Chemistry:4-Hydroxyamphetamine
Hydroxyamphetamine, also known as 4-hydroxyamphetamine or norpholedrine and sold under the brand names Paredrine and Paremyd among others, is a sympathomimetic medication used in eye drops to dilate the pupil for eye examinations.[1][2][3][4]
Hydroxyamfetamine acts as a norepinephrine releasing agent and hence is an indirectly acting sympathomimetic.[5][6] It is a substituted phenethylamine and amphetamine.[4]
Hydroxyamphetamine appeared to remain marketed only in the Czech Republic as of 2004.[3]
Medical uses
Hydroxyamphetamine is used in eye drops to dilate the pupil (a process called mydriasis) so that the back of the eye can be examined. This is a diagnostic test for Horner's syndrome. Patients with Horner's syndrome exhibit anisocoria brought about by lesions on the nerves that connect to the nasociliary branch of the ophthalmic nerve.[7] Application of hydroxyamphetamine to the eye can indicate whether the lesion is preganglionic or postganglionic based on the pupil's response. If the pupil dilates, the lesion is preganglionic. If the pupil does not dilate, the lesion is postganglionic.[7]
Hydroxyamphetamine has some limitations to its use as a diagnostic tool. If it is intended as an immediate follow up to another mydriatic drug (cocaine or apraclonidine), then the patient must wait anywhere from a day to a week before hydroxyamphetamine can be administered.[8][5] It also has the tendency to falsely localize lesions. False localization can arise in cases of acute onset; in cases where a postganglionic lesion is present, but the nerve still responds to residual norepinephrine; or in cases in which unrelated nerve damage masks the presence of a preganglionic lesion.[7][8]
Available forms
Hydroxyamphetamine is a component of two controlled (prescription only), name-brand ophthalmic mydriatics: Paredrine and Paremyd. Paredrine consists of a 1% solution of hydroxyamphetamine hydrobromide[9]: 543 while Paremyd consists of a combination of 1% hydroxyamphetamine hydrobromide and 0.25% tropicamide.[10]
Pharmacology
Pharmacodynamics
Hydroxyamphetamine acts as an indirect sympathomimetic and induces the release of norepinephrine which leads to mydriasis (pupil dilation).[5][6]
It has also been found to act as a serotonin releasing agent.[11] The drug produces the head-twitch response, a behavioral proxy of psychedelic effects, when it is given by intracerebroventricular injection in animals.[11] This effect is blocked by the serotonin receptor antagonists cyproheptadine and dimethothiazine, by the serotonin reuptake inhibitor fluoxetine, and by the serotonin synthesis inhibitor para-chlorophenylalanine (PCPA).[11] These findings suggest that hydroxyamphetamine-induced head twitches are due to activation of the serotonin 5-HT2A receptor and that they are mediated by induction of serotonin release as opposed to direct agonism of the serotonin 5-HT2A receptor.[11] Although hydroxyamphetamine produces the head-twitch response in animals, serotonin releasing agents are not necessarily hallucinogenic in humans, and hence their induction of head twitches in animals has been considered a false positive for psychedelic effects.[12][13][14]
It additionally decreases metabolism of serotonin and certain other monoamines by inhibiting the activity of monoamine oxidases (MAOs), particularly type A (MAO-A). The inhibition of MAO-A prevents metabolism of serotonin and catecholamines in the presynaptic terminal, and thus increases the amount of neurotransmitters available for release into the synaptic cleft.[11]
Like amphetamine, hydroxyamphetamine is an agonist of human TAAR1.[15]
Pharmacokinetics
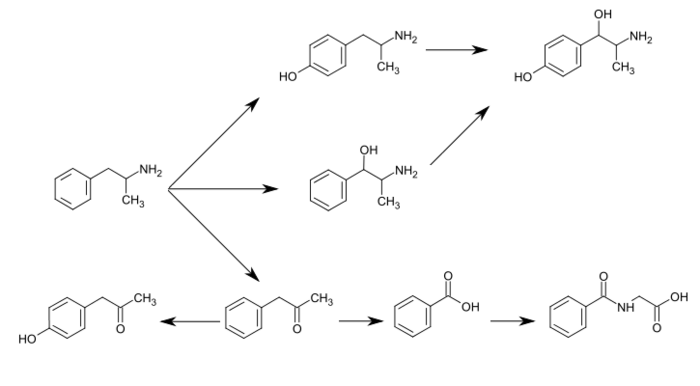
Hydroxyamphetamine is a major metabolite of amphetamine and a minor metabolite of methamphetamine. In humans, amphetamine is metabolized to hydroxyamphetamine by CYP2D6, which is a member of the cytochrome P450 superfamily and is found in the liver.[16][17] 4-Hydroxyamphetamine is then metabolized by dopamine β-hydroxylase into 4-hydroxynorephedrine or eliminated in the urine.[6]
Metabolic pathways of amphetamine in humans[sources 1]
|
Chemistry
Hydroxyamphetamine, also known as 4-hydroxy-α-methylphenethylamine, 4-hydroxyamphetamine, or α-methyltyramine, is a substituted phenethylamine and amphetamine derivative. It is the 4-hydroxylated analogue of amphetamine, the N-demethylated analogue of pholedrine (4-hydroxy-N-methylamphetamine), and the α-methylated analogue of tyramine (4-hydroxyphenethylamine). Other analogues include α-methyldopamine, corbadrine (levonordefrin; α-methylnorepinephrine), and dioxifedrine (α-methylepinephrine).
