Chemistry:Furosemide
| File:Furosemide.svg | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /fjʊˈroʊsəˌmaɪd/ |
| Other names | Frusemide |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category |
|
| Routes of administration | by mouth, IV, IM |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 43–69% |
| Metabolism | liver and kidney glucuronidation |
| Onset of action | 30 to 60 min (PO), 5 min (IV)[1] |
| Elimination half-life | up to 100 minutes |
| Excretion | renal 66%, biliary 33% |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
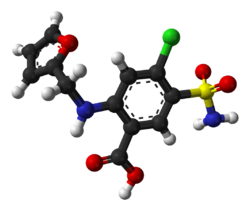
| Formula | C12H11ClN2O5S |
| Molar mass | 330.74 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
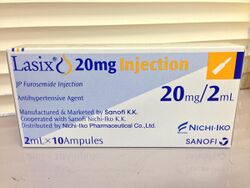
Furosemide, sold under the brand name Lasix among others, is a medication used to treat fluid build-up due to heart failure, liver scarring, or kidney disease.[1] It may also be used for the treatment of high blood pressure.[1] It can be taken by injection into a vein or by mouth.[1] When taken by mouth, it typically begins working within an hour, while intravenously, it typically begins working within five minutes.[1]
Common side effects include feeling lightheaded with standing, ringing in the ears, and sensitivity to light.[1] Potentially serious side effects include electrolyte abnormalities, low blood pressure, and hearing loss.[1] Blood tests are recommended regularly for those on treatment.[1] Furosemide is a type of loop diuretic that works by decreasing the reabsorption of sodium by the kidneys.[1]
Furosemide was patented in 1959 and approved for medical use in 1964.[2] It is on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system.[3] The wholesale price in the developing world is between US$0.004 and US$0.02 per day.[4] In the United States, it is available as a generic medication and costs about US$0.15 per day.[1] In 2017, it was the 17th most commonly prescribed medication in the United States, with more than 30 million prescriptions.[5][6] It is on the World Anti-Doping Agency's banned drug list due to concerns that it may mask other drugs.[7] It has also been used in race horses for the treatment and prevention of exercise-induced pulmonary hemorrhage.[8][9]
Medical uses
Furosemide is primarily used for the treatment of edema, but also in some cases of hypertension (where there is also kidney or heart impairment).[10] It is often viewed as a first-line agent in most people with edema caused by congestive heart failure.[1] Compared with furosemide, however, torsemide is associated with a lower risk of rehospitalization for heart failure and an improvement in New York Heart Association class of heart failure but no difference in the risk of death.[11][12] Torsemide may also be safer than furosemide.[13][14]
Furosemide is also used for liver cirrhosis, kidney impairment, nephrotic syndrome, in adjunct therapy for swelling of the brain or lungs where rapid diuresis is required (IV injection), and in the management of severe hypercalcemia in combination with adequate rehydration.[15]
Kidney disease
In chronic kidney diseases with hypoalbuminemia, it is used along with albumin to increase diuresis. It is also used along with albumin in nephrotic syndrome to reduce edema. [16]
Other information
- It is mainly excreted by tubular secretion in the kidney. In kidney impairment, clearance is reduced, increasing the risk of adverse effects.[1] Lower initial doses are recommended in older patients (to minimize side-effects) and high doses may be needed in kidney failure.[17] It can also cause kidney damage; this is mainly by loss of excessive fluid (i.e. dehydration), and is usually reversible.
- Furosemide acts within 1 hour of oral administration (after IV injection, the peak effect is within 30 minutes). Diuresis is usually complete within 6–8 hours of oral administration, but there is significant variation between individuals.[18]
Adverse effects
Furosemide also can lead to gout caused by hyperuricemia. Hyperglycemia is also a common side effect.
