Biology:μ-opioid receptor
 Generic protein structure example |
The μ-opioid receptors (MOR) are a class of opioid receptors with a high affinity for enkephalins and beta-endorphin, but a low affinity for dynorphins. They are also referred to as μ(mu)-opioid peptide (MOP) receptors. The prototypical μ-opioid receptor agonist is morphine, the primary psychoactive alkaloid in opium and for which the receptor was named, with mu being the first letter of Morpheus, the compound's namesake in the original Greek. It is an inhibitory G-protein coupled receptor that activates the Gi alpha subunit, inhibiting adenylate cyclase activity, lowering cAMP levels.
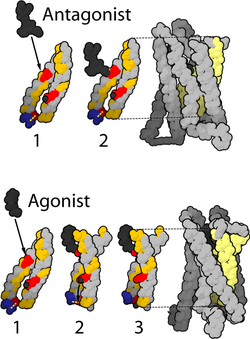
Structure
The structure of the inactive μ-opioid receptor has been determined with the antagonists β-FNA[2] and alvimopan.[3] Many structures of the active state are also available, with agonists including DAMGO,[4] β-endorphin,[5] fentanyl and morphine.[6] The structure with the agonist BU72 has the highest resolution,[7] but contains unexplained features that may be experimental artifacts.[8][9] This large body of evidence has enabled structure-based design of a new class of opioids with functional selectivity.[10]
Splice variants
Three variants of the μ-opioid receptor are well characterized, though reverse transcription polymerase chain reaction has identified up to 10 total splice variants in humans.[11][12][13]
| μ1 | More is known about the μ1 opioid receptor than the other variants. |
| μ2 | TRIMU 5 is a selective agonist of the μ2 receptor.[14] |
| μ3 | The μ3 variant was first described in 2003.[15] It is responsive to opiate alkaloids but not opioid peptides.[16] |
Location
They can exist either presynaptically or postsynaptically depending upon cell types.
The μ-opioid receptors exist mostly presynaptically in the periaqueductal gray region, and in the superficial dorsal horn of the spinal cord (specifically the substantia gelatinosa of Rolando). Other areas where they have been located include the external plexiform layer of the olfactory bulb, the nucleus accumbens, in several layers of the cerebral cortex, and in some of the nuclei of the amygdala, as well as the nucleus of the solitary tract.
Some MORs are also found in the intestinal tract. Activation of these receptors inhibits peristaltic action which causes constipation, a major side effect of μ agonists.[17]
Activation
MOR can mediate acute changes in neuronal excitability via suppression of presynaptic release of GABA. Activation of the MOR leads to different effects on dendritic spines depending upon the agonist, and may be an example of functional selectivity at the μ-receptor.[18] The physiological and pathological roles of these two distinct mechanisms remain to be clarified. Perhaps, both might be involved in opioid addiction and opioid-induced deficits in cognition.
Activation of the μ-opioid receptor by an agonist such as morphine causes analgesia, sedation, slightly reduced blood pressure, itching, nausea, euphoria, decreased respiration, miosis (constricted pupils), and decreased bowel motility often leading to constipation. Some of these effects, such as analgesia, sedation, euphoria, itching and decreased respiration, tend to lessen with continued use as tolerance develops. Miosis and reduced bowel motility tend to persist; little tolerance develops to these effects.
The canonical MOR1 isoform is responsible for morphine-induced analgesia, whereas the alternatively spliced MOR1D isoform (through heterodimerization with the gastrin-releasing peptide receptor) is required for morphine-induced itching.[19]
Deactivation
As with other G protein-coupled receptors, signalling by the μ-opioid receptor is terminated through several different mechanisms, which are upregulated with chronic use, leading to rapid tachyphylaxis.[20] The most important regulatory proteins for the MOR are the β-arrestins arrestin beta 1 and arrestin beta 2,[21][22][23] and the RGS proteins RGS4, RGS9-2, RGS14, and RGSZ2.[24][25]
Long-term or high-dose use of opioids may also lead to additional mechanisms of tolerance becoming involved. This includes downregulation of MOR gene expression, so the number of receptors presented on the cell surface is actually reduced, as opposed to the more short-term desensitisation induced by β-arrestins or RGS proteins.[26][27][28] Another long-term adaptation to opioid use can be upregulation of glutamate and other pathways in the brain which can exert an opioid-opposing effect, so reduce the effects of opioid drugs by altering downstream pathways, regardless of MOR activation.[29][30]
Tolerance and overdoses
Fatal opioid overdose typically occurs due to bradypnea, hypoxemia, and decreased cardiac output (hypotension occurs due to vasodilation, and bradycardia further contributes to decreased cardiac output).[31][32][33] A potentiation effect occurs when opioids are combined with ethanol, benzodiazepines, barbiturates, or other central depressants which can result in rapid loss of consciousness and an increased risk of fatal overdose.[31][32]
Substantial tolerance to respiratory depression develops quickly, and tolerant individuals can withstand larger doses.[34] However, tolerance to respiratory depression is quickly lost during withdrawal and may be completely reversed within a week. Many overdoses occur in people who return to their previous dose after having lost their tolerance following cessation of opioids. This puts addicts who receive medical treatment for opioid addiction at great risk of overdose when they are released, as they may be particularly vulnerable to relapse.
