy]". Annales de l'Anesthesiologie Francaise 20 (2): 118–120. 1979. PMID 38705.
- ↑ 19.0 19.1 "Randomized, double-blind comparison of ondansetron versus ondansetron plus metopimazine as antiemetic prophylaxis during platinum-based chemotherapy in patients with cancer". Journal of Clinical Oncology 15 (4): 1690–1696. April 1997. doi:10.1200/JCO.1997.15.4.1690. PMID 9193370.
- ↑ "The efficacy of a combination of ondansetron, methylprednisolone and metopimazine in patients previously uncontrolled with a dual antiemetic treatment in cisplatin-based chemotherapy. The French Ondansetron Study Group". Annals of Oncology 8 (9): 887–892. September 1997. doi:10.1023/a:1008276412559. PMID 9358940.
- ↑ "Ondansetron plus metopimazine compared with ondansetron plus metopimazine plus prednisolone as antiemetic prophylaxis in patients receiving multiple cycles of moderately emetogenic chemotherapy". Journal of Clinical Oncology 19 (7): 2091–2097. April 2001. doi:10.1200/JCO.2001.19.7.2091. PMID 11283143.
- ↑ "Dose-finding study of oral metopimazine". Supportive Care in Cancer 5 (1): 38–43. January 1997. doi:10.1007/BF01681960. PMID 9010988.
- ↑ "A randomized, double-blind trial assessing the efficacy and safety of sublingual metopimazine and ondansetron in the prophylaxis of chemotherapy-induced delayed emesis". Anti-Cancer Drugs 17 (2): 217–224. February 2006. doi:10.1097/00001813-200602000-00014. PMID 16428941.
- ↑ "Pharmacokinetic study of metopimazine by oral route in children". Pharmacology Research & Perspectives 3 (3): e00130. June 2015. doi:10.1002/prp2.130. PMID 26171218.
- ↑ "Metopimazine is primarily metabolized by a liver amidase in humans". Pharmacology Research & Perspectives 10 (1): e00903. February 2022. doi:10.1002/prp2.903. PMID 34918875.
- ↑ 26.0 26.1 "The effect of food on serum concentrations of metopimazine". British Journal of Clinical Pharmacology 30 (2): 237–243. August 1990. doi:10.1111/j.1365-2125.1990.tb03770.x. PMID 2206785.
- ↑ "A Phase 2 Randomized, Double-blind, Placebo-Controlled, Parallel-Group Study, of the Safety and Efficacy of NG101 Administered Orally to Patients With Gastroparesis". clinicaltrials.gov. 4 November 2022. https://clinicaltrials.gov/ct2/show/NCT04303195.
- ↑ "ACG Clinical Guideline: Gastroparesis". The American Journal of Gastroenterology 117 (8): 1197–1220. August 2022. doi:10.14309/ajg.0000000000001874. PMID 35926490.
- ↑ "1079 NG101: A potent and selective dopamine D2 receptor antagonist as a potential alternative to metoclopramide and domperidone for the treatment of gastroparesis". Gastroenterology 150 (4): S214. 2016. doi:10.1016/S0016-5085(16)30794-6. https://www.gastrojournal.org/article/S0016-5085(16)30794-6/pdf?referrer=https%3A%2F%2Fwww.researchgate.net%2F.
- ↑ "Gastroparesis: A Review of Current Diagnosis and Treatment Options". Journal of Clinical Gastroenterology 49 (7): 550–558. August 2015. doi:10.1097/MCG.0000000000000320. PMID 25874755.
- ↑ Jacob RM, Robert JG, DE patent 1092476, issued 1960, assigned to Rhone Poulenc SA.
- ↑ "A simple and commercially viable process for improved yields of metopimazine, a dopamine D2-receptor antagonist.". Organic Process Research & Development 21 (5): 720–731. May 2017. doi:10.1021/acs.oprd.7b00052.
External links
- "Metopimazine". AdisInsight. Springer Nature Switzerland AG. https://adisinsight.springer.com/drugs/800043679.
 |