It has a predicted log P of 0.58 to 1.4.[29][4][30]
Hydroxyamphetamine is used pharmaceutically as the hydrobromide salt.[1]
History
Hydroxyamphetamine was first synthesized by 1910.[1]
In the 1990s, the trade name rights, patents, and new drug applications (NDAs) for Paredrine and Paremyd were exchanged among a few different manufacturers after a shortage of the raw material required for their production, which caused both drugs to be indefinitely removed from the market.[31] Around 1997, Akorn, Inc., obtained the rights to both Paredrine and Paremyd,[32] and in 2002, the company reintroduced Paremyd to the market as a fast acting ophthalmic mydriatic agent.[10][33][34]
In 2004, hydroxyamphetamine appeared to remain marketed only in the Czech Republic.[3]
Society and culture
Names
Hydroxyamphetamine is the generic name of the drug and its BAN and DCF, while hydroxyamfetamine is its INN.[1][2][3] In the case of the hydrobromide salt, its generic name is hydroxyamphetamine hydrobromide and this is its USAN.[1][2][3] It is also known by synonyms including methyltyramine, norpholedrine, and oxamphetamine.[1][2][3][29] The drug is sold under brand names including Paredrine, Paredrinex, Paremyd, Pedrolon, and Mycadrine.[1][3]
Other drugs
4-Hydroxyamphetamine is also a metabolite of amphetamine and certain other amphetamines.[2]
Notes
- ↑ 4-Hydroxyamphetamine has been shown to be metabolized into 4-hydroxynorephedrine by dopamine beta-hydroxylase (DBH) in vitro and it is presumed to be metabolized similarly in vivo.[19][24] Evidence from studies that measured the effect of serum DBH concentrations on 4-hydroxyamphetamine metabolism in humans suggests that a different enzyme may mediate the conversion of 4-hydroxyamphetamine to 4-hydroxynorephedrine;[24][26] however, other evidence from animal studies suggests that this reaction is catalyzed by DBH in synaptic vesicles within noradrenergic neurons in the brain.[27][28]
Reference notes
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer US. 2014. p. 74. ISBN 978-1-4757-2085-3. https://books.google.com/books?id=0vXTBwAAQBAJ&pg=PA74. Retrieved 30 August 2024.
- ↑ 2.0 2.1 2.2 2.3 2.4 Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Netherlands. 2012. p. 90. ISBN 978-94-011-4439-1. https://books.google.com/books?id=tsjrCAAAQBAJ&pg=PA90. Retrieved 30 August 2024.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Schweizerischer Apotheker-Verein (2004). Index Nominum: International Drug Directory. Medpharm Scientific Publishers. p. 609. ISBN 978-3-88763-101-7. https://books.google.com/books?id=EgeuA47Ocm4C&pg=PA609. Retrieved 30 August 2024.
- ↑ 4.0 4.1 4.2 "Hydroxyamphetamine: Uses, Interactions, Mechanism of Action". 30 January 1992. https://go.drugbank.com/drugs/DB09352.
