Chemistry:Desloratadine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Clarinex, Aerius, Allex, others[1][2] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a602002 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth (tablets, solution) |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Rapidly absorbed |
| Protein binding | 83 to 87% |
| Metabolism | UGT2B10, CYP2C8 |
| Metabolites | 3-Hydroxydesloratadine |
| Onset of action | within 1 hour[3] |
| Elimination half-life | 27 hours[3] |
| Duration of action | up to 24 hours[3] |
| Excretion | 40% as conjugated metabolites into urine Similar amount into the feces |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
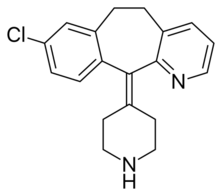
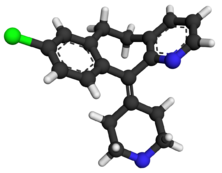
| Formula | C19H19ClN2 |
| Molar mass | 310.83 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Desloratadine (trade names Clarinex and Aerius) is a tricyclic H1 inverse agonist that is used to treat allergies. It is an active metabolite of loratadine.[3]
It was patented in 1984 and came into medical use in 2001.[4]
Medical uses
Desloratadine is used to treat allergic rhinitis, nasal congestion and chronic idiopathic urticaria (hives).[5] It is the major metabolite of loratadine and the two drugs are similar in safety and effectiveness.[5] Desloratadine is available in many dosage forms and under many trade names worldwide.[6]
An emerging indication for desloratadine is in the treatment of acne, as an inexpensive adjuvant to isotretinoin and possibly as maintenance therapy or monotherapy.[7][8]
Side effects
The most common side-effects are fatigue (1.2%[9]), dry mouth (3%[9]), and headache (0.6%[9]).[5]
Interactions
Co-administration with erythromycin, ketoconazole, azithromycin, fluoxetine or cimetidine resulted in elevated blood plasma concentrations of desloratadine and its metabolite 3-hydroxydesloratadine in studies. However, no clinically relevant changes were observed.[10][11]
Pharmacology
Pharmacodynamics
Desloratadine is a selective H1-antihistamine which functions as an inverse agonist at the histamine H1 receptor.[12]
At very high doses, is also an antagonist at various subtypes of the muscarinic acetylcholine receptors. This effect is not relevant for the drug's action at therapeutic doses.[13]
Pharmacokinetics
Desloratadine is well absorbed from the gut and reaches highest blood plasma concentrations after about three hours. In the bloodstream, 83 to 87% of the substance are bound to plasma proteins.[11]
Desloratadine is metabolized to 3-hydroxydesloratadine in a three-step sequence in normal metabolizers. First, n-glucuronidation of desloratadine by UGT2B10; then, 3-hydroxylation of desloratadine N-glucuronide by CYP2C8; and finally, a non-enzymatic deconjugation of 3-hydroxydesloratadine N-glucuronide.[14] Both desloratadine and 3-hydroxydesloratadine are eliminated via urine and feces with a half-life of 27 hours in normal metabolizers.[11][15]
It exhibits only peripheral activity since it does not readily cross the blood–brain barrier; hence, it does not normally cause drowsiness because it does not readily enter the central nervous system.[16]
Desloratadine does not have a strong effect on a number of tested enzymes in the cytochrome P450 system. It was found to weakly inhibit CYP2B6, CYP2D6, and CYP3A4/CYP3A5, and not to inhibit CYP1A2, CYP2C8, CYP2C9, or CYP2C19. Desloratadine was found to be a potent and relatively selective inhibitor of UGT2B10, a weak to moderate inhibitor of UGT2B17, UGT1A10, and UGT2B4, and not to inhibit UGT1A1, UGT1A3, UGT1A4, UGT1A6, UGT1A9, UGT2B7, UGT2B15, UGT1A7, and UGT1A8.[14]
Pharmacogenomics
2% of Caucasian people and 18% of people from African descent are desloratadine poor metabolizers. In these people, the drug reaches threefold highest plasma concentrations six to seven hours after intake, and has a half-life of about 89 hours. However, the safety profile for these subjects is not worse than for extensive (normal) metabolizers.[11][15]
See also
References
- ↑ "Desloratadine: an update of its efficacy in the management of allergic disorders". Drugs 63 (19): 2051–2077. April 7, 2003. doi:10.2165/00003495-200363190-00010. PMID 12962522.
