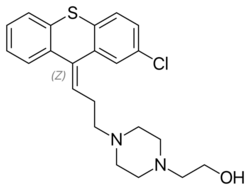
Chemistry:Zuclopenthixol
 | |
| Clinical data | |
|---|---|
| Trade names | Clopixol |
| AHFS/Drugs.com | International Drug Names |
| Pregnancy category |
|
| Routes of administration | Oral, IM |
| Drug class | Typical antipsychotic |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 49% (oral) |
| Protein binding | 98% |
| Metabolism | Liver (CYP2D6 and CYP3A4-mediated) |
| Elimination half-life | 20 hours (oral), 19 days (IM) |
| Excretion | Feces |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C22H25ClN2OS |
| Molar mass | 400.97 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Zuclopenthixol (brand names Cisordinol, Clopixol and others), also known as zuclopentixol, is a medication used to treat schizophrenia and other psychoses. It is classed, pharmacologically, as a typical antipsychotic. Chemically it is a thioxanthene. It is the cis-isomer of clopenthixol (Sordinol, Ciatyl).[2] Clopenthixol was introduced in 1961, while zuclopenthixol was introduced in 1978.
Zuclopenthixol is a D1 and D2 antagonist, α1-adrenergic and 5-HT2 antagonist.[3] While it is approved for use in Australia, Canada, Ireland, India, New Zealand, Singapore, South Africa and the UK it is not approved for use in the United States.[4][5]
Medical uses
Available forms
Zuclopenthixol is available in three major preparations:
- As zuclopenthixol decanoate (Clopixol Depot, Cisordinol Depot), it is a long-acting intramuscular injection. Its main use is as a long-acting injection given every two or three weeks to people with schizophrenia who have a poor compliance with medication and suffer frequent relapses of illness.[6] There is some evidence it may be more helpful in managing aggressive behaviour.[7]
- As zuclopenthixol acetate (Clopixol-Acuphase, Cisordinol-Acutard), it is a shorter-acting intramuscular injection used in the acute sedation of psychotic inpatients. The effect peaks at 48–72 hours providing 2–3 days of sedation.[8]
- As zuclopenthixol dihydrochloride (Clopixol, Cisordinol), it is a tablet used in the treatment of schizophrenia in those who are compliant with oral medication.[9]
It is also used in the treatment of acute bipolar mania.
Dosing
As a long-acting injection, zuclopenthixol decanoate comes in a 200 mg and 500 mg ampoule. Doses can vary from 50 mg weekly to the maximum licensed dose of 600 mg weekly. In general, the lowest effective dose to prevent relapse is preferred. The interval may be shorter as a patient starts on the medication before extending to 3 weekly intervals subsequently. The dose should be reviewed and reduced if side effects occur, though in the short-term an anticholinergic medication benztropine may be helpful for tremor and stiffness, while diazepam may be helpful for akathisia. 100 mg of zuclopenthixol decanoate is roughly equivalent to 20 mg of flupentixol decanoate or 12.5 mg of fluphenazine decanoate.
In acutely psychotic and agitated inpatients, 50 – 200 mg of zuclopenthixol acetate may be given for a calming effect over the subsequent three days, with a maximum dose of 400 mg in total to be given. As it is a long-acting medication, care must be taken not to give an excessive dose.
In oral form zuclopenthixol is available in 2, 10, 25 and 40 mg tablets, with a dose range of 20–60 mg daily.[10]
Side effects
Chronic administration of zuclopenthixol (30 mg/kg/day for two years) in rats resulted in small, but significant, increases in the incidence of thyroid parafollicular carcinomas and, in females, of mammary adenocarcinomas and of pancreatic islet cell adenomas and carcinomas. An increase in the incidence of mammary adenocarcinomas is a common finding for D2 antagonists which increase prolactin secretion when administered to rats. An increase in the incidence of pancreatic islet cell tumours has been observed for some other D2 antagonists. The physiological differences between rats and humans with regard to prolactin make the clinical significance of these findings unclear.