The tendency, as for all loop diuretics, to cause low serum potassium concentration (hypokalemia) has given rise to combination products, either with potassium or with the potassium-sparing diuretic amiloride (Co-amilofruse). Other electrolyte abnormalities that can result from furosemide use include hyponatremia, hypochloremia, hypomagnesemia, and hypocalcemia.[19]
In the treatment of heart failure, many studies have shown that the long-term use of furosemide can cause varying degrees of thiamine deficiency, so thiamine supplementation is also suggested.[20]
Although disputed,[21] it is considered ototoxic: "usually with large intravenous doses and rapid administration and in renal impairment".[22]
Other precautions include: nephrotoxicity, sulfonamide (sulfa) allergy, and increases free thyroid hormone effects with large doses.[23]
Interactions
Furosemide has potential interactions with these medications:[24]
- Aspirin and other salicylates
- Other diuretics (e.g. ethacrynic acid, hydrochlorothiazide)
- Synergistic effects with other antihypertensives (e.g. doxazosin)
- Sucralfate
Potentially hazardous interactions with other drugs:
- Analgesics: increased risk of kidney damage (nephrotoxicity) with nonsteroidal anti-inflammatory drugs; antagonism of diuretic effect with NSAIDs
- Antiarrhythmics: a risk of cardiac toxicity exists with antiarrhythmics if hypokalemia occurs; the effects of lidocaine and mexiletine are antagonized.
- Antibacterials: increased risk of ototoxicity with aminoglycosides, polymyxins and vancomycin; avoid concomitant use with lymecycline
- Antidepressants: increased risk of hypokalemia with reboxetine; enhanced hypotensive effect with MAOIs; increased risk of postural hypotension with tricyclic antidepressants
- Antiepileptics: increased risk of hyponatremia with carbamazepine
- Antifungals: increased risk of hypokalemia with amphotericin
- Antihypertensives: enhanced hypotensive effect; increased risk of first dose hypotensive effect with alpha-blockers; increased risk of ventricular arrhythmias with sotalol if hypokalemia occurs
- Antipsychotics: increased risk of ventricular arrhythmias with amisulpride, sertindole, or pimozide (avoid with pimozide) if hypokalemia occurs; enhanced hypotensive effect with phenothiazines
- Atomoxetine: hypokalemia increases risk of ventricular arrhythmias
- Cardiac glycosides: increased toxicity if hypokalemia occurs
- Cyclosporine: variable reports of increased nephrotoxicity, ototoxicity and hepatotoxicity
- Lithium: risk of toxicity.
Mechanism of action
Furosemide, like other loop diuretics, acts by inhibiting the luminal Na-K-Cl cotransporter in the thick ascending limb of the loop of Henle, by binding to the chloride transport channel, thus causing sodium, chloride, and potassium loss in urine.[25]
The action on the distal tubules is independent of any inhibitory effect on carbonic anhydrase or aldosterone; it also abolishes the corticomedullary osmotic gradient and blocks negative, as well as positive, free water clearance. Because of the large NaCl absorptive capacity of the loop of Henle, diuresis is not limited by development of acidosis, as it is with the carbonic anhydrase inhibitors.
Additionally, furosemide is a noncompetitive subtype-specific blocker of GABA-A receptors.[26][27][28] Furosemide has been reported to reversibly antagonize GABA-evoked currents of α6β2γ2 receptors at μM concentrations, but not α1β2γ2 receptors.[26][28] During development, the α6β2γ2 receptor increases in expression in cerebellar granule neurons, corresponding to increased sensitivity to furosemide.[27]
Pharmacokinetics
- Molecular weight (daltons) 330.7
- % Bioavailability 47-70%
- % Protein binding 91–99[31]
- Volume of distribution (L/kg) 0.07 – 0.2[32][33]
- Volume of distribution may be higher in patients with cirrhosis or nephrotic syndrome[32]
- Excretion
- Approximately 10% is metabolized by the liver in healthy individuals, but this percentage may be greater in individuals with severe kidney failure [33]
- Renal clearance (mL/min/kg) 2.0[32]
- Elimination half-life (hrs) 2[31]
- Time to peak concentration (hrs)
The pharmacokinetics of furosemide are apparently not significantly altered by food.[38]
No direct relationship has been found between furosemide concentration in the plasma and furosemide efficacy. Efficacy depends upon the concentration of furosemide in urine.[18]
Names
Furosemide is the INN and BAN.[39] The previous BAN was frusemide.
Brand names under which furosemide is marketed include: Aisemide, Apo-Furosemide, Beronald, Desdemin, Discoid, Diural, Diurapid, Dryptal, Durafurid, Edemid, Errolon, Eutensin, Flusapex, Frudix, Frusemide, Frusetic, Frusid, Fulsix, Fuluvamide, Furesis, Furix, Furo-Puren, Furon, Furosedon, Fusid.frusone, Hydro-rapid, Impugan, Katlex, Lasilix, Lasix, Lodix, Lowpston, Macasirool, Mirfat, Nicorol, Odemase, Oedemex, Profemin, Rosemide, Rusyde, Salix, Seguril, Teva-Furosemide, Trofurit, Uremide, and Urex.