Less commonly, massive overdoses have been known to cause circulatory collapse from vasodilation and bradycardia.[35]
Opioid overdoses can be rapidly reversed through the use of opioid antagonists, naloxone being the most widely used example.[31] Opioid antagonists work by binding competitively to µ-opioid receptors and displacing opioid agonists. Additional doses of naloxone may be necessary and supportive care should be given to prevent hypoxic brain injury by monitoring vital signs.
Tramadol and tapentadol carry additional risks associated with their dual effects as SNRIs and can cause serotonin syndrome and seizures. Despite these risks, there is evidence to suggest that these drugs have a lower risk of respiratory depression compared to morphine.[36]
See also
- δ-opioid receptor
- κ-opioid receptor
References
- ↑ "Homology models of mu-opioid receptor with organic and inorganic cations at conserved aspartates in the second and third transmembrane domains". Archives of Biochemistry and Biophysics 375 (1): 31–49. March 2000. doi:10.1006/abbi.1999.1529. PMID 10683246.
- ↑ "Crystal structure of the µ-opioid receptor bound to a morphinan antagonist". Nature 485 (7398): 321–326. March 2012. doi:10.1038/nature10954. PMID 22437502. Bibcode: 2012Natur.485..321M.
- ↑ "Structure determination of inactive-state GPCRs with a universal nanobody". Nature Structural & Molecular Biology 29 (12): 1188–1195. December 2022. doi:10.1038/s41594-022-00859-8. PMID 36396979.
- ↑ "Structure of the µ-opioid receptor-Gi protein complex". Nature 558 (7711): 547–552. June 2018. doi:10.1038/s41586-018-0219-7. PMID 29899455. Bibcode: 2018Natur.558..547K.
- ↑ "Structures of the entire human opioid receptor family". Cell 186 (2): 413–427.e17. January 2023. doi:10.1016/j.cell.2022.12.026. PMID 36638794.
- ↑ "Molecular recognition of morphine and fentanyl by the human μ-opioid receptor". Cell 185 (23): 4361–4375.e19. November 2022. doi:10.1016/j.cell.2022.09.041. PMID 36368306.
- ↑ "Structural insights into µ-opioid receptor activation". Nature 524 (7565): 315–321. August 2015. doi:10.1038/nature14886. PMID 26245379. Bibcode: 2015Natur.524..315H.
- ↑ "The role of metal ions in G protein-coupled receptor signalling and drug discovery" (in en). WIREs Computational Molecular Science 12 (2): e1565. 2022. doi:10.1002/wcms.1565. ISSN 1759-0876.
- ↑ "Reanalysis of a μ opioid receptor crystal structure reveals a covalent adduct with BU72". BMC Biology 21 (1): 213. October 2023. doi:10.1186/s12915-023-01689-w. PMID 37817141.
- ↑ "Structure-based design of bitopic ligands for the µ-opioid receptor". Nature 613 (7945): 767–774. January 2023. doi:10.1038/s41586-022-05588-y. PMID 36450356. Bibcode: 2023Natur.613..767F.
- ↑ "Morphine-stimulated nitric oxide release in rabbit aqueous humor". Experimental Eye Research 84 (1): 185–190. January 2007. doi:10.1016/j.exer.2006.09.014. PMID 17094965.
- ↑ "Identification and characterization of six new alternatively spliced variants of the human mu opioid receptor gene, Oprm". Neuroscience 133 (1): 209–220. 2005. doi:10.1016/j.neuroscience.2004.12.033. PMID 15893644.
- ↑ "Alternatively spliced mu opioid receptor C termini impact the diverse actions of morphine". The Journal of Clinical Investigation 127 (4): 1561–1573. April 2017. doi:10.1172/JCI88760. PMID 28319053.
- ↑ "TRIMU-5, a mu 2-opioid receptor agonist, stimulates the hypothalamo-pituitary-adrenal axis". Pharmacology, Biochemistry, and Behavior 47 (4): 943–946. April 1994. doi:10.1016/0091-3057(94)90300-X. PMID 8029266.
- ↑ "Molecular identification and functional expression of mu 3, a novel alternatively spliced variant of the human mu opiate receptor gene". Journal of Immunology 170 (10): 5118–5123. May 2003. doi:10.4049/jimmunol.170.10.5118. PMID 12734358.
- ↑ "Endogenous morphine: a role in wellness medicine". Medical Science Monitor 10 (6): ED5. June 2004. PMID 15173675.
- ↑ "Opiate-induced constipation related to activation of small intestine opioid μ2-receptors". World Journal of Gastroenterology 18 (12): 1391–1396. March 2012. doi:10.3748/wjg.v18.i12.1391. PMID 22493554.
- ↑ "Mu-opioid receptors modulate the stability of dendritic spines". Proceedings of the National Academy of Sciences of the United States of America 102 (5): 1725–1730. February 2005. doi:10.1073/pnas.0406797102. PMID 15659552. Bibcode: 2005PNAS..102.1725L.