Withdrawal syndrome: Abrupt cessation of therapy may cause acute withdrawal symptoms (eg, nausea, vomiting, or insomnia). Symptoms usually begin in 1 to 4 days of withdrawal and subside within 1 to 2 weeks.[1][2]
Other permanent side effects are similar to many other typical antipsychotics, namely extrapyramidal symptoms as a result of dopamine blockade in subcortical areas of the brain. This may result in symptoms similar to those seen in Parkinson's disease and include a restlessness and inability to sit still known as akathisia, a slow tremor and stiffness of the limbs.[9] Zuclopenthixol is thought to be more sedating than the related flupentixol, though possibly less likely to induce extrapyramidal symptoms than other typical depots.[6] As with other dopamine antagonists, zuclopenthixol may sometimes elevate prolactin levels; this may occasionally result in amenorrhoea or galactorrhoea in severe cases. Neuroleptic malignant syndrome is a rare but potentially fatal side effect. Any unexpected deterioration in mental state with confusion and muscle stiffness should be seen by a physician.
Zuclopenthixol decanoate induces a transient dose-dependent sedation. However, if the patient is switched to maintenance treatment with zuclopenthixol decanoate from oral zuclopenthixol or from i.m. zuclopenthixol acetate the sedation will be no problem. Tolerance to the unspecific sedative effect develops rapidly.[11]
- Very common Adverse Effects (≥10% incidence) [12]
- Dry Mouth
- Somnolence
- Akathisia
- Hyperkinesia
- Hypokinesia
- Common (1%≤incidence≤10%) [12]
- Tachycardia
- Heart palpitations
- Vertigo
- Accommodation disorder
- Abnormal vision
- Salivary hypersecretion
- Constipation
- Vomiting
- Dyspepsia
- Diarrhoea
- Asthenia
- Fatigue
- Malaise
- Pain (at the injection site)
- Increased appetite
- Weight gain
- Myalgia
- Tremor
- Dystonia
- Hypertonia
- Dizziness
- Headache
- Paraesthesia
- Disturbance in attention
- Amnesia
- Abnormal gait
- Insomnia
- Depression
- Anxiety
- Abnormal dreams
- Agitation
- Decreased libido
- Nasal congestion
- Dyspnoea
- Hyperhidrosis
- Pruritus
- Uncommon (0.1%≤incidence≤1%)[12]
- Hyperacusis
- Tinnitus
- Mydriasis
- Abdominal pain
- Nausea
- Flatulence
- Thirst
- Injection site reaction
- Hypothermia
- Pyrexia
- Liver function test abnormal
- Decreased appetite
- Weight loss
- Muscle rigidity
- Trismus
- Torticollis
- Tardive dyskinesia
- Hyperreflexia
- Dyskinesia
- Parkinsonism
- Syncope
- Ataxia
- Speech disorder
- Hypotonia
- Convulsion
- Migraine
- Apathy
- Nightmares
- Libido increased
- Confused state
- Ejaculation failure
- Erectile dysfunction
- Female orgasmic disorder
- Vulvovaginal
- Dryness
- Rash
- Photosensitivity
- Pigmentation disorder
- Seborrhoea
- Dermatitis
- Purpura
- Hypotension
- Hot flush
- Rare (0.01%≤incidence≤0.1%)[12]
- Thrombocytopenia
- Neutropenia
- Leukopenia
- Agranulocytosis
- QT prolongation
- Hyperprolactinaemia
- Hypersensitivity
- Anaphylactic reaction
- Hyperglycaemia
- Glucose tolerance impaired
- Hyperlipidaemia
- Gynaecomastia
- Galactorrhoea
- Amenorrhoea
- Priapism
- Withdrawal symptoms
- Very rare (incidence<0.01%)[12]
- Cholestatic hepatitis
- Jaundice
- Neuroleptic malignant syndrome
- Venous thromboembolism
Pharmacology
Pharmacodynamics

Zuclopenthixol antagonises both dopamine D1 and D2 receptors, α1-adrenoceptors and 5-HT2 receptors with a high affinity, but has no affinity for muscarinic acetylcholine receptors. It weakly antagonises the histamine (H1) receptor but has no α2-adrenoceptor blocking activity [citation needed].