- ↑ "Allex EPAR". https://www.ema.europa.eu/en/medicines/human/EPAR/allex.
- ↑ 3.0 3.1 3.2 3.3 "Antihistamines". Clinical Immunology. Elsevier. 2008. pp. 1317–1329. doi:10.1016/b978-0-323-04404-2.10089-2. ISBN 9780323044042. "Desloratadine is a metabolite of loratadine. The onset of action is within 1 hour. Peak serum concentrations of desloratadine appear 3 hours after dosing. The mean elimination half-life of desloratadine is 27 hours and that of its metabolite is 36 hours. The consumption of food does not interfere with the absorption of desloratadine. Wheal inhibition is detected 1 hour after administration and may last 24 hours."
- ↑ Analogue-based Drug Discovery. John Wiley & Sons. 2006. p. 549. ISBN 9783527607495. https://books.google.com/books?id=FjKfqkaKkAAC&pg=PA549.
- ↑ 5.0 5.1 5.2 "Desloratadine for allergic rhinitis". American Family Physician 68 (10): 2015–2016. November 2003. PMID 14655812. http://www.aafp.org/afp/20031115/steps.html. Retrieved 2005-08-01.
- ↑ Drugs.com Desloratadine entry at drugs.com international Page accessed May 4, 2015
- ↑ "Effect of antihistamine as an adjuvant treatment of isotretinoin in acne: a randomized, controlled comparative study". Journal of the European Academy of Dermatology and Venereology 28 (12): 1654–1660. December 2014. doi:10.1111/jdv.12403. PMID 25081735.
- ↑ "Top Ten List of Clinical Pearls in the Treatment of Acne Vulgaris". Dermatologic Clinics 34 (2): 147–157. April 2016. doi:10.1016/j.det.2015.11.008. PMID 27015774.
- ↑ 9.0 9.1 9.2 "Safety evaluation of desloratadine in allergic rhinitis". Expert Opinion on Drug Safety (Informa Healthcare) 12 (3): 445–453. May 2013. doi:10.1517/14740338.2013.788148. PMID 23574541.
- ↑ "Clarinex: Prescribing Information". U.S. Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/021165s017,021300s014,021312s015,021563s003lbl.pdf.
- ↑ 11.0 11.1 11.2 11.3 "Aerius: EPAR – Product Information". European Medicines Agency. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000313/WC500025540.pdf.
- ↑ "Antihistaminic, anti-inflammatory, and antiallergic properties of the nonsedating second-generation antihistamine desloratadine: a review of the evidence". The World Allergy Organization Journal 4 (2): 47–53. February 2011. doi:10.1097/WOX.0b013e3182093e19. PMID 23268457.
- ↑ "Aerius: EPAR – Scientific Discussion". European Medicines Agency. 2006-04-03. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Scientific_Discussion/human/000313/WC500022748.pdf.
- ↑ 14.0 14.1 "Further Characterization of the Metabolism of Desloratadine and Its Cytochrome P450 and UDP-glucuronosyltransferase Inhibition Potential: Identification of Desloratadine as a Relatively Selective UGT2B10 Inhibitor". Drug Metabolism and Disposition 43 (9): 1294–1302. September 2015. doi:10.1124/dmd.115.065011. PMID 26135009.
- ↑ 15.0 15.1 Drugs.com: Desloratadine Monograph.
- ↑ "Sedation with "non-sedating" antihistamines: four prescription-event monitoring studies in general practice". BMJ 320 (7243): 1184–1186. April 2000. doi:10.1136/bmj.320.7243.1184. PMID 10784544.
External links
- "Desloratadine". Drug Information Portal. U.S. National Library of Medicine. https://druginfo.nlm.nih.gov/drugportal/name/desloratadine.
 |