Veterinary uses
The diuretic effects are put to use most commonly in horses to prevent bleeding during a race. Sometime in the early 1970s, furosemide's ability to prevent, or at least greatly reduce, the incidence of bleeding (exercise-induced pulmonary hemorrhage) by horses during races was discovered accidentally. In the United States of America, pursuant to the racing rules of most states, horses that bleed from the nostrils three times are permanently barred from racing. Clinical trials followed, and by decade's end, racing commissions in some states in the USA began legalizing its use on race horses. On September 1, 1995, New York became the last state in the United States to approve such use, after years of refusing to consider doing so. Some states allow its use for all racehorses; some allow it only for confirmed "bleeders". Its use for this purpose is still prohibited in many other countries.
Furosemide is also used in horses for pulmonary edema, congestive heart failure (in combination with other drugs), and allergic reactions. Although it increases circulation to the kidneys, it does not help kidney function, and is not recommended for kidney disease.
It is also used to treat congestive heart failure (pulmonary edema, pleural effusion, and/or ascites) in cats and dogs.[40] It can also be used in an attempt to promote urine production in anuric or oliguric acute kidney failure.
Horses
Furosemide is injected either intramuscularly or intravenously, usually 0.5-1.0 mg/kg twice/day, although less before a horse is raced. As with many diuretics, it can cause dehydration and electrolyte imbalance, including loss of potassium, calcium, sodium, and magnesium. Excessive use of furosemide will most likely lead to a metabolic alkalosis due to hypochloremia and hypokalemia. The drug should, therefore, not be used in horses that are dehydrated or experiencing kidney failure. It should be used with caution in horses with liver problems or electrolyte abnormalities. Overdose may lead to dehydration, change in drinking patterns and urination, seizures, gastrointestinal problems, kidney damage, lethargy, collapse, and coma.
Furosemide should be used with caution when combined with corticosteroids (as this increases the risk of electrolyte imbalance), aminoglycoside antibiotics (increases risk of kidney or ear damage), and trimethoprim sulfa (causes decreased platelet count). It may also cause interactions with anesthetics, so its use should be related to the veterinarian if the animal is going into surgery, and it decreases the kidneys' ability to excrete aspirin, so dosages will need to be adjusted if combined with that drug.
Furosemide may increase the risk of digoxin toxicity due to hypokalemia.
The drug is best not used during pregnancy or in a lactating mare, as it has been shown to be passed through the placenta and milk in studies with other species. It should not be used in horses with pituitary pars intermedia dysfunction (Cushings).
Furosemide is detectable in urine 36–72 hours following injection. Its use is restricted by most equestrian organizations.
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 "Furosemide". The American Society of Health-System Pharmacists. Archived from the original on 2015-11-19. https://web.archive.org/web/20151119161939/http://www.drugs.com/monograph/furosemide.html. Retrieved October 23, 2015.
- ↑ Fischer, Jnos; Ganellin, C. Robin (2006) (in en). Analogue-based Drug Discovery. John Wiley & Sons. p. 458. ISBN 9783527607495. https://books.google.ca/books?id=FjKfqkaKkAAC&pg=PA458.
- ↑ World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. 2019. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ "Furosemide". Archived from the original on 10 May 2017. https://web.archive.org/web/20170510104950/http://mshpriceguide.org/en/single-drug-information/?DMFId=363&searchYear=2014. Retrieved 24 October 2015.
- ↑ "The Top 300 of 2020". https://clincalc.com/DrugStats/Top300Drugs.aspx.
- ↑ "Furosemide - Drug Usage Statistics". 1 December 1981. https://clincalc.com/DrugStats/Drugs/Furosemide.
- ↑ "THE 2014 PROHIBITED LIST INTERNATIONAL STANDARD". 2014. p. 5. Archived from the original on 15 January 2016. https://web.archive.org/web/20160115033743/https://wada-main-prod.s3.amazonaws.com/resources/files/WADA-prohibited-list-2014-EN.pdf. Retrieved 24 October 2015.
- ↑ Sullivan, S; Hinchcliff, K (April 2015). "Update on exercise-induced pulmonary hemorrhage.". The Veterinary Clinics of North America. Equine Practice 31 (1): 187–98. doi:10.1016/j.cveq.2014.11.011. PMID 25770069.