Evidence from in vitro work and clinical sources (i.e. therapeutic drug monitoring databases) suggests that both CYP2D6 and CYP3A4 play important roles in zuclopenthixol metabolism.[13]
Pharmacokinetics
History
Zuclopenthixol was introduced by Lundbeck in 1978.[14]
References
- ↑ "Clopixol (Zuclopenthixol Hydrochloride) Film-coated tablets". Australian Product Information. Australia: The Therapeutics Goods Administration. https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-05705-3.
- ↑ Sneader, Walter (2005). Drug discovery: a history. New York: Wiley. p. 410. ISBN 0-471-89980-1. https://books.google.com/books?id=Cb6BOkj9fK4C&pg=PA410. Retrieved 2020-10-07.
- ↑ "Pharmacological effects of a specific dopamine D-1 antagonist SCH 23390 in comparison with neuroleptics". Life Sciences 34 (16): 1529–1540. April 1984. doi:10.1016/0024-3205(84)90607-6. PMID 6144029.
- ↑ "Substance abuse and schizophrenia: pharmacotherapeutic intervention". Journal of Substance Abuse Treatment 34 (1): 61–71. January 2008. doi:10.1016/j.jsat.2007.01.008. PMID 17574793.
- ↑ Sweetman, Sean C., ed (2009). "Anxiolytic Sedatives Hypnotics and Antipsychotics". Martindale: The complete drug reference (36th ed.). London: Pharmaceutical Press. pp. 1040–1. ISBN 978-0-85369-840-1.
- ↑ 6.0 6.1 "Zuclopenthixol decanoate for schizophrenia". The Cochrane Database of Systematic Reviews (John Wiley and Sons, Ltd.) 1999 (2): CD001164. 1999. doi:10.1002/14651858.CD001164. PMID 10796607. PMC 7032616. http://www.cochrane.org/reviews/en/ab001164.html. Retrieved 2007-06-12.
- ↑ "Zuclopenthixol in adults with intellectual disabilities and aggressive behaviours". British Journal of Psychiatry 190 (5): 447–448. 2007. doi:10.1192/bjp.bp.105.016535. PMID 17470962.
- ↑ Lundbeck P/L (1991). "Clopixol Acuphase 50 mg/mL Injection Clopixol Acuphase 100 mg / 2 mL Injection". Lundbeck P/L. http://home.intekom.com/pharm/lundbeck/clopixac.html.
- ↑ 9.0 9.1 "Zuclopenthixol dihydrochloride for schizophrenia". The Cochrane Database of Systematic Reviews 2017 (11): CD005474. November 2017. doi:10.1002/14651858.CD005474.pub2. PMID 29144549.
- ↑ "Clopixol 2 mg film-coated tablets - Summary of Product Characteristics (SmPC) - (emc)". https://www.medicines.org.uk/emc/product/994/#gref.
- ↑ "Summary of Product Characteristics". https://www.hpra.ie/img/uploaded/swedocuments/LicenseSPC_PA0115-005-007_03062015110150.pdf.
- ↑ 12.0 12.1 12.2 12.3 12.4 "TGA eBS - Product and Consumer Medicine Information Licence". https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-05705-3.
- ↑ "Characterisation of zuclopenthixol metabolism by in vitro and therapeutic drug monitoring studies.". Acta Psychiatrica Scandinavica 122 (6): 445–453. 2010. doi:10.1111/j.1600-0447.2010.01619.x. PMID 20946203.
- ↑ William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia. Elsevier. pp. 1102–. ISBN 978-0-8155-1856-3. https://books.google.com/books?id=_J2ti4EkYpkC&pg=PA1102. Retrieved 27 September 2017.
 |