- ↑ 5.0 5.1 5.2 "Diagnostic pharmacology of the pupil". Clinical Neuropharmacology 8 (1): 27–37. 1985. doi:10.1097/00002826-198503000-00003. PMID 3884149.
- ↑ 6.0 6.1 6.2 "Pathways of metabolism of amphetamine and related compounds". Life Sciences 22 (5): 363–372. February 1978. doi:10.1016/0024-3205(78)90282-5. PMID 347211.
- ↑ 7.0 7.1 7.2 "Horner syndrome". Current Opinion in Ophthalmology 14 (6): 357–363. December 2003. doi:10.1097/00055735-200312000-00007. PMID 14615640.
- ↑ 8.0 8.1 "Adult Horner's syndrome: a combined clinical, pharmacological, and imaging algorithm". Eye 27 (3): 291–298. March 2013. doi:10.1038/eye.2012.281. PMID 23370415.
- ↑ "The Pupils and Accommodation.". Neuro-ophthalmology. Philadelphia, PA: Lippincott, Williams, & Wilkins. 1999. ISBN 978-0781717298.
- ↑ 10.0 10.1 "Hydroxyamphetamine Hydrobromide; Tropicamide". Orange Book: Approved Drug Products with Therapeutic Equivalence Evaluations. http://www.accessdata.fda.gov/scripts/cder/ob/docs/obdetail.cfm?Appl_No=019261&TABLE1=OB_Rx.
- ↑ 11.0 11.1 11.2 11.3 11.4 "Monoamine oxidase and head-twitch response in mice. Mechanisms of alpha-methylated substrate derivatives". Neurotoxicology 25 (1–2): 223–232. January 2004. doi:10.1016/S0161-813X(03)00101-3. PMID 14697897. Bibcode: 2004NeuTx..25..223N.
- ↑ "Effect of Hallucinogens on Unconditioned Behavior". Behavioral Neurobiology of Psychedelic Drugs. Current Topics in Behavioral Neurosciences. 36. Berlin, Heidelberg: Springer Berlin Heidelberg. 2018. pp. 159–199. doi:10.1007/7854_2016_466. ISBN 978-3-662-55878-2. "Amphetamine and methamphetamine, which act primarily by increasing carrier-mediated release of dopamine and norepinephrine, do not provoke head twitches (Corne and Pickering 1967; Silva and Calil 1975; Yamamoto and Ueki 1975; Jacobs et al. 1976; Bedard and Pycock 1977; Halberstadt and Geyer 2013). By contrast, the 5-HT releasing drugs fenfluramine and p-chloroamphetamine (PCA) do produce a robust HTR (Singleton and Marsden 1981; Darmani 1998a). Fenfluramine and PCA are thought to act indirectly, by increasing carrier-mediated release of 5-HT, because the response can be blocked by inhibition of the 5-HT transporter (Balsara et al. 1986; Darmani 1998a) or by depletion of 5-HT (Singleton and Marsden 1981; Balsara et al. 1986). [...] Because indirect 5-HT agonists such as fenfluramine, PCA, and 5-HTP are not hallucinogenic (Van Praag et al. 1971; Brauer et al. 1996; Turner et al. 2006), their effects on HTR can potentially be classified as false-positive responses."
- ↑ "Correlation between the potency of hallucinogens in the mouse head-twitch response assay and their behavioral and subjective effects in other species". Neuropharmacology 167. May 2020. doi:10.1016/j.neuropharm.2019.107933. PMID 31917152. "Indirect 5-HT2A agonists such as fenfluramine, p-chloroamphetamine (PCA), and 5-hydroxytryptophan (5-HTP) induce head twitches in rodents (Corne et al. 1963; Singleton and Marsden 1981; Darmani 1998) but do not act as hallucinogens in humans (van Praag et al. 1971; Brauer et al. 1996; Turner et al. 2006), However, overdoses of compounds that increase serotonin (5-HT) release can result in 5-HT syndrome, which sometimes includes hallucinations (Birmes et al. 2003; Evans and Sebastian 2007).".
- ↑ "Molecular and Medical Aspects of Psychedelics". Int J Mol Sci 25 (1): 241. December 2023. doi:10.3390/ijms25010241. PMID 38203411. "While some false positives have been identified, such as fenfluramine, p-chloroamphetamine, and 5-hydroxytryptophan, the test predominantly exhibits specificity for 5-HT2A receptor agonists [15].".