- ↑ Hinchcliff, KW; Couetil, LL; Knight, PK; Morley, PS; Robinson, NE; Sweeney, CR; van Erck, E (2015). "Exercise induced pulmonary hemorrhage in horses: American College of Veterinary Internal Medicine consensus statement.". Journal of Veterinary Internal Medicine 29 (3): 743–58. doi:10.1111/jvim.12593. PMID 25996660.
- ↑ "Furosemide". The American Society of Health-System Pharmacists. Archived from the original on 17 March 2011. https://web.archive.org/web/20110317080203/http://www.drugs.com/monograph/furosemide.html. Retrieved 3 April 2011.
- ↑ "READY: relative efficacy of loop diuretics in patients with chronic systolic heart failure-a systematic review and network meta-analysis of randomised trials". Heart Fail Rev 24 (4): 461–472. March 2019. doi:10.1007/s10741-019-09771-8. PMID 30874955.
- ↑ "Torsemide versus furosemide and intermediate-term outcomes in patients with heart failure: an updated meta-analysis". J Cardiovasc Med (Hagerstown) 20 (6): 379–388. June 2019. doi:10.2459/JCM.0000000000000794. PMID 30950982.
- ↑ "Diuretics: a review and update". J. Cardiovasc. Pharmacol. Ther. 19 (1): 5–13. 2014. doi:10.1177/1074248413497257. PMID 24243991.
- ↑ "A reappraisal of loop diuretic choice in heart failure patients". Am. Heart J. 169 (3): 323–33. 2015. doi:10.1016/j.ahj.2014.12.009. PMID 25728721.
- ↑ Rossi S, ed (2004). Australian Medicines Handbook 2004 (5th ed.). Adelaide, S.A.: Australian Medicines Handbook Pty Ltd. ISBN 978-0-9578521-4-3. http://www.amh.net.au/.
- ↑ BMC Nephrol. 2012 Aug 29;13:92. doi: 10.1186/1471-2369-13-92.The added-up albumin enhances the diuretic effect of furosemide in patients with hypoalbuminemic chronic kidney disease: a randomized controlled study. Phakdeekitcharoen B1, Boonyawat K Ann Pharmacother. 2003 May;37(5):695-700. Combined furosemide and human albumin treatment for diuretic-resistant edema. Elwell RJ1, Spencer AP, Eisele G
- ↑ "British National Formulary". https://bnf.nice.org.uk/drug/furosemide.html#renalImpairment. Retrieved 9 November 2018.
- ↑ 18.0 18.1 18.2 Ponto, LL; Schoenwald, RD (May 1990). "Furosemide (frusemide). A pharmacokinetic/pharmacodynamic review (Part I).". Clinical Pharmacokinetics 18 (5): 381–408. doi:10.2165/00003088-199018050-00004. PMID 2185908.
- ↑ Oh, SW; Han, SY (June 2015). "Loop Diuretics in Clinical Practice.". Electrolyte & Blood Pressure 13 (1): 17–21. doi:10.5049/EBP.2015.13.1.17. PMID 26240596.
- ↑ Katta, N; Balla, S; Alpert, MA (July 2016). "Does Long-Term Furosemide Therapy Cause Thiamine Deficiency in Patients with Heart Failure? A Focused Review.". The American Journal of Medicine 129 (7): 753.e7–753.e11. doi:10.1016/j.amjmed.2016.01.037. PMID 26899752.
- ↑ "Use of furosemide and hearing loss in neonatal intensive care survivors". Am J Perinatol 21 (6): 329–32. 2004. doi:10.1055/s-2004-831887. PMID 15311369.
- ↑ BNF 45 March 2003
- ↑ "UpToDate". https://www.uptodate.com/contents/furosemide-drug-information?search=furosemide&source=search_result&selectedTitle=1~148&usage_type=panel&kp_tab=drug_general&display_rank=1#F174802.
- ↑ Brand name:Lasix - Generic name: Furosemide Prescription Drug Information, Side Effects - PDRHealth
- ↑ Dowd, Frank J; Johnson, Bart; Mariotti, Angelo (3 September 2016). Pharmacology and Therapeutics for Dentistry - E-Book. Elsevier Health Sciences. pp. 324–326. ISBN 9780323445955. https://books.google.com/books?id=6xT7DAAAQBAJ&pg=PA326. Retrieved 4 November 2017.
- ↑ 26.0 26.1 "Selective antagonist for the cerebellar granule cell-specific gamma-aminobutyric acid type A receptor". Mol. Pharmacology. 47 (2): 283–9. 1995. PMID 7870036.