- ↑ "Unidirectional cross-activation of GRPR by MOR1D uncouples itch and analgesia induced by opioids". Cell 147 (2): 447–458. October 2011. doi:10.1016/j.cell.2011.08.043. PMID 22000021.*Lay summary in: "Researchers block morphine’s itchy side effect". October 13, 2011. http://news.wustl.edu/news/Pages/22805.aspx.
- ↑ "The role of mu opioid receptor desensitization and endocytosis in morphine tolerance and dependence". Current Opinion in Neurobiology 17 (5): 556–564. October 2007. doi:10.1016/j.conb.2007.10.004. PMID 18068348.
- ↑ "The role of opioid receptor internalization and beta-arrestins in the development of opioid tolerance". Anesthesia and Analgesia 101 (3): 728–734. September 2005. doi:10.1213/01.ANE.0000160588.32007.AD. PMID 16115983.
- ↑ "Tracking the opioid receptors on the way of desensitization". Cellular Signalling 18 (11): 1815–1833. November 2006. doi:10.1016/j.cellsig.2006.03.015. PMID 16750901.
- ↑ "Mechanisms of opioid-induced tolerance and hyperalgesia". Pain Management Nursing 8 (3): 113–121. September 2007. doi:10.1016/j.pmn.2007.02.004. PMID 17723928.
- ↑ "Morphine alters the selective association between mu-opioid receptors and specific RGS proteins in mouse periaqueductal gray matter". Neuropharmacology 48 (6): 853–868. May 2005. doi:10.1016/j.neuropharm.2005.01.004. PMID 15829256.
- ↑ "A role of RGS proteins in drug addiction". Biochemical Pharmacology 75 (1): 76–84. January 2008. doi:10.1016/j.bcp.2007.07.045. PMID 17880927.
- ↑ "The analgesic efficacy of fentanyl: relationship to tolerance and mu-opioid receptor regulation". Pharmacology, Biochemistry, and Behavior 91 (1): 115–120. November 2008. doi:10.1016/j.pbb.2008.06.019. PMID 18640146.
- ↑ "Morphine desensitization, internalization, and down-regulation of the mu opioid receptor is facilitated by serotonin 5-hydroxytryptamine2A receptor coactivation". Molecular Pharmacology 74 (5): 1278–1291. November 2008. doi:10.1124/mol.108.048272. PMID 18703670.
- ↑ "Regulation of mu-opioid receptors by cytokines". Frontiers in Bioscience 1 (1): 164–170. June 2009. doi:10.2741/e16. PMID 19482692.
- ↑ "Regulation of the extrinsic and intrinsic apoptotic pathways in the prefrontal cortex of short- and long-term human opiate abusers". Neuroscience 157 (1): 105–119. November 2008. doi:10.1016/j.neuroscience.2008.09.002. PMID 18834930.
- ↑ "Mechanisms underlying morphine analgesic tolerance and dependence". Frontiers in Bioscience 14 (14): 5260–5272. June 2009. doi:10.2741/3596. PMID 19482614.
- ↑ 31.0 31.1 31.2 Blok (2017). "Opioid toxicity". Clinical Key (Elsevier). https://www.elsevier.com/__data/assets/pdf_file/0010/545824/Opioid-toxicity-ClinicalKey.pdf.
- ↑ 32.0 32.1 "Sedation in the intensive care setting". Clinical Pharmacology 4 (53): 53–63. 2012. doi:10.2147/CPAA.S26582. PMID 23204873.
- ↑ "Acute and chronic effects of morphine on cardiovascular system and the baroreflexes sensitivity during severe increase in blood pressure in rats". ARYA Atherosclerosis 7 (3): 111–117. 2011. doi:10.1016/0277-9536(88)90399-1. PMID 22577457.
- ↑ "Tolerance to Opioid-Induced Respiratory Depression in Chronic High-Dose Opioid Users: A Model-Based Comparison With Opioid-Naïve Individuals". Clinical Pharmacology and Therapeutics 109 (3): 637–645. March 2021. doi:10.1002/cpt.2027. PMID 32865832.
- ↑ "Cardiovascular Complications of Opioid Use: JACC State-of-the-Art Review". Journal of the American College of Cardiology 77 (2): 205–223. January 2021. doi:10.1016/j.jacc.2020.11.002. PMID 33446314.
- ↑ "Efficacy and safety of tramadol versus morphine for moderate and severe postoperative pain with special regard to respiratory depression". Anesthesia and Analgesia 74 (4): 510–514. April 1992. doi:10.1213/00000539-199204000-00007. PMID 1554117.
External links
- "Opioid Receptors: μ". IUPHAR Database of Receptors and Ion Channels. International Union of Basic and Clinical Pharmacology. http://www.iuphar-db.org/GPCR/ReceptorDisplayForward?receptorID=2405.
- mu+Opioid+Receptor at the US National Library of Medicine Medical Subject Headings (MeSH)
- Human OPRM1 genome location and OPRM1 gene details page in the UCSC Genome Browser.
 |