- ↑ "Trace amine-associated receptor 1 is a stereoselective binding site for compounds in the amphetamine class". Bioorganic & Medicinal Chemistry 19 (23): 7044–7048. December 2011. doi:10.1016/j.bmc.2011.10.007. PMID 22037049.
- ↑ "Pharmacokinetic and pharmacodynamic drug interactions in the treatment of attention-deficit hyperactivity disorder". Clinical Pharmacokinetics 40 (10): 753–772. 2001. doi:10.2165/00003088-200140100-00004. PMID 11707061.
- ↑ "Monoaminergic drugs: general pharmacology". Pharmacology & Therapeutics B 2 (1): 185–218. 1976. doi:10.1016/0306-039x(76)90030-1. PMID 817330.
- ↑ "Adderall XR Prescribing Information". United States Food and Drug Administration. Shire US Inc. December 2013. pp. 12–13. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/021303s026lbl.pdf. Retrieved 30 December 2013.
- ↑ 19.0 19.1 Glennon RA (2013). Foye's principles of medicinal chemistry (7th ed.). Philadelphia, USA: Wolters Kluwer Health/Lippincott Williams & Wilkins. pp. 646–648. ISBN 9781609133450. "The simplest unsubstituted phenylisopropylamine, 1-phenyl-2-aminopropane, or amphetamine, serves as a common structural template for hallucinogens and psychostimulants. Amphetamine produces central stimulant, anorectic, and sympathomimetic actions, and it is the prototype member of this class (39). ... The phase 1 metabolism of amphetamine analogs is catalyzed by two systems: cytochrome P450 and flavin monooxygenase. ... Amphetamine can also undergo aromatic hydroxylation to p-hydroxyamphetamine. ... Subsequent oxidation at the benzylic position by DA β-hydroxylase affords p-hydroxynorephedrine. Alternatively, direct oxidation of amphetamine by DA β-hydroxylase can afford norephedrine."
- ↑ Taylor KB (January 1974). "Dopamine-beta-hydroxylase. Stereochemical course of the reaction". Journal of Biological Chemistry 249 (2): 454–458. PMID 4809526. http://www.jbc.org/content/249/2/454.full.pdf. Retrieved 6 November 2014. "Dopamine-β-hydroxylase catalyzed the removal of the pro-R hydrogen atom and the production of 1-norephedrine, (2S,1R)-2-amino-1-hydroxyl-1-phenylpropane, from d-amphetamine.".
- ↑ "Mammalian flavin-containing monooxygenases: structure/function, genetic polymorphisms and role in drug metabolism". Pharmacology & Therapeutics 106 (3): 357–387. June 2005. doi:10.1016/j.pharmthera.2005.01.001. PMID 15922018.
Table 5: N-containing drugs and xenobiotics oxygenated by FMO - ↑ "N-oxygenation of amphetamine and methamphetamine by the human flavin-containing monooxygenase (form 3): role in bioactivation and detoxication". Journal of Pharmacology and Experimental Therapeutics 288 (3): 1251–1260. March 1999. PMID 10027866.
- ↑ "Simultaneous determination of amphetamine and one of its metabolites by HPLC with electrochemical detection". Journal of Pharmaceutical and Biomedical Analysis 30 (2): 247–255. September 2002. doi:10.1016/S0731-7085(02)00330-8. PMID 12191709.
- ↑ 24.0 24.1 24.2 "Dopamine-beta-oxidase activity in man, using hydroxyamphetamine as substrate". British Journal of Pharmacology and Chemotherapy 20: 278–284. April 1963. doi:10.1111/j.1476-5381.1963.tb01467.x. PMID 13977820. "Hydroxyamphetamine was administered orally to five human subjects ... Since conversion of hydroxyamphetamine to hydroxynorephedrine occurs in vitro by the action of dopamine-β-oxidase, a simple method is suggested for measuring the activity of this enzyme and the effect of its inhibitors in man. ... The lack of effect of administration of neomycin to one patient indicates that the hydroxylation occurs in body tissues. ... a major portion of the β-hydroxylation of hydroxyamphetamine occurs in non-adrenal tissue. Unfortunately, at the present time one cannot be completely certain that the hydroxylation of hydroxyamphetamine in vivo is accomplished by the same enzyme which converts dopamine to noradrenaline.".