- ↑ 27.0 27.1 "Developmental changes of inhibitory synaptic currents in cerebellar granule neurons: role of GABA(A) receptor alpha 6 subunit". J. Neurosci. 16 (11): 3630–40. 1996. doi:10.1523/JNEUROSCI.16-11-03630.1996. PMID 8642407.
- ↑ 28.0 28.1 "Functional characterization of human gamma-aminobutyric acidA receptors containing the alpha 4 subunit". Mol. Pharmacol. 50 (3): 670–8. 1996. PMID 8794909.
- ↑ AMA Department of Drugs: Drug Evaluations Subscription, American Medical Association, Chicago, IL, 1990.
- ↑ Knoben JE & Anderson PO (Eds): Handbook of Clinical Drug Data, 6th. Drug Intelligence Publications, Inc, Hamilton, IL, 1988.
- ↑ 31.0 31.1 31.2 31.3 Product Information: Lasix(R), furosemide. Aventis Pharmaceuticals, Bridgewater, NJ, 2004.
- ↑ 32.0 32.1 32.2 32.3 32.4 Gilman AG, Rall TW, Nies AS, et al (Eds): Goodman and Gilman's The Pharmacological Basis of Therapeutics, 8th. Pergamon Press, New York, NY, 1990.
- ↑ 33.0 33.1 33.2 33.3 33.4 Kelly, M. R.; Cutler, R. E.; Forrey, A. W.; Kimpel, B. M. (February 1974). "Pharmacokinetics of orally administered furosemide". Clinical Pharmacology and Therapeutics 15 (2): 178–186. doi:10.1002/cpt1974152178. ISSN 0009-9236. PMID 4812154.
- ↑ Verbeeck, R. K.; Patwardhan, R. V.; Villeneuve, J. P.; Wilkinson, G. R.; Branch, R. A. (June 1982). "Furosemide disposition in cirrhosis". Clinical Pharmacology and Therapeutics 31 (6): 719–725. doi:10.1038/clpt.1982.101. ISSN 0009-9236. PMID 7075120.
- ↑ Chaturvedi, P. R.; O'Donnell, J. P.; Nicholas, J. M.; Shoenthal, D. R.; Waters, D. H.; Gwilt, P. R. (March 1987). "Steady state absorption kinetics and pharmacodynamics of furosemide in congestive heart failure". International Journal of Clinical Pharmacology, Therapy, and Toxicology 25 (3): 123–128. ISSN 0174-4879. PMID 3557737.
- ↑ Brater, D.C. (1991). "Clinical Pharmacology of Loop Diuretics" (in en). Drugs 41 (Supplement 3): 14–22. doi:10.2165/00003495-199100413-00004. ISSN 0012-6667. PMID 1712712.
- ↑ Haegeli, Laurent; Brunner-La Rocca, Hans Peter; Wenk, Markus; Pfisterer, Matthias; Drewe, Jürgen; Krähenbühl, Stephan (December 2007). "Sublingual administration of furosemide: new application of an old drug". British Journal of Clinical Pharmacology 64 (6): 804–809. doi:10.1111/j.1365-2125.2007.03035.x. ISSN 1365-2125. PMID 17875188.
- ↑ AHFS Drug Information 2004. McEvoy GK, ed. Furosemide. American Society of Health-System Pharmacists; 2004: 2260-4.
- ↑ "Naming human medicines". Archived from the original on 2010-04-27. https://web.archive.org/web/20100427025454/http://www.mhra.gov.uk/Howweregulate/Medicines/Namingofmedicines/ChangestomedicinesnamesBANstorINNs/index.htm. Retrieved 2009-11-18.
- ↑ Kittleson, Mark; Kienle, Richard (1998). Small Animal Cardiovascular Medicine. ISBN 978-0-8151-5140-1. https://archive.org/details/smallanimalcardi0000kitt.
Further reading
- Aventis Pharma (1998). Lasix Approved Product Information. Lane Cove: Aventis Pharma Pty Ltd.
- Barbara Forney (2007). Understanding Equine Medications, Revised Edition (Horse Health Care Library). Eclipse Press. ISBN 978-1-58150-151-3.
External links
- "Furosemide". Drug Information Portal. U.S. National Library of Medicine. https://druginfo.nlm.nih.gov/drugportal/name/furosemide.
- Lasix and horse bleeding
 |