- ↑ "Glycine conjugation: importance in metabolism, the role of glycine N-acyltransferase, and factors that influence interindividual variation". Expert Opinion on Drug Metabolism & Toxicology 9 (9): 1139–1153. September 2013. doi:10.1517/17425255.2013.796929. PMID 23650932. "Figure 1. Glycine conjugation of benzoic acid. The glycine conjugation pathway consists of two steps. First benzoate is ligated to CoASH to form the high-energy benzoyl-CoA thioester. This reaction is catalyzed by the HXM-A and HXM-B medium-chain acid:CoA ligases and requires energy in the form of ATP. ... The benzoyl-CoA is then conjugated to glycine by GLYAT to form hippuric acid, releasing CoASH. In addition to the factors listed in the boxes, the levels of ATP, CoASH, and glycine may influence the overall rate of the glycine conjugation pathway.".
- ↑ "Human serum dopamine-β-hydroxylase. Relationship to hypertension and sympathetic activity". Circulation Research 32 (5): 594–599. May 1973. doi:10.1161/01.RES.32.5.594. PMID 4713201. "The biologic significance of the different levels of serum DβH activity was studied in two ways. First, in vivo ability to β-hydroxylate the synthetic substrate hydroxyamphetamine was compared in two subjects with low serum DβH activity and two subjects with average activity. ... In one study, hydroxyamphetamine (Paredrine), a synthetic substrate for DβH, was administered to subjects with either low or average levels of serum DβH activity. The percent of the drug hydroxylated to hydroxynorephedrine was comparable in all subjects (6.5-9.62) (Table 3).".
- ↑ "Formation of p-hydroxynorephedrine in brain following intraventricular administration of p-hydroxyamphetamine". Neuropharmacology 13 (12): 1187–1190. December 1974. doi:10.1016/0028-3908(74)90069-0. PMID 4457764. "In species where aromatic hydroxylation of amphetamine is the major metabolic pathway, p-hydroxyamphetamine (POH) and p-hydroxynorephedrine (PHN) may contribute to the pharmacological profile of the parent drug. ... The location of the p-hydroxylation and β-hydroxylation reactions is important in species where aromatic hydroxylation of amphetamine is the predominant pathway of metabolism. Following systemic administration of amphetamine to rats, POH has been found in urine and in plasma.
The observed lack of a significant accumulation of PHN in brain following the intraventricular administration of (+)-amphetamine and the formation of appreciable amounts of PHN from (+)-POH in brain tissue in vivo supports the view that the aromatic hydroxylation of amphetamine following its systemic administration occurs predominantly in the periphery, and that POH is then transported through the blood-brain barrier, taken up by noradrenergic neurones in brain where (+)-POH is converted in the storage vesicles by dopamine β-hydroxylase to PHN.". - ↑ "Neurochemical effects of amphetamine metabolites on central dopaminergic and serotonergic systems". Journal of Pharmacology and Experimental Therapeutics 251 (3): 901–908. December 1989. PMID 2600821. "The metabolism of p-OHA to p-OHNor is well documented and dopamine-β hydroxylase present in noradrenergic neurons could easily convert p-OHA to p-OHNor after intraventricular administration.".
- ↑ 29.0 29.1 "4-(2-Aminopropyl)phenol". https://pubchem.ncbi.nlm.nih.gov/compound/3651.
- ↑ "C9H13NO". 30 August 2024. https://www.chemspider.com/Chemical-Structure.3525.html.
- ↑ "Akorn Acquires Paredrine - Specialty Ophthalmic Diagnostic Product From Pharmics, Inc.". Akorn press release. March 24, 1999. http://www.thefreelibrary.com/Akorn+Acquires+Paredrine+-+Specialty+Ophthalmic+Diagnostic+Product...-a054197191.
- ↑ "Akorn press release". http://investors.akorn.com/phoenix.zhtml?c=78132&p=irol-newsArticle&ID=247062.
- ↑ "Akorn timeline". http://www.akorn.com/about_timeline.php.
- ↑ "Unique Mydriatic Returns: The combination formula fosters patient flow efficiencies". Ophthalmology Management. December 1, 2002. http://www.ophthalmologymanagement.com/articleviewer.aspx?articleID=85623.
External links
- p-Hydroxyamphetamine at the US National Library of Medicine Medical Subject Headings (MeSH)
 |